![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
Describe life cycle of hepadnaviruses.
|
Virus binds receptor on hepatocyte
Enters, get uncoated, repaired into closed, circular covalent DNA (cccDNA)-->enters nucleus Serves as template for transcription (DNA-->RNA-->DNA in cytoplasm via reverse transcriptase); packaged and shipped into other cells Virus is very hard to get rid of! |
|
|
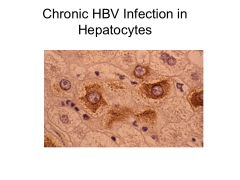
Main cause of HBV chronic carrier status.
Treatment? |
Maternal to fetal transmission of HBV
Provide neonate with passive immunity at birth (HBV Ab's) until immune system develops--then give HBV vaccine. |
|
|
Main complication of HBV.
|
Liver cancer
|
|
|
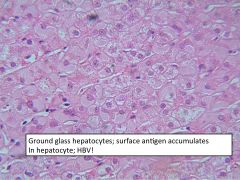
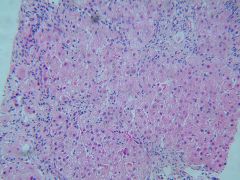
Low Level HBV:
Effects Concerns w/immunocompromised |
Low level HBV (AKA occult level HBV) = cause of chronic hepatitis and cirrhosis
Can reactivate w/immunosuppression-chemotx, transplantation (treat w/nucleoside analog to prevent viral DNA replication) Allows for viral persistance and infectivity--often co-exists w/HIV, HCV |
|
|
This HBV test may not detect low level HBV infection.
|
Anti-HBs (surface Ag)
|
|
|
How does the non-cytolytic pathway clear HBV?
When does this occur? |
Occurs early in infection (3-7 days)--NK cells etc release TNFalpha, IFNgamma to down-regulate viral replication.
|
|
|
How does the cytolytic pathway clear HBV?
When does this occur? |
Occurs late in infection (10-14 days), involves adaptive immunity
MHC I presentation on hepatocytes-->CD8+ and CD4+ responses; destroys infected hepatocytes |
|
|
How long does it take to develop anti-HBs?
|
1-6 months after infection--provides protective immunity from reinfection
98% of those infected w/HBV will clear the virus; 2% will be chronic carriers (most babies that are infected with it will be chronic carriers) |
|
|
Which treatments for chronic HBV exhibit the lowest antiviral resistance?
|
Tenofovir (PegIFN?)
Entecavir |
|
|
What percent of patients with HCV infection will become chronic carriers?
|
85%
|
|
|
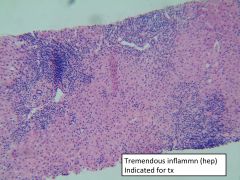
Risk factors for fibrosis in HCV.
|
Age
Males ALT (high ALT-->high risk) Inflammation Alcohol: even low level consumption! HIV |
|
|
Patients with _____ must have _____ before risk of hepatocarcinoma.
|
HCV: need cirrhosis before at risk of hepatocarcinoma
|
|
|
How does HAV differ from HBV/HCV?
|
-No chronic carrier state
-No cirrhosis |
|
|
HAV:
Diagnosis |
-Measure HAV IgM (not IgG)
-IgG just tells you whether you've had virus in the past -Positive IgM means acute infection |
|
|
This virus has reverse transcriptase activity.
|
HBV
|
|
|
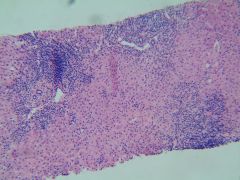
This virus requires liver biopsy to define clinical course.
|
HBV
|
|
|
This virus can be treated with nucleoside analogs.
|
HBV--note: nucleoside Rx effective but requires constant administration and mutations are a problem
|
|
|
HBV:
Treatment considerations |
Nucleoside Rx effective but requires constant administration and mutations are a problem
|
|
|
This hepatitis virus is a DNA virus.
|
HBV
|
|
|
This hepatitis virus is an RNA virus.
|
HCV
|
|
|
HCV:
Treatment |
IFNalpha + ribavirin
|
|
|
This virus is a major risk factor for hepatocarcinoma.
|
HCV
|
|
|
This hepatitis does not result in chronic hepatitis, cirrhosis, or hepatocarcinoma.
|
HAV
|
|
|
|
|
|
|
|
|

|
|
|
|
|
|
|
|
|
|

