![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
|
Compared to nucleated cells, what do RBC's look like metabolically?
|
No replication, DNA/RNA synthesis, Lipid heme protein synthesis, electron transport or TCA
90% of glycolysis and 10% of HMS |
|
|
O2 and CO2 transport are ____ and that matters in RBC's because....
|
passive
it doesn't use energy to transport these-- RBC's don't have much in energy production |
|
|
What do RBC's use their energy for?
|
Not O2/CO2 transport (passive)
Maintaining transmembrane gradients Maintaining Hb in ferrous (Fe2+) state. |
|
|
What is Met Hb?
How is it used? |
It's Hb that has a ferric iron.
Ferr"ick" gross Fe3+ is oxidized and can't work as a carrier. RBC's use energy to reduce these back to ferrous = ferr"us" (good for "us") Fe2+ |
|
|
What are the three ways to change Met Hb to Hb?
|
Met Hb reductase (enzymatic)
a secret minor enzyme that uses NADPH Ascorbic acid/Glutathione (non enzymatic) |
|
|
When might you purposefully change Hb to Met Hb?
|
during cyanide poisoning since CN goes after Fe3+
|
|
|
Met Hb Reductase
What does it need? |
NADH for the electrons
|
|
|
What is the disorder in which excessive amounts of Met Hb are in the blood?
What are the two forms of this we learned? |
methemoglobinemia
hereditary: NADH-Met Hb reductase deficiency acquired: chemicals (nitrites, quinones, peroxides) oxidize |
|
|
Describe different ROS.
|
O2 + ...
1e- = O2- superoxide 2e- = H2O2 hydrogen peroxide 3e- = OH + HO' (hydroxyl radical these free radicals are bad business |
|
|
Outline the formation of methemoglobin
|
Hb(Fe2+,O2)--> O2- + Hb(Fe3+)
Reversed with Met Hb reductase |
|
|
What do you do with ROS? Include intermediates and enzymes.
What makes this process sustainable? |
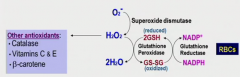
O2- --superoxide dismutase--> H2O2 (which is actually worse)
but + 2GSH --glutathione peroxidase--> 2H2O + GS-SG (oxidized glutathione) (RBC specific) To recycle GSH, HMS's NADPH regenerates GSH via glutathione reductase (RBC specific) Can also just use other antioxidants for H2O2 All of these are necessary- can't be missing any parts of this. |
|
|
What ROS related enzymes are specific to RBC?
Why is it specific to RBC? |
glutathione peroxidase (H2O2 + 2GSH -> 2H2O GS-SH) and glutathione reductase (recycles GS-SG to 2GSH using NADPH)
The oxidation potential is much higher in RBC since so much O2 always around. All cells combat ROS, but RBC especially. |
|
|
What causes necrosis during MI?
What other disorders did we learn about that's similar to this? |
The reprofusion of oxygenated blood causes excess ROS that ruin everything.
Homocysteinemia and homocystinuria (caused by loss of 5-MTHF or vit B6, folate, B12 deficiency) |
|
|
Why would supplementing cysteine in your diet help with oxidative stress?
|
It's a component of GSH
|
|
|
What is the mode of inheritance for G6PD deficiency?
What populations have high rates? |
X-linked recessive
Mediterranean Middle Eastern African |
|
|
What is the problem in G6PD deficiency?
What are the symptoms? |
G6P + NADP ---G6P dehydrogenase--> 6-phosphoglucate (goes to HMS) + NADPH
In deficiency: no NADPH(!) which is used to recycle glutathione via glutathione reductase -> high H2O2 levels (in the RBC only, so problems focal on RBC) Get Heinz bodies (Hb-s-s-Hb) and hemolytic anemia (Hb-s-s-membrane lipids) |
|
|
What would set off an episode in someone wtih Class III G6PD deficiency?
|
These are moderate cases: an acute situation like infection or a lot of fava beans would cause too many ROS for the moderately deficient enzyme.
|
|
|
What is an advantage of G6PD deficiency?
|
In malaria, the plasmodia invade RBC's, but when ROS levels go up, RBC can't cope and plasmodia die and cell dies-> selectively destroying infested RBC's only.
|

