![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Just draw out the overview of blood clot formation.
|

|
|
|
Role of platelets: ____ hemostasis. Platelets have an affinity for ___.
|
Primary
collagen |
|
|
How do platelets work?
|
injury causes exposed collagen fibers which platelets adhere to. Platelets activate and secrete: ADP and serotonin
|
|
|
What role does ADP play after activation by platelets?
What can inhibit this? |
platelets swell, and plasma membrane becomes sticky making a platelet plug.
Plavix |
|
|
What role does serotonin play after platelet secretion?
What inhibits this? |
increases plasma membrane phospholipase A2 which cleaves arachidonic acid from phospholipids --COX--> thromboxane A2 which vasoconstricts
COX is blocked by aspirin |
|
|
What happens in scurvy?
|
Vitamin C deficiency means collagen not properly formed causing bleeding problems.
|
|
|
Formation of ___ fibrin from ___ - this is the main chemical defense against blood loss.
|
insoluble
fibrinogen |
|
|
Fibrinogen is a major protein in ___, comprising __% of all proteins. Its ___like and its amino and carboxy termini have lots of ___ and ___ important for their ___ charges. These _noun__ _verb__ other fibrinogens to keep it ___ ___.
|
plasma. 7%.
rodlike with many Asp and Glu for negative charges poles repulse to keep free flowing |
|
|
How does fibrinogen make a soft clot?
|
fibrinogen --thrombin--> fibrin (lost charged ends)
Now they spontaneously assemble in fibrin polymer (insoluble red [trapped RBC's] clot, so-called soft clot) |
|
|
How do you make a hard clot?
|
thrombin activates Factor XIII --> XIIIa aka transglutaminase by proteolytic cleavage
XIIIa covalently links lys and glu residues of fibrins to form amide crosslinks |
|
|
Where does thrombin come from?
What all is required? |
prothrombin (zymogen of thrombin) has several γ-carboxylglutamates on the amino terminal end
glu --vit K--> γ-carboxyglu prothrombin -> thrombin requires phospholipid Factor V Factor Xa Ca2+ |
|
|
Activation of all blood coagulation zymogens occurs on a surface which has net ___-charged ___ derived from platelets or damaged tissues.
These are found exclusively ___________ which matters because.... |
negatively-charged phospholipids
on the cytoplasmic side of lipid bilayers (PI PS PG only on inner leaflet) which is why prothrombin does NOT bind to normal, intact RBC's or endothelial cells |
|
|
Draw the complex that activates the blood coagulation zymogens
|

Note the negative PL on the inner membrane are exposed due to cell death and lysis.
Ca2+ is chelated by γ-carboxylglutamates of prothrombin and available as a target to cleave by V and Xa |
|
|
What is a chelator?
Where are we seeing this? |
a molecule that binds extremely tightly to divalent cations
γ-carboxyglu chelates Ca2+ so all the clotting factors can sit on the membrane |
|
|
So outline the extrinsic coagulation pathway
|
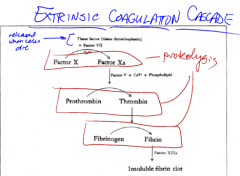
protein tissue factors (thromboplastin) released when cells die. Activates factor X, and then as described above.
|
|
|
After a factor like thromboplastin is added, what is a normal clotting time?
|
12s
|
|
|
What is the intrinsic pathway?
Outline it. |
This cascade amplifies minute quantities of clotting factors early in the secquence to make great amounts of end products (thrombin and fibrin).
|
|
|
How long does the intrinsic coagulation pathway take?
|

2-3 minutes.
|
|
|
What is wrong in "classic" hemophilia?
|
Factor VII missing.
|
|
|
How do we confine coagulation to the place of damage?
|
Natural clotting inhibitors like antithrombin III
Clotting factors bind tightly to the clot to limit sites of action The t1/2 of factors are short and they're removed by hepatocytes rapidly The concentration of factors decreases by dilution of flowing blood (shearing forces) |
|
|
What is vitamin K's role in clotting?
|
It is an essential cofactor for γ glutamyl carboxylase (only in LIVER).
These γ-carboxyglu are in prothrombin as well as X, IX and VII. Without the γ-carboxyglu, these cannot bind calcium. So deficiency/inhibition of vit K leads to decrease in proper factors and higher coagulation times. |
|
|
What are different anticoagulants used in different situations?
|
In vitro use calcium chelators like EDTA, F-, citrate, oxalate because they bind Ca tightly
In vivo: dicumarol or warfarin (coumadin) are vit K analogues Also, heparin: short-term anticoagulant- activates anti-thrombin III |
|
|
Describe heparin.
Where is it naturally found? |
Big polysaccharide with many sulfate and carboxyl groups (glucuronic acid)
Found in metachromatic granules of mast cells that line the endothelium of blood vessels |

