![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Consequences of Left Sided Heart Failure
|
Pulmonary congestion and Edema
|
|
|
Consequences of Right-sided Heart Failure (4)
|
Increase in Systemic Venous pressure
-Pitting Edema -Ascites -Nutmeg liver -Pleural effusions |
|
|
What usually causes right sided heart failure?
|
Left-sided heart failure
|
|
|
What is Cor Pulmonale?
|
Pure right-sided heart failure due to chronic severe Pulmonary Hypertension
|
|
|
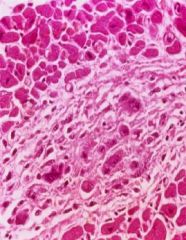
Histological cells of Left-sided Heart Failure
|
Hemosiderin-laden Macrophages = Heart Failure cells
|
|
|
Liver congestion in Right Sided Heart Failure first occurs in this part
|
Central Vein = centrilobular necrosis
|
|
|
Define Myocardial Ischemia
|
an imbalance between the supply (perfusion) and demand of oxygen in the heart
|
|
|
Causes 90% of Myocardial Ischemia
|
reduction in coronary blood flow due to Atherosclerotic coronary artery obstruction
|
|
|
An increased Myocardial metabolism could be due to this disease
|
Hyperthyroidism -> tachycardia -> increased O2 demand
|
|
|
Example of decreased oxygen transport resulting in Myocardial Ischemia
|
Anemia
|
|
|
How is the dominant artery chosen?
|
the one that gives rise to teh Posterior Descending artery
-90% is the Right Coronary |
|
|
Risk factors for Ischemic Heart Disease
|
HAS LIPIDS
Hereditary Age Sex (Male>Female) Lipidemia Increased weight Pressure (Hypertension) Inactivity Diabetes Smoking |
|
|
Ischemic Heart Disease can present in these 4 ways
|
1. Angina Pectoris
2. Chronic Ischemic Heart Disease 3. Myocardial Infarct 4. Sudden Cardian Death |
|
|
Fixed obstruction occludes what percent of the lumen?
|
>75%
|
|
|
Soft atheromas are highly likely to result in what type of angina?
|
Unstable Angina
|
|
|
Most common form of angina
|
Stable
|
|
|
Stable angina is induced by __1__ and is caused by __2__
|
1. exercise
2. ischemia due to atherosclerotic narrowing of coronary arteries |
|
|
Stable Angina is relieved by these 2 things
|
Rest
Nitroglycerin |
|
|
Explain Prinzmetal Angina (3)
|
-Coronary Artery SPASM at REST
- ST elevation = transmural ischemia -Nitroglycerin helps |
|
|
What characterizes Unstable (Crescendo) Angina
|
pain that is becoming more and more severe and is precipitated by less and less effort
|
|
|
What usually causes Unstable Angina
|
coronary atheromas that are prone to rupture
|
|
|
What is Myocardial Akinesis
|
where there are no contractions
|
|
|
What is Myocardial Dyskinasis
|
Where there are Abnormals contractions
|
|
|
3 consequences of Plaque rupture in Coronary Arteries
|
1. Healing
2. Embolism in downstream smaller mural vessels 3. Thrombosis -> unstable angina |
|
|
Parts of the Heart that the Right Coronary Artery supplies
|

1. posterior wall of LV
2. Posterior part of Septum 3. RV |
|
|
Parts of the Heart that the LAD supplies
|
1. anterior LV
2. Anterior septum |
|
|
Parts of heart that Left Circumflex artery supplies
|
lateral wall of LV
|
|
|
Frequencies of Coronary Artery obstruction
|
LAD = 50%
RCA = 30% LCX = 20% |
|
|
Part of heart that is most susceptible to damage when principal blood flow is compromised (Hypotension)
|
Subendocardium (blood flows thru layers from outside to in)
|
|
|
Most coronary artery blood flow occurs during ventricular __________
|
diastole
|
|
|
Loss that occurs within seconds of Cardiac Ischemia
|
ATP
|
|
|
This is dimished in <2 minutes with Cardiac Ischemia
|
Contractility
|
|
|
50% ATP depletion occurs within _____
|
10 minutes
|
|
|
90% ATP depletion occurs within ______
|
40 minutes
|
|
|
Irreversible Cell injury occurs within _________
|
20-40 minutes
|
|
|
Microvascular injury (endothelial damage of small terminal vessels) occurs after ________
|
1 hour
|
|
|
MI pathology:
4-24 hours = 1 1-2 days = 2 3-5 days = 3 5-7 days = 4 2-4 wks = 5 5-8 wks = 6 |
1. mottling or no apparent gross changes
2. pale-yellow, cell necrosis, PMN's 3. central yellow, red rim, necrosis peaks 4. mottled yellow-red, Macrophages 5. red-gray, granulation tissue, fibroblasts 6. scarring; collagen |
|
|
When are the chances of Ventricular rupture the greatest after an MI
|
during the first week b/c collagen has not been put down yet
|
|
|
Characteristics of Transmural MI (4)
|
1. Q wave abnormality
2. Coronary Occlusion 3. limited to an ANATOMIC area 4. Epicarditis can occur |
|
|
Characteristics of Subendocardial MI (4)
|
1. non-Q wave
2. Hypoperfusion 3. Circumferential 4. No Epicarditis |
|
|
Irreversible injury of Ischemic Myocytes occurs first in this zone
|
Subendocardial zone
|
|
|
Preferred biomarker for diagnosing MI. Why?
|
Troponin I
-more specific for myocardial tissue -increase in blood within 2-4 hours -last for 7-10 days |
|
|
Characteristics of CK-MB
|
1. elevated at 2-4 hours
2. lasts 72 hours (3 days) |
|
|
After MI's, do most people have complications or not?
|
Complications arise in 80%
|
|
|
Most common complication after MI
|
Arrhythmia
|
|
|
What would cause an Infarct extension?
|
Retrograde movement of a thrombus
|
|
|
3 Types of Myocardial Rupture and their consequences
|
1. Ventricle Free wall rupture -> hemopericardium -> Cardiac Tamponade -> death
2. Ventricle Septum -> L to R shunt -> RV failure, Pulmonary HTN 3. Papillary Muscle rupture -> mitral regurgitation |
|
|
When does free-wall rupture most frequently occur?
|
3-7 days post-MI = early complication
|
|
|
When do Ventricular Aneurysms typically occur?
|
Several Weeks-Months post-MI = Late Complication
|
|
|
The Lumen of Ventricular Aneurysms often contains?
|
Mural Thrombi
|
|
|
Rupture of the Septum causing L-to-R shunting is an early or late complication?
|
Early (3-7 days)
|
|
|
Papillary Muscle ruptures causes...
|
Mitral Valve Insuffiency
- Systolic Murmur -Left-sided failure -Pulmonary edema |
|
|
3 treatments for Coronary Thrombosis
|
1. Thrombolytic Enzymes (Plasminogen Activator)
2. Coronary Angioplasty 3. Coronary artery bypass graft |
|
|
Rheumatic Fever:
-Median age = 1 -Where common? = 2 -Immune response to: 3 |
1. 10 yoa
2. underdeveloped countries 3. S. pyogenes (Group A, beta-hemolytic) |
|
|
Type of S. pyogenes infection that Acute Rheumatic Fever follows
|
Pharyngitis
|
|
|
Explain how S. pyogenes causes RF
|
S. pyogenes elicits an Immune response againsts its M protein that reacts with SELF
|
|
|
Most common manifestations of RF (2)
|
1. Joint pain
2. Carditis |
|
|
Major Criteria for RF
|
1. Carditis
2. Polyarthritis 3. Chorea 4. Erythema Marginatum 5. Subcutaneous Nodules |
|
|
4 minor criteria for RF
|
1. Previous history of RF
2. Fever 3. Lab findings 4. EKG (prolonged PR) |
|
|
Criteria that must be met to Diagnose someone with RF
|
2 major, 1 minor
or 1 major, 2 minor |
|
|
Most common cause of death in Acute RF
|
Myocarditis
|
|
|
What are Aschoff Bodies?
|
granulomas that consist of:
-central area of fibrinoid necrosis -surrounding M0 and lymphocytes -M0 have "owl-eye" appearance |
|
|
Type of Carditis that Acute RF causes
|
Pancarditis = effects the whole heart
|
|
|
RF Pericarditis has this appearance
|
"bread and butter"
|
|
|
Endocarditic Valve involvement in RF
|
Mitral > Aortic > Tricuspid
|
|
|
Are the verrucous lesions(fibrin vegetations) in RF sterile or septic?
|
Sterile
|
|
|
Chronic Endocarditis from RF results in ________
|
Dystrophic Calcification -> Stenosis
|
|
|
Valvular Heart Disease can result in these 2 things
|
Valvular Stenosis
Valvular Insufficiency |
|
|
Mitral Stenosis murmur
|
Diastolic
-opening snap -mid-diastolic rumbling |
|
|
Consequences of Mitral Stenosis
|
1. dilated/hypertrophy of L. Atrium
2. Pulmonary congestion 3. RVH |
|
|
Mitral Insufficiency murmur
|
Systolic murmur
|
|
|
Consequences of Mitral Insufficiency
|
1. LA dilation/hypertrophy
2. Pulmonary congestion 3. RVH 4. *LVH* b/c it is receiving more blood |
|
|
Most common stenosis of all Valvular abnormalities
|
Aortic Stenosis
|
|
|
Aortic Stenosis does not allow the outflow of blood from the LV into the Aorta during ________
|
Systole
|
|
|
Consequence of Aortic Stenosis
|
1.LVH
2. low peripheral arterial pressure |
|
|
Aortic Stenosis murmur
|
high-pitched Systolic murmur
|
|
|
Most common cause of Mitral Stenosis
|
Rheumatic Fever
|
|
|
Most common cause of Mitral Insufficiency
|
Mitral Valve prolapse
-endocarditis and rupture -or dysfxn of papillary muscle |
|
|
Most common cause of Aortic Stenosis
|
Calcification due to old age
(or a congenital Bicuspid Aortic Valve) |
|
|
Aortic insufficiency is due to .........
|
dilation of ascending aorta due Hypertension or Old Age
|
|
|
Mnemonic for most common Congenital Heart Diseases
|
VA-PATENT
-VSD -ASD -Patent ductus ateriosus -Aortic Stenosis -Tetralogy of Fallot -Endocardial cushion defect -Narrowing of Aorta (Coarctation) -Transposition of great vessels |

