![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
Symptoms of:
1. Bacterial conjunctivitis |

• often one eye affected, followed by both eyes affected a day or so later
• purulent discharge • gritty feeling • generalized redness |
|
|
Name at least 10 causes of red eye
|
1-3: conjunctivitis
4-6. Patchy red spots: episcleritis, scleritis, subconjunctival haemorrhage 7-8. uveitis, keratitis 9. acute closed angle glaucoma 10. trauma, smog, dust 11. pterygium 12. inward turning eyelashes (entropion) |
|
|
Symptoms of:
Viral conjunctivitis |

Usually in both eyes
Watery discharge Gritty feeling Generalised redness Often with cough and cold symptoms |
|
|
Symptoms of:
Allergic conjunctivitis |

Both eyes
Watery discharge Itchy Generalised redness, but tends to be redder near the eyelid May also have rhinitis, and a personal or family history of atopy Can be seasonal |
|
|
Symptoms of:
Subconjunctival haemorrhage |

A segment (or even the whole ) of the sclera will appear bright red
May be a history of coughing, straining or lifting, or asphyxia, or may be spontaneous No pain, resolves in 10-14 days |
|
|
Symptoms of:
Acute closed-angle glaucoma |

Fast onset
Characteristically occurs in the evening Iris may appear cloudy and sclera is red Blurred vision, halos around lights Vomiting, which may be severe and distract from actual eye problem Severe pain (therefore unlikely to present to community pharmacy) |
|
|
Symptoms of:
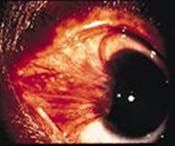
Episcleritis (inflammation of the epislcera, which is between the sclera and conjunctiva) |

A segment of the eye appears red and "vein-y", unlike subconjuctival haemorrhage
A dull ache is sometimes present Usually in young women, self-limiting, clears in 6-8 weeks |
|
|
Symptoms of:
Scleritis |
• Looks like episcleritis but much less common and much more painful
• Often associated with autoimmune disease |
|
|
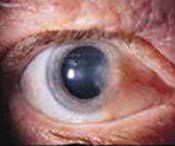
Symptoms of:
Keratitis (Corneal ulcer/inflammation) |

Redness worse around the iris
Prominent pain, which may be severe Photophobia & watery discharge Hx of recent trauma, long-term steroid eye drops, overuse of soft contact lenses |
|
|
Symptoms of:
Uveitis (Inflammation of the uveal tract = iris, ciliary body, choroid) |
Usually only in one eye, with redness mostly around the edge of the iris
Irregularly shaped pupil Prominent photophobia Moderate to severe pain Possibly impaired reading vision Usually due to an autoimmune reaction |
|
|
Symptoms of: Trauma
|
• Pain or foreign body sensation
• Vision is often blurred • May be blood, pupil may be affected • Hx of trauma |
|
|
Symptoms of: pterygium
|
usually develops over a period of years and is asymptomatic, but may be red and inflammed.
|
|
|
1. What causes a pterygium?
2. Onset? 3. Symptoms? 4. Complications? 5. Management? |
1. sustained environmental trauma (heat, dust, UV light), mostly in people who work oudoors, such as fishermen and farmers
2. develops over a period of years 3. Asymptomatic; may be acutely red and inflammed; usually raised, yellowy, fleshy and usually located on the nasal side of the conjunctiva 4. only affects vsion if gets big enough! 5. artificial tears often adequate; refer to opthamologist if gets too big or changes rapidly |
|

What can cause an occular pseudomembrane/membrane
|
True membranes become interdigitated with the vascularity of the conjunctival epithelium. They are firmly adherent, and tearing and bleeding often result when removed. B-hemolytic streptococci, Neisseria gonorrhoeae, Corynebacterium diphtheriae, Stevens-Johnson syndrome (severe systemic vesiculobullous eruptions affecting the mucous membranes-erythema multiforme) and chemical or thermal burns are among the common etiologic sources.
|
|
|
Red eye with dischage
|
probably conjunctivitis
|
|
|
Red eye with visual changes
|
Extreme caution, expecially if there is scleral redness
- halos, pain: acute closed angle galucoma - |
|
|
Red eye with true pain
|
Generally requires referral: scleritis, keratitis, acute galucoma
Conjunctival pain is often gritty/foreign body like |
|
|
Red eye, concentrated around iris
|
Bad sign:
uveitis |
|
|
Red eye, concentrated around fornices (corners)
|
conjunctivitis
|
|
|
Trigger points for referral of red eye?
|
- distortion of vision
- clouding of cornea - vomiting - irregularly shaped pupil - photophobia - redness localised around pupil - true eye pain **Redness caused by a foreign body |
|
|
Episcleritis - prognosis, cause, onset, management (3 points)
|
1. usually self limiting
could take 6-8 weeks to resolve, recurrent 2. presummably autoimmune induced inflammation of episcleral blood vessels 3. rapid 4. (a) reassurance - will clear (b) an NSAID such as aspirin may relieve symptoms (c) if recurrent or persistent refer to an opthamologist |
|
|
Scleritis -
1. how do i know if i'm dealing with scleritis or episcleritis (4) 2. outlook, management |
1. much less common, PAINFUL, underlying sclera IS pink, vision may be affected, may be associated with RA or other autoimmune disease
2. possible visual damage 3. (a) prompt referral to an opthamologist (b) meanwhile NSAIDs may help (c) manage with oral corticosteroids, antimetabolites |
|
|
Is there discharge with episcleritis or scleritis?
Is vision affected? |
No, it is rare, and if present is watery.
Vision is not affected in episcleritis but it may be impaired with scleritis |
|
|
Who is at increased risk of acute closed angle glaucoma?
|
1. people who are far-sighted
2. older people 3. asians 4. uveitis 5. diabetic retinopathy |
|
|
Acute closed angle glaucoma
1. Why does acute closed angle glaucoma tend to occur in the evening? 2. What examination suggests the diagnosis? 3. Where is the redness located? |
1. Because there is reduced light so mydriasis occurs
2. Gentle palpitation over the eye-lid (closed eye) suggests one eye is harder than the other 3. on the bottom half of the sclera |
|
|
Acute closed angle glaucoma
1. prognosis 2. management |
1. optic nerve atrophy and irreversible vision loss within hours - emergency; may resolve intermittently after e.g. lying supine
2. opthamologist / ED (a) premedication with IV acetazolamide, topical prilocarpine, topical beta blocker, topical apraclonidine, and oral mannitol/glycerol (b) as soon as the cornea is clear and inflammation has subsided, peripheral laser iridotomy (hours to 2 days)- opens another pathway for intra-ocular fluid ** interestingly, usually done in both eyes because there is an 80% of development later on |
|
|
Uveitis
(a) what is it, AKA? (b) symptoms in details (c) can be associated with what? |
(a) inflammation of the ciliary body and iris, aka iritis
(b) - pain (often an ache), - photophobia, blurred vision, sluggish reaction to light, miosis (vs. mydriasis in acute closed angle glaucoma) - sometimes a white purulent material, but minimal and watery discharge - red rings the iris (c) RA, IBD, autoimmune |
|
|
Uveitis
(c) complications (d) management |
(a) can cause glaucoma, cataracts, impair vision
(b) immediate referral to an opthamologist |
|
|
Keratitis (a corneal ulcer)
(a) causes (b) symptoms (c) management |
(a)
- recent trauma, dry eyes, viral conjunctivitis, UV light, soft contact lenses - long term steroids (b) pain is a prominent feature, and there is usually photophobia and watery discharge (more discharge if infective cause) (c) referral - best diagnosed and managed by an opthamologist |
|
|
A unilateral red eye with vomiting is what until proven otherwise?
|
Acute closed angle glaucoma
|
|
|
Red eye with severe pain or visual defect warrants what?
|
Opthamologist immediately
|
|
|
In viral conjunctivitis, what should never be prescribed?
|
Topical corticosteroid or local anaesthetic
|
|
|
Subconjunctival haemorrhage
prognosis and management |
Will resolve in 2-3 weeks
(1) reassure patient (2) evaluate contributing factors: refer if there is a history of trauma; refer if doesn't clear up |
|
|
Conjunctivitis
- what is the phenomenon "chemosis" |
Oedema of the conjunctiva causing a swelling around the cornea (iris)
Can occur in conjunctivitis |
|
|
What is the most common cause of a red eye?
|
Viral conjunctivitis
|
|
|
Viral conjunctivitis
(a) in one or both eyes? (b) does it affect vision? |
Often one eye first and then the other a few days later; like a bacterial eye infection, but more contagious and more likely to affect both
(b) Discharge may cause some blurring. PHOTOPHOBIA is uncommon. |
|
|
Viral conjunctivitis
(a) prognosis (b) management |
(a) usually self-limited
(b) 1. Highly contagious: washing hands frequently, don't share towels for about TWO WEEKS 2. There is evidence that ABX can shorten the course (prevent secondary infection); and are useful if dx is uncertain or if patient wants treatment 3. Regular use of artifical tears are recommended; a cool compress may also help 4. Refer if no improvement in 7-10 days |
|
|
Bacterial conjunctivits
- which bacteria |
- Staphylococcus & Haemophilus are common
- A wide range of gram +ve > gram -Ve bacteria can be involved - Chlamydia - Neisseria gonorrhoea |
|
|
Bacterial conjunctivitis
- one or two eyes? - lab studies? - prognosis |
- will start in one eye, usuallly spreads to the other within 48hrs
- only in severe cases - self-limiting (usually) lasting 2-3 days |
|
|
Bacterial conjunctivitis
- do what before treatment - treatment |
- if only in one eye, exclude serious pathology
- give antibiotics to reduce duration, prevent complications, and prevent spread (1) antibiotic eye drops (2) hygeine (3) artificial tears, cold compress (4) refer to a doctor if not improved after 2-3 days, and an opthamologist if doesn't improve in 1 week |
|
|
Bacterial conjunctivitis
- which eye drops? (a) which eye drops are more effective? (b) list which eye drops are available & their brands |
There is little data, but none shows a difference in efficacy (except perhaps with propramidine)
1. Sulfacetamide (Bleph-10) 2. (Dibromo)Propramidine [Brolene] 3. Chloramphenicol (Chlorsig, 4. Ciprofloxacin (CiloQuin, Ciloxan) 5. Ofloxacin (Ocuflox) 6. Tetracycline (SAS) Aminoglycosides: 7. Framycetin (Soframycin, Sofradex, Otodex) 8. Gentamicin (Genoptic, Minims Gentamicin) 9. Tobramycin (Tobrex) |
|
|
Which ABX eye drop to use?
|
1. Tobramycin, gentamicin (wide spectrum)
2. Chloramphenicol (not used routinely in US due to rare but devastating aplastic anaemia) 3. Quinolones - reserve for severe infections 4. sulphacetamide - avoid, irritating 5. propramidine - antiseptic not abx |
|

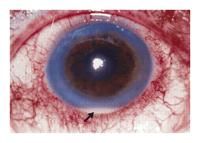
(a) What is this & nb. chemosis is present.
(b) cause (c) treatment |
(a) hyperacute bacterial conjunctivits - usually due to Neisseria gonorrhoea and in sexual active people.
(c) 1. immediate referral to an opthamologist 2. topical and systemic treatment 3. ask about genital symptoms 4. ask about sexual contacts |
|
|
Bleph-10
(a) what does anyone have against it? (b) dose form (c) dose regimen (d) children? (e) pregnancy, BF |
(a) An irritant, AMH advices that it's use be avoided
(b) 10% sulfacetamide, 15mL, SOLUTION (c) 1 drop every 2-4hr for 2 days; continue only if there is an improvement with 1 qid for 5 days (d) PI advices can be used w/o caution from 2 months (e) Cat C in pregnancy, avoid esp in last month - kernicterus in newborn; safe if BF (PI says different) |
|
|
Brolene
(a) action (b) uses (c) would it be ueseful where Bleph-10 isn't? |
(a) antiseptic
(b) may be useful for MRSA, also used for acanthamoeba keratitis; mild conjunctivitis only (c) Pregnancy: "appropriate if needed", BF: only appropriate whereas Bleph-10 is safe - ok in sulphur allergy and dry eye - children: not to be used in "infants" |
|
|
Brolene
(c) dose forms (d) children (e) preg, bf (f) SE (g) dose, inc ointment |
(c) 0.1% 10mL propamidine
0.15% 5g bromopropamidine oint (d) not in "infants" (e) pregnancy: "suitable if needed"; BF: safe (f) stinging, burning on instillation, allergy to benzalkonium preservative infrequent (g) 1 drop qid, oint tds for 2 days, if helping use up to 7/7 ** Use drops q2h probably more effective |
|
|
Chlamydia trachomatis
(a) complications (b) other forms of chlamydia (c) treatment (d) how is it spread? |
(a) blindness
(b) may be sexually transmitted, but is not the trachomatis specis, and does not cause blindnes (c) Azithromycin (erythromycin in neonates) & there is no evidence that topical therapy helps (d) contact and flies |
|
|
Allergic Conjunctivitis
(a) Treatment |
1. avoid allergen if possible - may be a topical medicine (conjunctivitis medicamentosa)
** cold compress 2. oral antihistamines 3. topical antihistamine (Levocabastine - livostin) 4. topical anithistamines with decongestants * antazoline with naphazoline * pheniramine with naphazoline 5. topical mast cell stabilisers * Cromoglycate, Lodoxamide Steroid eye drops if severe (specialist) topical NSAIDs has variable results |
|
|
Lomide?
- active ingredient - dosing - preg/bf - children - side effects |
lodoxamide (mast cell stabiliser)
- 1 drop qid - Cat B1, Caution in BF - Children 4 years and up (cf. Opticrom: no age specified) - Stinging on instillation (13%) |
|
|
Livostin
(a) children (b) preg (c) breastfeeding (d) dose regimen (d) side effects (f) other advice |
(a) 6 year plus
(b) B3; manufacturer CI use; SUSDP: must have label 62: do not use if pregnant and label 1 (c) Suitable if needed (d) 1 bd-qid (e) irritation on instillation & headache (all antihistamines), sedation (f) suspension - shake |
|
|
What is Zaditen?
(a) ingredient, moa, schedule (b) benefit (c) administration (d) children (e) pregnancy, BF (f) SEs |
(a) Ketotifen eye drops, antihistamine and mast cell stabiliser, S3
(b) fast onset in 15 mins (c) 1 bd (d) 3 years plus (half age of Livostin) (e) Preg B1, no human data, BF: suitable if needed (f) stinging on instillation, headache |
|
|
Another antihistamine eye drop?
(a) name, brand, schedule, MOA (b) disadvantage (c) dosing (d) children, preg, BF |
Patanol (Olopatadine) - S4
Also a mast cell stabiliser (b) besides headache and stinging, also causes dry eyes and keratitis and hyperaemia commonly (c) 1 drop bd (d) 3 year plus (sa Zaditen, half of Livostin), B1 - no data, BF: suitable if needed |
|
|
Name some antihistamine - vascoconstrictor combinations
|
Antihistine-privine, Albalon-A(Antazoline, naphazoline)
Naphcon-A, Visine Allergy (Pheniramine, naphazoline) |
|
|
Antihistamine - Vasoconstrictors
(a) dosage (b) preg and BF (c) children |
(a)1-2 drops up to qid, max 3-5 days
(b) no data in pregnancy or BF, avoid (c) Antihistine-privine in chidren 5years and up; the other two: 12 years and up only |
|
|
Vasoconstrictor eye drops
(a) products |
Naphazolin (Naphcon Forte, Albalon, Murine Clear Eyes)
Phenylephrine (Prefrin, Isopto Frin, & 5xsinlge use Albalon Relief) Tetrahydrozoline (Murine Sore Eyes, Visine Advanced Relief, Visine Original) |
|
|
Vasoconstrictors
(a) Your checklistwhen selling: CI, cautions (b) preg, bf (c) children (d) adverse effects |
(a) MAOIs (Parnate or Nardil), narrow anterior chamber: may precipitate closed angle glaucoma, glaucoma: may increase intracoluar pressure, contacts
(b) Safe in preg for up to 5 days, Safe in BF (c) PI: tetrahydozoline (Visine Advanced) if 6 years+, the other's don't say so avoid (d) transient irritation, rebound hyperaemia |
|
|
What about severe allergic conjunctivitis
|
May require steroids - see a specialist
|
|
|
What about mast cell stabilising eye drops
(a) name some (b) dosing of main one, safety in children, pregnancy, BF, onset of effect |

1. cromoglycate (Cromolux or Opticrom)
2. Lodoxamide (Lomide) 3. ketotifen (Zaditen) 4. olopatadine (Patanol) (b)Cromoglycate: 1 drop 4-6 times daily, no specified minimum age "children" ok, Cat A, safe in preg and BF Takes 2-4 weeks to work! |
|
|
Foreign body in the eye
Management? |
1. Wash in saline: This may be sufficient if not a solid or if just dust!
2. If a solid: Don't try and remove it yourself. Go straight to ED/GP, where they will (a) check vision (b) remove (or arrange an opthamologist to do it). 3. Patch to rest and allow scratches to heal. 4. Later check up by doctor. |
|
|
Once at home, after treatment of a foreign body, do what?
|
- With the patch on: Don't drive, work with machinery or work at heights (it can be very hard to judge distances)
- You can take the patch off after about 2hrs, or a day if there has been ulceration or abrasion - Take paracetamol - wear sunglasses prn - don't wear contacts until your eyes have healed |
|
|
Eye injuries - flash burns - what causes them and how do you treat them?
|
Exposure to bright UV light, such as through welding, sunlamps in tanning beds, or out on the sea or snow
1. Dilating drops to relax the eye muscles and ease the pain 2. eye dressing: rest and healing 3. antibiotics and a steroid drop may be used 4. review in 1-2 days to ensure healing 5. at home: care as for foreign body |
|
|
Eye trauma - when to refer?
|
All brunt trauma and abrasions
Any condition lasting >48 hrs |
|
|
Zinc sulfate in eye drops?
|
Aid removal of mucus from surface, may ppt protein
e.g. Zincfrin (with PE) and In-A-Wink (with naphazoline) |

