![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
In the respiratory system, cartilage is present from the ______ to the _______.
|
Trachea to Bronchi
|
|
|
In the respiratory system, cilia is present from the ______ to the _______.
|
Trachea to Respiratory Bronchioles
|
|
|
How does cartilage distribution differ in the trachea and bronchi?
|
Trachea: anterolateral distribution
Bronchi: distributed as plates of cartilage |
|
|
Goblet cells are located between ______ cells.
|
Ciliated
|
|
|
Which glands contribute most to mucus production in the respiratory system?
|
Mostly submucosal gland contribution, but some goblet cell contribution
|
|
|
K Cells:
Function Clinical Significance |
Neuroendocrine cells with processes extending in lumen; may play a role in regional control of ventilation and perfusion
Potential to become neoplastic |
|
|
How does epithelial cell type differ along the tracheobronchial tree?
|
Goes from pseudostratified columnar to single layer of cuboidal at level of terminal bronchioles
|
|
|
How do the presence/number of Goblet Cells differ along the tracheobronchial tree?
|
Decrease in number and are replaced by clara cells a TERMINAL bronchiole
|
|
|
Role of Clara Cells
|
Produce liquid layer of bronchiolar epithelium
|
|
|
How does airway size and proportion of smooth muscle change along the tracheobronchial tree?
|
Dec'd airway size, larger proportion of tree composed of cartilage
|
|
|
Pleura:
What cells line it? Static function? Dynamic function? |
Lined by mesothelial cells
Static fn: couples to chest wall Dynamic fn: lubricant, allows lung to move freely |
|
|
Acinus vs Secondary Pulmonary Lobule
|
Acnius = primary pulmonary lobule; functional gas exchange unit of lung--consists of respiratory bronchiole, its alveola ducts and alveoli
Secondary Pulmonary Lobule = collection of 3-5 respiratory bronchioles bordered by interlobar septa |
|
|
Conducting Zone:
Function ANS Innervation, NTs, and Effects |
Bring air into/out of lungs (Trachea-->Terminal Bronchioles)
Symp Innerv: beta-2 receptors act'd by epi-->dilation Psymp: muscarinic receptors act'd by Ach-->constriction + inc'd mucosal secretions |
|
|
Function of Type II Pneumocytes
|
1) Synthesize surfactant to reduce surface tension of alveoli
2) Regenerative capacity for Type 1 and Type 2 pneumocytes |
|
|
Why do alveoli require macrophages?
|
Alveoli lack cilia; need macs to remove debris/dust
|
|
|
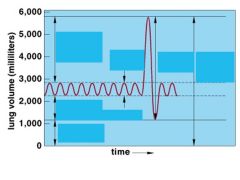
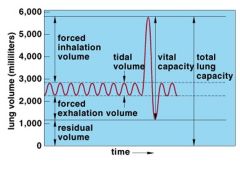
What is tidal volume?
|
Volume of air that fills alveoli and airways during quiet breathing
|
|
|
What is inspiratory reserve volume?
|
Add'l volume that can be inspired above tidal volume
|
|
|
What is expiratory reserve volume?
|
Add'l volume that can be expired above tidal volume
|
|
|
What is residual volume?
|
Volume remaining in lungs after maximal forced expiration; cannot be measured by spirometry
|
|
|
What is inspiratory capacity?
|
Tidal Volume + Inspiratory Reserve Volume
|
|
|
What is functional residual capacity?
|
Expiratory reserve volume + residual volume
AKA equilibrium volume--volume remaining after normal tidal volume expired |
|
|
What is vital capacity?
What factors increase/decrease it? |
Inspiratory capacity + expiratory reserve volume
Increases with size, male gender, physical conditioning; dec'd with age |
|
|
What mechanical factors determine total lung capacity?
|
Inc'd inward respiratory recoil = reduced inspiratory muscle strength
|
|
|
What mechanical factors determine residual volume?
|
In children: Inc'd outward respiratory recoil = reduced expiratory muscle strength
In adults: determined by airway closure |
|
|
|
|
|
What tests are used to measure FRC? Why can't spirometry be used?
|
Spirometry can't measure lung volumes that can't be exhaled (that remain in lung).
Use Helium dilution (breathe in known [ ] of He, breathe out diluted concentration of He, calculate volume of air in lungs that correlates with that concentration) Body plethysmograph: employs Boyle's Law (P1V1=P2V2); patient in airtight box, inspires, volume decreases in box, calculate FRC from pressure change. |
|
|
Anatomic vs Physiologic Dead Space
|
Anatomic Dead Space = volume of conducting airways; doesn't include respiratory bronchioles or alveoli. Doesn't participate in gas exchange and will be first air expired.
Physiologic Dead Space: total volume of lungs that doesn't participate in gas exchange. Includes FUNCTIONAL DEAD SPACE in alveoli (V/Q mismatch). In normal persons, physiologic dead space = anatomic dead space |
|
|
For a tidal volume of 500 mL, how much of the volume is in anatomic dead space?
|
150 mL
|
|
|
How is alveolar air sampled?
|
Must sample END-expiratory air (first air to be expired is air that was lingering in conducting airways--anatomic dead space)
|
|
|
Causes of elevated physiologic dead space.
|
Emphysema
PE Mechanical Ventilation Anesthesia |
|
|
Equation for determining Volume of Dead Space.
|
VD = VT x [PaCO2-PECO2]/PaCO2
If no dead space, VD = 0 If dead space = tidal volume, VD=1.0 |
|
|
What is minute ventilation?
Equation? |
Air moved into and out of lungs per unit time (minute)
VT x Breaths/Min |
|
|
What is alveolar ventilation?
Equation? |
Alveolar ventilation = minute ventilation corrected for physiologic dead space.
VA = (VT-VD) x breaths/min |
|
|
If CO2 production is constant, PACO2 is determined by ______.
|
Alveolar ventilation
|
|
|
When alveolar ventilation is halved, _________ is doubled.
|
PACO2
|
|
|
When alveolar ventilation is halved, _________ is halved.
|
PAO2; slightly more than halved FYI
|
|
|
What is forced vital capacity?
|
Total volume of air that can be FORCIBLY expired after MAXIMAL INSPIRATION.
|
|
|
Normal value of FEV1/FVC.
What does this volume mean? |
Normally 0.8, meaning, 80% of vital capacity expired in first second of forced expiration.
|
|
|
When is FEV1/FVC decreased?
|
Obstructive lung disease (asthma)
|
|
|
When is FEV1/FVC increased?
|
Restrictive lung disease (fibrosis)
|
|
|
What is senile emphysema?
|
Enlargement of alveolar ductal airspaces in elderly; dilation without destruction.
|

