![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
What three forces must be overcome to inhale?
|
Elastic: lungs and chest wall resist stretch (volume dependent)
Resistive: viscosity of lung tissue and airway resistance (flow-dependent--quicker you inhale, the more resistance you get) Intertial: ignored unless ventilating at high frequencies |
|
|
What lung forces promote collapse?
What force prevents collapse? |
Elastic forces: surface tension of alveoli, lung tissue elastic recoil
Chest wall prevents collapse (pushes against recoil and surface tension forces) |
|
|
How is alveolar pressure measured?
|
At the mouth under 2 conditions:
1) No airflow 2) Glottis is open |
|
|
What is normal pleural pressure (approximately)? Chest wall?
Lung? Pressure of respiratory system? |
Lung pressure = Palv-Ppl=0-(-5)=+5cmH2O
Pleural pressure ~-5 cmH2O Recoil of chest ~+5 cmH2O Thus Pressure of resp syst = 0, no mvmt of air into our out of lung |
|
|
What presure changes occur at 60% vital capacity?
|
Volume where chest wall is neutral; won't collapse or expand
Thus Ppl = 0 Pbody surface =0 Chest wall pressure = 0 Lung wants to collapse |
|
|
What pressure changes occur at total lung capacity?
|
Chest and lung want to collapse in (requires a lot of force)
|
|
|
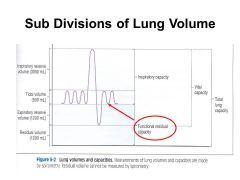
What is functional residual capacity? When does it occur?
|
Functional Residual Capacity (FRC) is the volume of air present in the lungs, specifically the parenchyma tissues, at the end of passive expiration.
FRC occurs at 0 (~60% vital capacity) so that propensity for RS to collapse is due to lung and nothing else |
|
|
What is the formula for compliance?
What is normal tissue compliance? How does it change in emphysema and fibrosis? |
Compliance: deltaV/deltaP
NL: Crs = 100 ml/cm H2O, Clungs = 200, C chest wall = 200 In emphysema, mroe compliant, In fibrosis, less compliant (more fibrinogen) |
|
|
What is transthoracic pressure (formula)?
|
Palv-Pbs = Prs
|
|
|
What is trans chest wall pressure (formula)?
|
Pcw = Ppl - Pbs
|
|
|
What is the role of surfactant?
|
Minimizes surface tension
Equalizes pressure in large and small alveoli: Reduce surface tension in smaller alveoli (which have greater pressures than larger alveoli). This prevents lung collapse (atelectasis) due to high pressure (smaller) alveoli emptying into low pressure (larger radius) alveoli. |
|
|
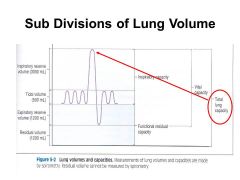
What is total lung capcity?
What determines it? |
The amount of gas contained in the lung at the end of a maximal inhalation.
Need strong inspiratory muscles. Determined by Increased Inward Expiratory forces (Respiraoty system recoil at TLC) and Reduced Inspiratory Muscle Strentgth at TLC (these two must equal each other) |
|
|
Expiratory pressure is greatest at _______ and lowest at _________.
|
Expiratory pressure is greatest at TLC, lower at FRC/RV
|
|
|
Inspiratory pressure is greatest at _______ and lowest at _________.
|
Inspiratory pressure is greatest at TLC (most positive ~-50), lowest at FRC/RV (-100)
Inspiratory muscles get weaker as you approach greater volumes. |
|
|
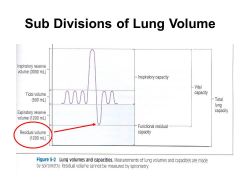
What is residual volume?
What determines it in children? In adults? |
Air remaining in the lungs after the most complete expiration possible
Determined by Increased Ouward (Inspiratory) RS recoil at RV and Reduced Expiratory muscle strength at RV (these two must equal each other)--this is in adults In adults, it's due to airway closure and not so much expiratory muscle weakness. |
|
|
|
|
|
|
|
|
|
|
|
Alveolar pCO2 is proportional to ____________.
When would you get hyperventilation? Hypoventilation? |
Metabolic Rate/Alveolar Ventilation
Hyperventilation when pCO2 too high Hypoventilation when pCO2 low |
|
|
What is anatomic dead space? How much of tidal volume does it account for?
|
Anatomic dead space = air in nose, trachea, bronchi and subdivisions
Accounts for 1/3 of tidal volume |
|
|
What factors affect laminar flow?
|
RADIUS (to the 4th power)
Flow is linearly related to pressure Viscosity |
|
|
Laminar flow is prominent in the _______.
|
Small airways
|
|
|
Turbulent flow is prominent in the ________.
|
large airways: trachea (HIGHEST RESISTANCE)
|
|
|
Transitional flow is prominent in the ________.
|
Carina, branching of airways
|
|
|
Describe pressure changes in the lung and pleural space at FRC, inspiration, end-inspiration, and expiration.
|
FRC: NO FLOW; Lung = 0, Ppl = -5
Inspiration: Plung = -1; pPl =-7 End-inspiration: NO FLOW: P=0, Ppl=-8 Expiration: Plung = +1, Ppl = -6 |
|
|
How does alveolar compliance differ in the apex and base of the lung?
|
Alveoli in apex are less compliant (more stretched), experience less change in volume
Alevoli in base are more compliant, change more in volume |

