![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
50 Cards in this Set
- Front
- Back
|
What are the permanent mucosal folds present in the D, J, and proximal ileum called?
|
Plicae Ciculares
|
|
|
What is the point of Plicae Circularis?
|
Increases SA of small intestine by a factor of 2-3 and decrease the velocity of movement of chyme along the alimentary canal.
|
|
|
Where is the villi frequency the highest? What is the approx height of the villi in the duodenum vs ileum?
|
In the Duodenum. Height in duodenum = 1.5 vs ileum = 0.5mm
|
|

What structure is the lower arrow pointing to?
|
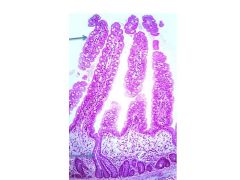
Crypts of Lieberkuhn
|
|
|
What three layers make up the intestinal mucosa?
|
1. Simple columnar epi
2. Lamina propria 3. Muscularis mucosae |
|
|
What type of cells is the simple columnar epi covering the villi and the intervillar space composed of? (3 types)
|
1. Absorptive cells
2. Goblet cells 3. DNES (enteroendocrine) cells |
|
|
What extends up into the villi? I.e. what are they an extension fo?
|
Lamina propria
|
|
|
What structures can be found within the LP of a microvilli?
|
Lacteal and several capillaries. Also smooth muscle fibers, loose connective tissue, lymphoid cells.
|
|
|
In addition to terminal digestion and absorption of water and nutrients, what else does the absorptive cells/enterocytes process?
|
They re-esterify fatty acids into triglycerides, form chylomicrons, and transport the bulk of the absorbed nutrients into the lamina propria for distribution to the rest of the body.
|
|
|
Describe the cellular morphology of the enterocytes (including nucleus)
|
Columnar epithelium ~ 25uM high - with an elongated nucleus.
|
|
|
What is found on the lateral walls of the absorptive cells?
|
1. Zonulae Occludentes
2. Zonulae Adherentes 3. Desmosomes 4. Gap junctions |
|
|
About how many microvilli/cell?
|
3000
|
|
|
What is the microvilli covered in? What is its function?
|
1. Microvilli covered in glycocalyx coat
2. Has protective roles and also integrally involved in the digestion of disaccharides and dipeptides into monomers for absorption through peptide hydrolases and disaccharidases that are abundant on the apical surface. |
|
|
To what structure are the microvilli attached to?
|
Intermediate filaments of the enterocyte terminal cytoskeletal web through bundles of actin filaments
|
|
|
Describe the composition of mucin:
|
20% protein and 80% carbohydrate.
|
|
|
DNES (enteroendocrine) cells produce what category of hormones?
|
Paracrine and endocrine
|
|
|
The Crypts of Lieberkuhn have three types of cells:
|
1. Enteroendocrine cells
2. Paneth 3. Stem cells |
|
|
Describe the migration of Paneth and Stem cells in the Crypts of Lieberkuhn.
|
Stem cells migrate to the surface of the microvilli epithelium and ultimately sloughed off. Paneth cells are long lived and do not participate in the upward migration.
|
|
|
What do Paneth cells produce/secrete?
As you'd expect, what type of organells are abundant in these cells? |
Lysozymes, defensins that neutralize bacterial and viral infections. RER, numerous mitochondria, large apical secretory granules are abundant.
|
|
|
The lamina propria forms the core of the villi and extends down to the:
|
muscularis layer.
|
|
|
The muscularis mucosae is present as an:
(type of muscle and its orientation) |
Inner circular and outer longitudinal layer of smooth muscle fibers.
|
|
|
Describe the relative frequency of lymphoid nodules in the small intestine.
|
Mostly in ileum with some more in jejunum, least numerous in duodenum
|
|
|
What is believed to cause inflammatory bowel disease? What gene might be involved?
|
IBD is believed to be caused by a defect in the immune reaction to bacteria colonizing the gut, resulting in uncontrolled chronic inflammation of the gut mucosa. The gene possibly involved = NOD2.
|
|
|
Describe the muscularis Mucosae. (talk about its arrangement and how this is usefull.
|
Composed of inner circular layer and outer longitudinal layer of smooth muscle. The inner layer extend through its core to the tip of connective tissue, as far as the basement membrane.During digestion, fibers rhythmically contract, shortening the villus
|
|
|
What gland distinguishes duodenal submucosa from the rest of the GI?
|
Brunner's Glands. The junction of the stomach and duodenum is marked by the presence of the pyloric sphincter and appearance of Brunner's
|
|
|
Describe how Brunner's glands are situated.
|
They ascend through the muscularis mucosae layer and enter the Crypts of Lieberkuhn to deposit their secretions into the lumen.
|
|
|
What does the Brunner's Gland secrete and what is the purpose? (two things)
|
It secretes alkaline mucus that neutralizes the pH of gastric chyme and protects the duodenum. It also produces epidermal growth factor that may be involved in stem cell proliferation in the crypts.
|
|
|
Brunner's gland secretion is stimulated by: (2 things)
|
1. Submucosal Plexus
2. Cholecystokinin and secretin |
|
|
Describe the muscularis externa (with respect to muscle orientation, what is between the two layers)
|
Inner Circular, Outer Longitudinal. Between is the Myenteric Plexus (Auerbach)
|
|
|
Mixing contractions are localized and do what to chyme?
|
Exposes it to digestive juices.
|
|
|
Peristaltic movement is mediated by Miesssern's or Auerbach's plexus?
|
Myenteric
|
|
|
It makes sense that the the villi in the duodenum are more numerous and taller than in other parts of the small intestine. However, what are there fewer of?
|
Goblet cells
|
|
|
Where are Brunner's glands found in duodenal tissues?
|
Submucosa
|
|
|
Where do Payer's patches reside in the ileum?
|
Lamina propria - in the wall of the ileum that is opposite to the attachment of the mesentary. Villi are reduced in hight or absent above the patches.
|
|
|
How much fluid, Na, CHO, protein, and fat is absorbed by the intestine daily?
|
1. 7L fluid
2. 30 kg sodium 3. 0.5g kg CHO and protein 4. 1 kg of fat |
|
|
?? degrades fats into:
|
Pancreatic lipases degrade it into free fatty acids and monoglycerides
|
|
|
Once micelles transfer long chain FA into the cell, what happens?
|
They are re-esterified in triglycerides by smooth ER.
|
|
|
What is the difference between micelles and chilomycrons?
|
Micelles are emulsified fatty acids in bile salts. Chilomycrons are TGs combined with lipoprotein and released into lacteals of the intestinal villi.
|
|
|
What is the hallmark of ciliac disease?
|
missing microvilli
|
|
|
Does the colon have villi?
|
No - it is relatively smooth
|
|
|
The colon epithelium consists of cells similar to the small intestine with the exception: (missing these cells?)
|
Paneth
|
|
|
Although the colonic mucosa is absent of villi, it is full of ?? with cell types that are similar to small intestine.
|
Crypts of Lieberkhun
|
|
|
Discuss how the colon muscular layers differ compared to the small intestine.
|
The muscularis mucosae is more developed with clear circular and longitudinal fibers. The submucosa is not distinctive but the the externa is with three distinct bands called taenia coli that remain partially contracted and cause the large intestine to be puckered into sacuulations called haustra coli.
|
|
|
The appendix tissue is similar to the intestine but a characteristic feature is the presence of:
|
masses of lymphoid tissue in the mucosa and submucosa and mucosal glands are more dispersed.
|
|
|
Rectal mucosa are similar to colon except:
|
Crypts are deeper and goblet cells are more abundant
|
|
|
What is the cell type at the transition from recto-anal junction?
|
Epithelium transitions from simple columnar to stratified squamous.
|
|
|
What two venus plexi are found in the submucosa of the anal canal?
|
Internal hemorrhoidal plexus and external hemorrhoidal plexus.
|
|
|
From proximal to distal, what are the sphincters of the anus? Include the muscle type for each.
|
Anal sphincter (thickened smooth muscle) and then external anal sphincter (striated muscle)
|
|
|
What causes Hirschsprung's Disease?
|
Neural Crest Cells do not migrate to the distal colon and there are no nerves there. The colon enlarged (anus is small), is non-functional and must be removed.
|
|
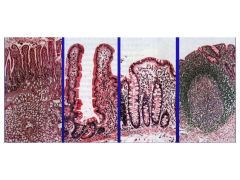
From left to right, name these tissues
|

1. Duodenum (brunner's glands)
2. Illium (villi and crypts, Payer's patches) 3. Colon (just Crypts, no paneth cells) 4. Appendix (lymphoid tissue) |

