![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
Warm it up: 7 causes of cell injury
|
hypoxia/ischemia
physical agents drugs/chemicals infectious agents immunologic reactions nutritional imbalances genetic |
|
|
most common cause of hypoxia
|
ischemia
|
|
|
Examples of physical agents causing cell injury
|
trauma
burns deep cold |
|
|
A genetic example of a cell injury cause
|
sickle cell anemia
|
|
|
What are the three responses a cell can have to an injurious agent?
|
Adaptation
Injured reversibly Injured irreversibly and dies (via either necrosis or apoptosis) |
|
|
What factors determine if a cell injury is reversible/irreversible?
|
Duration of exposure
Dosage Type of cell and its ability to adapt (neurons are weaksauce compared to cardiomyocyte during hypoxia) |
|
|
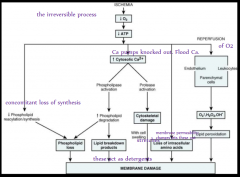
What are the four grand biochemical themes in cell injury/death?
|
Role of oxygen
Intracellular Ca/loss of Ca homeostasis ATP depletion Defects in membrane permeability |
|
|
How is O2 like money a parent gives a kid?
|
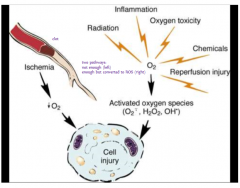
In ischemia it ain't flowing to kid; in hypoxia, the parent just doesn't have any. Kid doesn't get any and runs out of (A)TP.
Or kid gets spoiled with lots of O2, bad morals, drugs, and too much tanning (radiation, inflammation, straight up oxygen toxicity, reperfusion, chemicals) -> ROS Best case is balanced |
|
|
What are those ROS's again?
And what are they destroying? |
Oxygen-derived free radicals: superoxide O2-, hydrogen peroxide H2O2, hydroxyl radical OH'
Cellular proteins, phospholipids, nucleic acids |
|
|
Why/how is Ca loosed in damaged cells? Explain by contrasting to healthy cell.
|
Healthy/normal cell: Ca is sequestered in organelles (mitochondria, smooth ER) and little is free in cytoplasm. Ca ATP-ases pump Ca across membranes to maintain this environment.
Agents can affect the ATP-ases (hypoxia -> lack of ATP or directly targeted) |
|
|
What 5 things can happen once Ca homeostasis is lost?
|
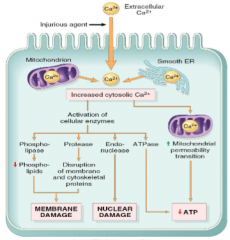
Phopholipases activated -> destroy membrane
proteases activated -> destroy cytoskeleton -> destroy membrane endonucleases activated -> destroy DNA/chromatin fragmentation ATPases activated -> ATP depletion Mitochondrial permeability transition pores formed -> no ATP production |
|
|
What is the relationship between the cytoskeleton and membrane?
|
They are physically attached to each other, so if the cytoskeleton is disrupted, the membrane will be destroyed.
|
|
|
What are sources of mitochondrial injury or dysfunction?
|
Increased cytosolic Ca
ROS lipid peroxidation |
|
|
What effects does mitochondrial damage cause? What do these lead to?
|
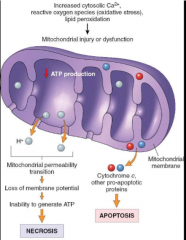
With mitochondrial permeability transition -> membrane potential (proton gradient) is lost -> cannot make ATP -> necrosis
Cytochrome c and other pro-apoptotic proteins escape -> apoptosis |
|
|
ATP depletion is a common theme in cell injury- what is causing this?
Why is this bad exactly? |
Either activation of ATPases and/or decreased ATP synthesis.
Need ATP to support the membrane (synthesizing materials and maintaining pumps)- without enough ATP, membrane will fail. |
|
|
Defects in membrane permeability: causes
|
direct damage by toxin
indirectly through Ca dependent enzymes |
|
|
What are the key features in reversible injury caused by ischemia?
|
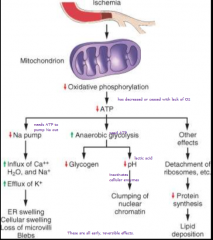
mitochondria cannot make ATP (no O2 to accept electrons) ->
1 increased anaerobic glycolysis -> lactic acid -> lowers pH -> impairs intracellular enzymes 2 Na/K pumps fail -> influx of Na and H2O These are all early stage- if oxygen restored, all fixed. |
|
|
What are the key features in irreversible injury caused by ischemia?
|
After a certain point, mitochondria are beyond repair:
phospholipids lost (Ca-> phospholipases and no ATP for new ones; breakdown products act like detergent -> more damage) cytoskeletal abnormalities (Ca -> proteases) reperfusion injuries (O2 reestablished -> oxygen-derived free radicals pillage what's left and local healthy cells -> lipid peroxidation) amino acids lost (normally protect membrane from hypoxic damage) |
|
|
What amino acid in particular did he list as protector of membranes?
|
Gly
|
|
|
What was the name of the pink stain used in the examples to look at healthy and dead cells?
|
hematoxylin and eosin
H & E |

