![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
|
|
|
Background for ivabradine |
•Increased heart rate is a significant predictor of death andcardiovascular death/hospitalization in heart failure patients •Hypothesis that lowering heart rate could be beneficial for cardiacfunction and clinical outcomes in heart failure patients •If is a mixed Na+–K+ inward current activated by hyperpolarization and modulated by theautonomic nervous system |
|
|
Why is I(f) important? |
•Important ionic current for regulating pacemaker activity in the sinoatrial (SA) node |
|
|
Therapeutic indication of ivabradine |
Reduce hospitalization for patients with symptomatic (NYHA classII-III) stable chronic HFrEF (LVEF ≤35%) receiving standard of care, including a beta blocker,and who are in sinus rhythm with a heart rate of ≥70 bpm at rest |
|
|
MOA of Ivabradine |
•Selectively inhibits the If (“funny” ion channel) current in the sinoatrial node, prolongingdiastolic time and reducing heart rate •Increases stroke volume, preserves myocardial contractility and relaxation, AVconduction, and ventricular repolarization |
|
|
Adverse effects of ivabradine |
•Luminous Phenomenon (sensations of enhanced brightnessin a fully maintained visual field)--- due to Ifchannel in retina •Bradycardia •First-degree AV block, ventricular extrassystoles •Dizziness •Blurred vision |
|
|
Contraindications for Ivabradine |
•Sick Sinus Syndrome •With Verapamil or Diltiazem (Ca2+ channel blockers) •With potent inhibitors of CYP3A4 |
|
|
Propranolol - drug class and MOA for HTN |
B-adrenergic antagonist, reduce adrenergic effects |
|
|
Carvedilol - drug class and MOA for HTN
|
B-adrenergic + alpha-adrenergic blockers - reduce adrenergic effects |
|
|
Prazosin - drug class and MOA for HTN |
Alpha adrenergic blockers - relax vascular smooth muscle |
|
|
Clonidine - drug class and MOA for HTN |
Reduce release of NE |
|
|
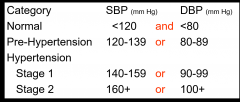
Classification of BP in adults |
|
|
|
Integrative cardiovascular system responses to vasomotor drugs depend on: |
1) Combined net effects of drug actions on target receptors (independent effects) 2) Inter-dependent relationship among CV variables (dependent effects) 3) Compensatory or autonomic neural reflexes (evoked reflex effects) |
|
|
Phenylephrine |
Selective alpha-1 agonist |
|
|
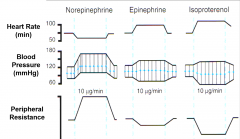
Describe changes to blood pressure, heart rate, CO, and peripheral resistance with physiologic epi |
Beta adrenergic effect Arterial pressure - systolic increases, diastolic decreases, so MAP remains the same HR -increases (B1 receptors in the heart) CO - increases (sustained - due to inc HR + decreased TPR) (B1 receptors regulate HR + contractility) Peripheral resistance - decreased |
|
|
Describe changes to blood pressure, heart rate, CO, and peripheral resistance with pharmacologic epi |
Alpha adrenergic effect Arterial pressure - all pressures increase (increased MAP) Decrease in HR - due to baroreceptor reflex Decreased CO - due to decreased HR + peripheral resistance Increased peripheral resistance - alpha-1 receptors on blood vessels |
|
|
Describe changes to blood pressure, heart rate, CO, and peripheral resistance with phenylephrine |
Increase in arterial pressure (moreso than epi) Decrease in HR (moreso than epi) Decrease in CO (moreso than epi) Increased in peripheral resistance (moreso than epi) effects are more pronounced than pharmacologic epi due to the fact that phenylephrine is a selective alpha-1 agonist |
|
|
Effects of NE, epi, and isoproterenol on HR, BP, and peripheral resistance |
|
|
|
Isoproterenol |
Non-selective B1, B2 agonist |
|
|
CV effects of high dose epi after selective alpha and beta receptor blockade |
Whena high dose of epinephrine is administered in the presence of an a-adrenergicreceptor antagonist the predominant a-adrenergicreceptor-mediated response is “reversed” to one where b-adrenergicreceptor-mediated effects predominate, including relaxation of smooth muscle,decrease in blood pressure, bronchodilation, increase in heart rate, increasedlikelihood of cardiac arrhythmias, etc. Opposite is true for b-receptor inhibition |
|
|
Uses for vasoconstrictor drugs? |
-Increase BP in hypotensive situations -Restore cardiac output by constricting the systemic veins -Improve blood flow to pressure dependent vasodilated organs under special conditions (hemorrhagic or hypotensive shock) -Reduction of local or regional blood flow (eg achieving hemostasis in surgery, for reducing diffusion of local anesthetics, and for reducing mucous membrane congestion) |
|
|
Ex of alpha adrenergic receptor agonist? |
Phenylephrine |
|
|
Ex of uptake-1 blockers |
Tricyclic antidepressants Cocaine |
|
|
Ex of indirect acting sympathomimetics |
Tyramine Ephedrine Amphetamine |
|
|
Ex of mixed alpha, beta, dopamine receptor agonist |
Dopamine |
|
|
Dopamine method of admin + use |
-IV only -Useful in pt with hypotensive shock (after correction of hypovolemia) -Acute heart failure |
|
|
Mechanism of dopamine |
-Dose dependent differential receptor MOA 1) Low dose: acts on peripheral dopamine receptors (D1) to produce a selective dilation of renal and splanchnic vessels 2) Mid dose: acts on B1 adrenergic receptors in the heart to produce tachycardia and increased contractility 3) High dose: acts on a1 adrenergic receptors to increase peripheral vascular resistance |
|
|
Adv effects of dopamine |
similar to other catecholamines |
|
|
Why do we use vasodilator drugs? |
-Blood flow improvement - ischemic tissues/organs -BP reduction -Heart pump function improvement |
|
|
CNS sympatholytics drug classes |
a2 receptor agonists b1,2 receptor antagonists |
|
|
Peripheral sympatholytics drug classes |
Ganglionic blocking drugs Norepi synthesis + release inhibitors a1 receptor antagonists combined a1 + B1,2 receptor antagonists |
|
|
Receptors found on pre and postsynaptic sympathetic nerve terminals? |
Pre-synaptic: a2 receptor - inhibits NE release, b2 receptor - stimulates NE release Post-synaptic: -a1 receptors (blood vessels - constriction) -b1 receptors (heart - inc HR + contractility) -b2 receptors (blood vessels - vasodilation @ skeletal muscle) |
|
|
Ex of presynaptic a2 receptor agonists
|
Clonidine a-methyldopa (via its metabolite - a-methyl NE) |
|
|
MOA of clonidine + a-methyldopa |
Lower blood pressure and reduces peripheral and renal vascularresistance principally through an action on pre-synaptic alpha-2 adrenergicreceptors |
|
|
Clonidine CNS site |
Clonidine,a presynaptic a2-adrenergic receptor agonist, causes a reduction in theadrenergic outflow from the CNS and thereby reduces catecholamine release fromperipheral adrenergic nerves, and also reduces renin release and its consequentactions. |
|
|
Clonidine vs alpha-methyldopa on HR + CO |
Clonidinelowersheart rate and cardiac output morethan does methyldopa. |
|
|
Indications/uses for clonidine |
-HTN -Reduce BP in supine position, rarely causing postural hypotension |
|
|
Cautions for use of clonidine |
-Severe coronary insufficiency -Recent MI (exacerbate ischemic injury) -Cerebrovascular disease -Chronic renal failure |
|
|
Adverse rxns of clonidine |
-Dry mouth -Constipation -Drowsiness and dizzines -Rebound HTN on abrupt withdrawal (when you are taking drug chronically, downregulate presynaptic a2 receptor levels - these are reducing sympathetic outflow so postsynaptic alpha receptors are upregulating) |
|
|
Rebound HTN due to ____ withdrawal |
clonidine |
|
|
Rebound HTN + clonidine |
-Rebound HTN may be observed upon rapid withdrawal of pre-synaptic a2 receptor agonists -This "rebound HTN" is believed to be a result of: 1) Down-regulation of central pre-synaptic a2 receptors 2) Upregulation and expression of peripheral post-synaptic a1 receptors on vascular smooth muscle -Consequence is hyperactive autonomic CV system -Treatment of HTN crisis: reinstitute clonidine therapy or admin of a and b receptor blocking agents |
|
|
alpha-methyldopa CNS site |
a-Methyldopa, a presynaptic a2-adrenergic receptor agonist, causes a reduction in theadrenergic outflow from the CNS and thereby reduces catecholamine release. |
|
|
a2 adrenergic receptors for clonidine vs a-methyldopa |
A-methyldopa acts at different pre-synaptic a2-adrenergic receptor than those forclonidine’s action |
|
|
Indications/use for a-methyldopa |
-Used primarily for HTN during pregnancy -Reduces BP in supine position, rarely causing postural hypotension |
|
|
Contraindications for a-methyldopa |
Liver disease |
|
|
Adverse reactions for a-methyldopa |
-Positive Coomb's test (agglutination of RBCs) -Sedation -Lactation in women and men (inhibition of dopaminergic system in hypothalamus) -Fever -Jaundice |
|
|
Ex of a2 adrenergic receptor antagonists |
-Phentolamine (a1 = a2) -Prazosin (a1 >> a2) |
|
|
Ex of b-adrenergic receptor antagonists |
Propranolol (B1 = B2) Metoprolol (B1 >> B2) |
|
|
a + B blockers |
Labetolol (a1 + B1 + B2) (a:B = 1:5) Carvedilol (a1 + B1 + B2) - greater B affinity than labetolol |
|
|
Phentolamine drug class and MOA |
Phentolamineis a competitive non-selective alpha1/2adrenergic receptor blocker. This leads toarterial and venous dilation resulting in reduced peripheral vascularresistance and venous return |
|
|
With phentolamine, BP is reduced more in the ____ position than ____ position. What is observed because of this? |
Bloodpressure is reduced more in the upright than in the supine position. Due tolowered blood pressure, reflex tachycardia is observed. |
|
|
Effect on blood volume of phentolamine? |
Retention of salt and water occurs whenthese drugs are administered without a diuretic. |
|
|
Use of phentolamine more effective with _____ |
Thedrugs are moreeffective when used in combination with other agents, such as a beta-blocker and adiuretic, than when used alone. |
|
|
Indications/uses for phentolamine |
-Pheochromocytoma -Prevention of dermal necrosis after IV NE or dopamine |
|
|
Contraindications for phentolamine |
Coronary artery disease (hypotension can evoke angina + AMI) |
|
|
Adverse reactions of phentolamine |
-Acute + prolonged hypotension (due to B2 receptor activation and high NE levels) -Accompanying tachycardias and arrythmias (high levels of NE at B-receptors) |
|
|
Prazosin class + effects |
Prazosinis a competitive, selective alpha1 antagonist that causes arterial and venous dilation. |
|
|
With prazosin, blood pressure is reduced more in the ____ than in the _____ - effect? |
Bloodpressure is reduced more in the upright than in the supine position. No reflex tachycardia is observed due to unopposednegative feedback of alpha2 stimulation |
|
|
Blood volume changes with prazosin? |
Retention of salt and water occurs whenthese drugs are administered without a diuretic |
|
|
What makes prazosin more effective? |
Thedrugs are moreeffective when used in combination with other anti-hypertensive agents. |
|
|
Indications/uses for prazosin |
-HTN (2nd line drug) -BPH (bladder + prostate smooth muscle relaxation improves urine flow) |
|
|
Contraindications of prazosin |
Hypersensitivity to congener drug (ex terazosin, doxazosin) |
|
|
Adverse rxns of prazosin |
-"First dose" hypotension, dizziness, and syncope -Nasal congestion (vasodilation by unopposed B-receptor action of NE) |
|
|
B-adrenergic receptor antagonists - first, second, and third generation compounds |
-First generation B-blockers: propranolol (nonselectively block B1 and B2, and sometimes B3, receptors) -Second generation: metoprolol (have relative selectivity for B1 receptors (largely cardiac) when given in low doses) -Third generation: carvedilol (have added vasodilatory properties - a1-receptor blockade) |
|
|
Benefits of B-receptor blockers |
-Lower blood pressure in mild to moderate HTN -In severe HTN, prevent reflex tachycardia of direct vasodilators -Reduce mortality after a MI (timolol, propranolol, or metoprolol) and reduce mortality in pts with heart failure (carvedilol, metoprolol succinate); advantageous for treating HTN in pts with these conditions |
|
|
Sites of action of B-blockade in HTN |
-Central adrenergic inhibition -Block heart receptors - decrease HR, SV, CO -Renal b-receptor blockade - decreased renin production -Reflex SVR increase, but later NE release is inhibited and SVR falls --> late BP decrease |
|
|
Side effects of B-blockers |
1) Smooth muscle spasm (bronchospasm) 2) Exaggeration of cardiac actions (bradycardia, heart block, andnegative inotropic effect) 3) Central nervous system effects (insomnia, depression) |
|
|
Contraindications of B-blockers |
Cardiac contraindications: •Severe bradycardia•Preexisting high-degree heart block•Untreated overt LV heart failure Pulmonary contraindications: •Asthma•Severe bronchospasm Central nervous systemcontraindication:•Severe depression (especially for propranolol) Activeperipheral vascular disease with rest ischemia |
|
|
Propranolol sites of action + effect |
Propranolol is a competitive, non-selective beta1/2 adrenergic receptor antagonist which reduces adrenergic outflow from the CNS and thus decreases peripheralcatecholamine release from adrenergic nerves and also decreases renin release and subsequent angiotensin formation and aldosterone release. NOTE: propranolol has the same receptor targets in the periphery |
|
|
Indications for propranolol |
–hypertension –angina pectoris –hypertrophic subaortic stenosis –supraventricular arrhythmias –tachycardia of digitalisintoxication –myocardial infarction –pheochromocytoma (in presence ofalpha1-blocker) –migraine –essential tremor Usually used as 2nd/3rd line therapy for many conditions |
|
|
Contraindications for propranolol |
-Sinus bradycardia -More than first degree heart block -Overt heart failure -Bronchial asthma or bronchospasm or COPD -Pheochromocytoma in absence of a1 receptor antagonist |
|
|
Adverse reactions with propranolol |
-Bradycardia -Vertigo and fatigue -Sexual dysfunction -Dry mouth and assorted GI problems -After prolonged regular use, some patients experience a withdrawal syndrome |
|
|
Precautions of use with propranolol |
-Blunting/masking of signs (ex tachycardia) of diabetes (hypoglycemia) and thyrotoxicosis -Increased lipids (but not HDL) |
|
|
Metroprolol site + effects |
Metoprolol is a competitive, selective beta1 antagonist that causes decrease renin release, and reduce heart rate and cardiac contractility. |
|
|
Metoprolol indications/use |
Hypertension Heart failure (extended release form) |
|
|
Contraindications of metoprolol |
2 or 3rd degree heart block |
|
|
Adverse reactions of metoprolol |
Cardiac depression AV conduction block Sexual dysfunction |
|
|
Carvedilol + labetolol site of action + effects |
Carvedilol or Labetalol is a competitive non-selective beta1/2receptor and alpha1 receptor antagonist.This results in decreased catecholamine release from adrenergic nerves, vasodilation, decreased heart rate and alsodecreased renin release and subsequent angiotensin formation and aldosteronerelease. |
|
|
Carvedilol indications/uses |
HTN Heart failure |
|
|
Contraindications for carvedilol |
Bronchial asthma 2nd or 3rd degree heart block |
|
|
Adverse reactions w/ carvedilol |
-Cardiac depression -Sexual dysfunction (rare) -Blunting/masking of signs (ex tachycardia) of diabetes (hypoglycemia) and thyrotoxicosis -Combination of those with propranolol and prazosin |
|
|
Labetolol indications/uses |
Hypertension (oral form) Pregnancy-induced HTN Hypertensive emergencies (IV form) |
|
|
Contraindications for labetolol |
-Heart failure -- major difference between this and carvedilol -Bronchial asthma -2nd or 3rd degree heart block |
|
|
Adverse reactions with labetolol |
-Cardiac depression -Sexual dysfunction (rare) -Hepatic injury -Blunting/masking of signs/sx (ex tachycardia) of diabetes (hypoglycemia) and thyrotoxicosis -Combination of those with propranolol and prazosin |

