![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
|
The first positive deflection before the QRS. Represents the depolarization of both the right and left atria.
|
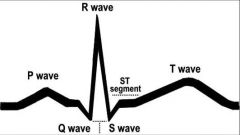
P WAVE
|
|
|
Represents the depolarization of the ventricles . The repolarization of the atria is also buried here
|
The QRS complex
|
|
|
Represents repolarization of the ventricles
|
T WAVE
May be elevated (greater than half the height of the QRS complex) Or depressed (inverted |
|
|
Beginning of P-wave to beginning of QRS
|
PR INTERVAL
|
|
|
Norm for the the PR interval
|
0.12 - 0.20 seconds
3-5 small squares |
|
|
Beginning of the Q wave to the place where the S wave meets the baseline
|
QRS interval
|
|
|
Norm for the QRS interval
|
Normal is less than 0.12 seconds or less than 3 small squares on the paper
|
|
|
From the end of the S wave to the beginning of the T wave
|
ST segment
Flat (normal) Elevated (above baseline) Depressed (below baseline) |
|
|
Beginning of QRS to end of T wave
|
QT interval
|
|
|
Beginning of the R wave if the Q wave is not present to the place where the S wave meets the baseline (or would meet the baseline if it did not curve into the ST segment
|
QRS interval
|
|
|
Normally this interval is less than half the R to R interval of that complex.
|
QT Interval
Called a prolonged QT interval if more than half of the R-R interval |
|
|
Basic Interpretation Guidelines
First, take a general look at the rhythm strip. Are the complexes (in general) the same? Then? |
systematically look at the appearance of P, QRS and T waves, and the ratio of P waves to QRS complexes
|
|
|
Interpreting P-WAVES
Are p-waves ____ in the strip? Are they all ____? Do all p-waves ____ ____? Is there a p-wave before every ___? Are the P to P intervals equal? |
Are p-waves present in the strip?
Are they all upright? Do all p-waves look alike? Is there a p-wave before every QRS? Are the P to P intervals equal? |
|
|
Interpreting PR-INTERVALS
Are PR intervals ____? Are all PR intervals ____? Are all PR intervals within normal limit for ____? |
Are PR intervals present?
Are all PR intervals equal? Are all PR intervals within normal limit for length? |
|
|
originate in the SA node in the right atrium
|
Sinus rhythms
|
|
|
Sinus rhythms originate in the SA node in the right atrium & the impulse follows the ____ ____ ____ through the rest of the heart
|
normal conduction pathway
|
|
|
The only rhythm considered “normal”
|
Normal Sinus Rhythm (NSR)
|
|
|
Normal Sinus Rhythm (NSR)is the only rhythm considered “normal”
Rate: ___-___ Rhythm: ____ The P wave is ____ There is a P wave present for each ___ There is a QRS present for each ___ PR interval: ___-___ QRS interval is: All QRS complexes: |
The only rhythm considered “normal”
Rate 60-100 Rhythm is regular The P wave is upright There is a P wave present for each QRS There is a QRS present for each P wave PR interval range: 0.12 - 0.20 seconds QRS interval is: less than 0.12 All QRS complexes: look alike |
|
|
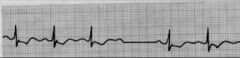
Rate: 50
Rhythm: regular The P wave: upright There is a P wave present for each QRS There is a QRS present for each P wave PR interval range: 0.12 - 0.20 QRS interval is less that 0.12 All QRS complexes look alike |
Sinus Brady
Rate: < 60 Rhythm: regular The P wave is upright P wave for ea QRS QRS for es P PR interval: 0.12 - 0.20 QRS interval: < 0.12 All QRS complexes look alike |
|
|
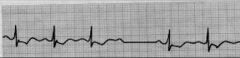
Rate: 120
Rhythm: regular The P wave: upright There is a P wave present for each QRS There is a QRS present for each P wave PR interval range: 0.16 QRS interval: 0.10 All QRS complexes look alike This is? |
Sinus Tachy
Rate: >100 Rhythm: regular P wave: upright P for ea QRS QRS present for ea P PR interval: 0.12 - 0.20 QRS interval: < 0.12 All QRS complexes look alike |
|
|
Occurs when the SA node initiates all the electrical impulses, but at irregular intervals.
|
Sinus Arrhythmia
|
|
|
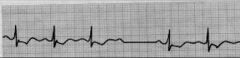
The P wave is upright
There is a P wave present for each QRS and a QRS present for each P wave PR interval range is 0.16 QRS interval is 0.11.08 All QRS complexes look alike This is? |
Sinus Arrhythmia
The P wave: upright There is a P wave present for each QRS There is a QRS present for each P wave PR interval range is 0.12-0.20 QRS interval is less that 0.12 All QRS complexes look alike |
|
|
Generally not serious unless CO decreases &Pt is medically unstable.
|
Sinus arrhythmia
|
|
|
May change with respirations & is normal for infants & young children.
May indicate a diseased SA node or CAD in adults |
Sinus Arrhythmia
|
|
|
An individual complex that occurs earlier than the next expected complex in the underlying rhythm.
Originates from an atrial site outside the SA node. The underlying rhythm is generally sinus. Looks just like the rest of the beats of the strip, but comes early in the rhythm & P wave may look a little different Followed by a pause before the rhythm continues |
Premature Atrial Contraction (PAC)
Must also identify the underlying rhythm |
|
|
Sudden onset tachycardia with a rate greater than 151
Caused by an irritable site in the atria Beats look like the underlying rhythm, but rate is faster Ventricles don’t fill well, so patient may be symptomatic |
Paroxysmal Atrial Tachycardia (PAT)
|
|
|
Paroxysmal Atrial Tachycardia (PAT) is caused by?
|
irritable site in the atria
|
|
|
With Paroxysmal Atrial Tachycardia (PAT) the patient may not feel well because?
|
Ventricles don’t fill well
Must be able to see the beginning of the acceleration to be termed PAT |
|
|
Patient doesn't feel well
Experienced a sudden elevation in HR to 160 On the EKG, beats look like the underlying rhythm but the rate is faster |
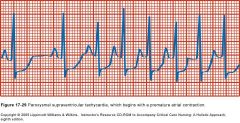
Paroxysmal Atrial Tachycardia (PAT)
Sudden onset tachycardia Rate: >151 Frequently initiated by a PAC Caused by an irritable site in the atria Beats look like the underlying rhythm, but rate is faster Ventricles don’t fill well, so patient may be symptomatic Must be able to see the beginning of the acceleration to be termed PAT |
|
|
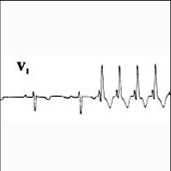
Occurs when a single irritable site in the atria initiates many electrical impulses at a rapid rate.
Impulses are conducted so rapidly that normal P waves are not produced There is not a QRS present for each wave QRS complexes are 0.10 seconds and appear somewhat regularly through the rhythm Rate is 50 |
Atrial flutter
Occurs when a single irritable site in the atria initiates many electrical impulses at a rapid rate Impulses are conducted so rapidly that normal p waves are not produced Saw-toothed, jagged flutter waves appear on the rhythm strip rather than p waves There is not a QRS present for each flutter wave QRS complexes usually are less than 0.12 seconds and appear somewhat regularly through the rhythm |
|
|
Many times the flutter is so regular that it is easy to determine the ratio of waves to QRS complexes
Two F waves/1 QRS is called a ____ Three F waves/1 QRS is called a ____ Ventricular impulses may occur very regularly, so that the rhythm is ____ |
2 :1 block
3:1 block is regular |
|
|
There is no P wave, but rather there is a wavy, fibrillatory line between each QRS
Since there isn't a P wave there is no PR interval |
A FIB
|
|
|
Occurs when there is general increase in irritability of all the cardiac cells of the atria
The atria are not completely depolarized with each impulse and are quivering, not forcefully contracting |
Atrial fibrillation (A fib)
Rhythm: irregular Rate: 350-500 (not a true contraction rate) Every once in a while, an impulse slips through causing a ventricular beat Ventricular rate: < 60 is atrial fibrillation w/slow ventricular response Ventricular rate: 60-100 is called atrial fibrillation Ventricular rate: 101-150 is call atrial fibrillation w/rapid ventricular response Ventricular rate > 150 is called uncontrolled atrial fibrillation |
|
|
Rhythms that start in the AV area are called?
|
Junctional rhythms
|
|
|
This occurs when SA fails to initiate electrical impulses to cause the heart to contract & the AV node acts as a secondary pacemaker though slower & not as efficient as the SA.
|
Junctional rhythms
|
|
|
When an impulse impulse starts in the AV node there may not be a P Wave.
However, the electrical impulse from the AV node can travel back into the SA area causing an impulse. In this case the resultant P wave not “normal.” These characteristic P wave changes are what identify a junctional rhythm. Name the 3 types of abnormal characteristics reflected in an EKG as a result? These characteristic p wave changes are what identify a junctional rhythm |
1-inverted
2-buried 3-retrograde |
|
|
With a junctional rhythm, if the electrical impulse originates high in the AV node, the atria are depolarized rather quickly, but the electrical stimulus moves upward to them, rather than down from the SA node.
This results in what kind of wave? |
inverted
|
|
|
With a junctional rhythm, depolarization of the atria and depolarization of the ventricles take place at closer to the same time. As a result of this, what would you see on an EKG?
|
The PR interval may be shorter in addition to an inverted P Wave
|
|
|
Why would a P wave invert on an EKG?
|
If the electrical impulse originates high in the AV node, the atria are depolarized rather quickly, but the electrical stimulus moves upward to them, rather than down from the SA node
|
|
|
Why would a PR interval be shorter in a junctional rhythm reflecting an inverted P wave?
|
The PR interval may also be shorter because the depolarization of the atria and the depolarization of the ventricles take place at closer to the same time
|
|
|
When an electrical impulse originates more toward the middle of the AV junctional area, the distance the impulse travels back to fire the atria and the distance the impulse moves down to fire the ventricles is more similar. Therefore, depolarization occurs at almost the same time. What is reflected on an EKG as a result of this?
|
Buried P waves
|
|
|
When the electrical impulse originates in the lower part of the AV junctional area, the distance the impulse travels to fire the atria is greater than the distance to fire the ventricles
How will this reflect on an EKG? |
Retrograde P wave
Therefore, the P wave comes after the QRS |
|
|
Occurs when there is a partial or complete interruption in the cardiac electrical conduction system & can occur anywhere in the system.
The resultant tracing will look different depending upon where the interruption occurs. What is this called? |
Heart Blocks
|
|
|
A block that occurs when the electrical impulse traveling from the atria is interrupted at the AV junction & when the interruption becomes longer with each impulse.
This progression continues until an impulse is completely blocked from the ventricles. |

2nd degree heart block
|
|
|
Mobitz I (Wenckebach) block is also known as a?
|
Second degree heart blocks
Proggggrrrrressssssivvve ~ |
|
|
With a 2nd degree heart block (AKA: Mobitz I (Wenckebach))what happens to the PR interval & the QRS?
|
The PR interval gets longer and longer and then there is a P wave with no QRS
|
|
|
With a 2nd degree heart block (AKA: Mobitz I (Wenckebach))what happens to the ventricles?
|
The progression continues until in impulse is completely blocked from the ventricles
|
|
|
With a 2nd degree heart block (AKA: Mobitz I [Wenckebach]) what happens to the electrical impulse traveling from the atria?
|
This block occurs when the electrical impulse traveling from the atria is interrupted at the AV junction and when the interruption becomes longer with each impulse.
|
|
|
Caused by a delay in the conduction of an electrical impulse between the atria and the bundle of His.
All the electrical impulses eventually conduct to the ventricles, but the interruption causes a delay. |
1st Degree Heart Block
|
|
|
How would you expect to see a 1st degree heart block on an EKG?
|
A prolongation of the PR interval (> 0.20 second)
|
|
|
With a 1st degree heart block there is a delay in the conduction of an electrical impulse. Where does this delay occur?
|
atria and the bundle of His.
|
|
|
With a 1st degree heart block there is a delay in the conduction of an electrical impulse. This delay occurs in the atria and the bundle of His. What occurs after this?
|
All the electrical impulses eventually conduct to the ventricles, but the interruption causes a delay.
|
|
|
Mobitz II Heart block is also known as a?
|
2nd degree block.
|
|
|
Occurs with there is an intermittent interruption in the electrical conduction system near or below the AV junction.
What is it called? |
MOBITZ II
|
|
|
A Mobitz II Heart block is is considered a 2nd degree heart block. What would you expect to see on an EKG?
|
Normal PR intervals but suddenly there is a P wave with no answering QRS
|
|
PR intervals are normal, but suddenly there is a P wave with no answering QRS.
What is happening? |
there is an intermittent interruption in the electrical conduction system near or below the AV junction
Mobitz II Heart block (2nd degree heart block) |
|
|
An "AV dissociation" is also known as a?
|
Third Degree heart block
a complete heart block |
|
|
Occurs when the electrical impulse is completely blocked between the atria and the ventricles.
What is this called? |
Third Degree heart block
a complete heart block |
|
|
With a Third Degree heart block what would you expect to see on the EKG strip?
|
It is as if there were two separate hearts beating
The atria impulses show up as P waves The ventricles create there own impulses that show up as QRS complexes, but there is no cause and effect between the two |
|
|
With a Third Degree heart block where is the electrical impulse blocked?
|
between the atria and the ventricles
|
|
|
If there are no impulses coming from the atria or from the junction (or if the ventricles become irritable), what happens?
|
the ventricles can initiate their own impulse
|
|
|
Since the cells of the heart are automatistic, if there are no impulses coming from the atria or from the junction (or if the ventricles become irritable) the ventricles can initiate their own impulse (ventricular beats). How would this be indicated on an EKG strip?
|
wide & bizarre
|
|
|
Since the cells of the heart are automatistic, if there are no impulses coming from the atria or from the junction (or if the ventricles become irritable) the ventricles can initiate their own impulse. This results in funny looking beats. Why?
|
impulse arise far distant from the normal area
|
|
|
What are ventricular beats caused from & how do they look on an EKG?
|
no impulses coming from the atria or from the junction so ventricles initiate their own impulse appearing WIDE & BIZZARE on the EKG.
|
|
|
We know impulses from the SA range from 60-100, and from secondary pace makers such as the AV (40-60) & the HIS-Purkinje sytem (20-40)per/minute. How many impulses a minute does the ventricles produce per minute when impulses are not produced by the atria or the junction?
|
20-40 impulses per minute
Generally this is not enough to sustain life. |
|
|
An individual complex that originates from an area below the bundle of His & occurs earlier than the next expected complex in the underlying rhythm.
This is called? |
Premature Ventricular Contractions (PVC)
|
|
|
PVC’s can have many different configurations. Why is this?
|
It depends on where in the ventricles the impulse arises
|
|
|
What rhythm are the terms belo associated with?
Bigeminal Trigeminal Quadrigeminal Couplet Triplet Run of V tach |
PVC's
|
|
|
three PVC’s in a row is called?
Bigeminal Trigeminal Quadrigeminal Couplet Triplet Run of V tach |
Triplet
|
|
|
A PVC that occurs in every third complex is called?
Bigeminal Trigeminal Quadrigeminal Couplet Triplet Run of V tach |
Trigeminal
|
|
|
more than 3 PVC’s in a row:
Bigeminal Trigeminal Quadrigeminal Couplet Triplet Run of V tach |
Run of V tach
|
|
|
two PVC’s in a row:
Bigeminal Trigeminal Quadrigeminal Couplet Triplet Run of V tach |
Couplet
|
|
|
PVC that occurs every other complex
Bigeminal Trigeminal Quadrigeminal Couplet Triplet Run of V tach |
Bigeminal
|
|
|
PVC that occurs every 4th complex:
Bigeminal Trigeminal Quadrigeminal Couplet Triplet Run of V tach |
Quadrigeminal
|
|
|
A life-threatening dysrhythmia that usually originates from a single site in the ventricles at a rate of 100-125 impulses per minute. This condition is called?
|
Ventricular tachycardia
|
|
|
Why is Ventricular Tachycardia (V tach) a life threatening condition?
|
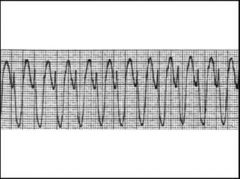
because as the rate increases the ventricles do not have time to empty and refill completely, thereby decreasing the stroke volume and the cardiac output
|
|
|
How many impulses occur per minute in V tach?
|
100-125 impulses per minutes
|
|
|
With V-Tach, as the rate increases the ventricles do not have time to empty and refill completely. This results in?
|
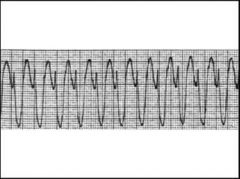
decreasing stroke volume and cardiac output
|
|
|
Sometimes, V tach is started by a PVC that occurs at the same time as the T wave of the previous beat.
This time of repolarization (T wave) is a period of vulnerability when it is easy to cause loss of control. This is known as? |
R on T phenomenon
|
|
|
Sometimes, V tach is started by a PVC that occurs at the same time as the T wave of the previous beat.
This time of repolarization (T wave) is a period of vulnerability when it is easy to cause loss of control. This is known as? |
R on T phenomenon
|
|
|
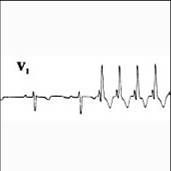
A lethal dysrhythmia in which cardiac cells do not have time to react to one impulse before another one arrives resulting in cardiac chaos. As a result, There is no cardiac output from the rhythm. This is an event called?
|
Ventricular Fibrillation (V fib)
|
|
|
Ventricular Fibrillation (V fib) origiginates from where?
|
many different sites within the ventricles.
|
|
|
With V-Fib, there is no cardiac output from the rhythm therfore, the patient does not have a pulse. Death will occur under these circumstances within what time?
|
minutes
|
|
|
Occurs when there is a complete lack of electrical activity in both the atria and the ventricles. ???
|
Asystole
|
|
|
Asystole appears as a slightly wavy or straight line on the monitor strip?
|
Asystole
|

