![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
xenograft
|
transplant between different species; contains xeno-Ag
|
|
|
allograft
|
same species, but NOT genetically identical; contains allo-Ag
|
|
|
isograft or syngeneic graft
|
same species, IS genetically identical; contains iso-Ag
|
|
|
autograft
|
same species, same individual, different location on the body; contains auto-Ag
|
|
|
What are the two sources of tissue to be transplanted?
|
cadaver, live donors
|
|
|
What are the two biggest crossmatching factors that must be considered between donor and recipient?
|
blood type
HLA |
|
|
What must blood type be considered in a transplant?
|
ABO antigens are expressed on RBCs and endothelial cells of the blood vessels in the donor tissue
|
|
|
What HLA types must match?
|
HLA-A
HLA-B HLA-DR |
|
|
Of the following blood type individuals, from whom can they receive blood:
AB B A O |
AB = A, B, AB, O
B = B, O A = A, O O = O |
|
|
Why would a child never match with their mother or father for HLA haplotypes?
|
HLA haplotypes are expressed codominantly, so they get one (of two) from their mother and one (of two) from their father, both [parents] of which have two to offer. Each child, then, will never match a parent, but will have a 25% chance of matching a sibling - their best chance for family match.
|
|
|
When given the haplotype for A, B and DR, how do you determine the best compatibility given many donors?
|
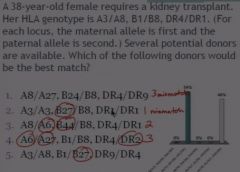
count the number of mismatches
(pic) |
|
|
microtoxicity test
|
used for Class I (HLA A or B) compatibility where lymphocytes from donor or recipients are mixed with HLA antigens to determine which Ags will produce a reaction
|
|
|
mixed lymphocyte reaction
|
Used for Class II (HLA-DR) where lymphocytes from one individual is irradiated and then other individual's cell are added and if there is proliferation, that indicates that the second individual is having an immune response to the first individual
|
|
|
UNOS
|
united network for organ sharing
|
|
|
Which organs are at the highest demand from UNOS?
|
1. kidney
2. liver 3. heart 4. lungs |
|
|
What are the three types of transplant rejection based on host mounting an immune response to donated tissue?
|
1. hyperacute - w/i 24 hrs caused by pre-existing Ab, complement
2. acute - wks to mos caused by T cells 3. chronic - mos to yrs caused by tissue remodeling, fibrosis, T cells |
|
|
What types of pathological processes lead to cell death in hyperacute rejection?
|
a lot of inflammation (see neutrophilic increase) histologically ->
ischemic death cell lysis |
|
|
In what demographic does an acute rejection occur?
|
everyone receiving an allograft to some degree
|
|
|
What are the two mechanisms of Acute Rejection?
|
1. Direct - MHC molecules expressed on donor cells produce T cell response
2. Indirect - MHC molecules secreted by donor cells must be processed by APC, will be expressed on APCs and then a T cell response will occur |
|
|
What cell type would be present histologically in an Acute Rejection scenario?
|
lymphcytes (T cells)
|
|
|
What is the ultimate reason why chronic rejection leads to cell death?
|
remodeling/fibrosis causes ischemia to donated tissue
|
|
|
What is the mechanism of chronic rejection?
|
MHC from donor cells is processed and presented by APC
|
|
|
What is the histological signs of chronic rejection?
|
proliferation of endothelial cells and smooth muscle cells and collagen in and around blood vessels
|
|
|
What is GVHD?
|
Graft-Versus-Host Disease, which most commonly occurs in bone marrow transplant wks to mos after transplant where T-cells from donated tissue attacks recipient cells due to MHC or minor-HC Ag
|
|
|
What three areas of the body will produce symptoms for GVHD?
|
skin - rash
liver - jaundice GI - diarrhea |
|
|
How are pts hindered from mounting an immune response?
|
All transplant pts are forced into immunosuppression:
1. inhibit T-cell proliferation w/ mitotic inhibitors 2. inhibit T-cell activation w/ macrolides & fungal metabolites 3. kill T-cells w/ globulins, monoclonal Abs 4. block cytokine or co-stimulatory molecules w/ corticosteroids |

