![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
101 Cards in this Set
- Front
- Back
|
What are the three major defense systems of the GI tract?
|
1. mucus layer
2. gastric acids 3. food motility |
|
|
What organism causes gastritis, peptic ulcer disease, and gastric carcinoma and is the only infection of the stomach?
|
Helicobacter pylori
|
|
|
What percent of the population is infected with H. pylori?
|
1/3
|
|
|
What are the virulence factors of H. pylori that allows it to be infectious in the stomach?
|
1. flagella to swim through mucosa,
2. adhesins to attach to mucosal lining, 3. makes urease to make ammonia cloud around itself to neutralize stomach acid |
|
|
What is the clinical presentation of gastritis?
|
inflammation of stomach mucosa is usually caused by H. pylori and are usually asymptomatic, but sometimes presents with gastric pain
|
|
|
What is the clinical presentation of peptic ulcer disease?
|
epigastric pain that occurs 1 to 5 hours after eating
|
|
|
What are the two primary causes of peptic ulcer disease?
|
1. H. pylori
2. NSAIDs |
|
|
How is H. pylori diagnosed?
|
1. biopsy (invasive)
2. urease test 3. silver stain 4. ELISA test (most common) |
|
|
What is the Tx for H. pylori stomach infections?
|
1. amoxicillin, erythromycin
2. proton pump inhibitor |
|
|
What are the five risk factors of diarrhea?
|
1. blood in stool
2. fever 3. abdominal pain 4. extent of dehydration 5. epidemiology |
|
|
What is the major difference in Tx for self-limiting watery diarrhea and dysentery?
|
self-limiting watery diarrhea only requires supportive care but no antibiotics
|
|
|
What are you not likely to see in watery diarrhea stools?
|
blood, mucus, pus
|
|
|
What is significant about the way that watery diarrhea causing pathogens attach to the GI mucosa?
|
they attach but do not invade and cause inflammatory reactions
|
|
|
What causes the watery diarrhea itself after a bacterial infection?
|
enterotoxin, which increases fluid loss to the lumen of the small intestine
|
|
|
What symptoms are common with Staph. aureus food poisoning?
|
2-6 hours after ingestion of staphylococcal enterotoxin riddled food there is vomiting, diarrhea and abdominal pain. lasts less than 24 hrs.
|
|
|
What are the most common contaminated products of Staph. aureus food poisoning?
|
ham and dairy products
|
|
|
What is significant about the Staph. aureus enterotoxin?
|
1. heat-stable, so can't heat and destroy
2. superantigen |
|
|
Why would antibiotics not be helpful to resolve Staph. aureus food poisoning?
|
it's not caused by bacteria directly. it's caused by enterotoxin
|
|
|
Tx for Staph. aureus food poisoning?
|
maintain hydration
|
|
|
What two types of disease is caused by Bacillus cereus?
|
1. Emetic - vomiting
2. Diarrheal - diarrheal |
|
|
What are the symptoms of emetic disease caused by Bacillus cereus?
|
Within 6 hrs of ingesting Bacillus cereus spore containing food (usually rice) pt experiences vomiting, nausea, abdominal craps for about 24 hrs.
|
|
|
What is the causative agent of emitic disease related to Bacillus cereus? It's not directly B. cereus.
|
Bacillus cereus produces a spore that after it germinates produces a toxin. The toxin is heat resistant.
|
|
|
What type of food is generally infected with Bacillus cereus spores that cause emetic disease?
|
rice
rice rice think cereal think cereus |
|
|
What are the symptoms of diarrheal disease caused by Bacillus cereus?
|
After 8 - 12 hours of ingestion of B. cereus spores or vegetative cells in meat, veggies or sauces pt experiences watery diarrhea and abdominal cramps for about 24 hrs.
|
|
|
What is the causative agent of diarrheal disease caused by Bacillus cereus?
|
spores or vegetative cells produced by B. cereus that produce an enterotoxin
|
|
|
What type of food is generally infected with Bacillus cereus spores and vegetative cells that cause diarrheal disease?
|
meat, VEGGIES, sauces
VEGGIES because vegetative cells as well as spores as a differential between this an emeitc |
|
|
What treatment is warranted for both emetic and diarrheal Bacillus cereus food related disease?
|
supportive to prevent dehydration. no antibiotic.
|
|
|
What virulence factor allows for diarrheal disease caused by Bacillus cereus?
|
attachment to mucosal lining
|
|
|
What is significant about Clostridium perfringens food related diarrhea?
|
It is a true bacterial infection that causes symptoms. Symptoms are caused by the enterotoxin, and since it's self-limiting antibiotics are not used. But the infection is caused by bacterially infected foods.
|
|
|
What food products cause Clostridium perfringens related GI infection?
|
meat and meat products
|
|
|
What is unique about the Clostridium perfringens caused GI infections?
|
It's caused by ingesting the bacteria, itself. This means that it can be killed by heating the food long enough before eating.
|
|
|
What symptoms present with Clostridium perfringens GI infections?
|
8 hrs to 1 day after ingestion of contaminated meat products pt has diarrhea for no longer than 1 day.
|
|
|
Since Clostridium perfringens GI infections is caused by bacterial ingestion, should tx include antibiotics?
|
NO. Symptoms, themselves, are caused by toxin released after infection, but regardless, this infection is self-limiting and tx should just be supportive.
|
|
|
What does ETEC stand for?
|
Enterotoxigenic E. coli
|
|
|
What are the two endotoxins produced in the small intestine caused by ETEC?
|
AB3 Heat labile LT-1 - increase adenylate cyclase activity (cAMP)
Heat stable STa - increases guanylate cyclase activity (cGMP) both carried on conjugative plasmids |
|
|
What foods are commonly contaminated with ETEC?
|
fruit, vegetables, water
|
|
|
What demographic is most commonly infected with ETEC GI infections?
|
travelers
children |
|
|
What is the Tx for ETEC?
|
self-limiting, so supportive
lasts for no more than 5 days NO antibiotics |
|
|
What is the difference between food poisoning and foodborne infection?
|
food poisoning - ingestion of toxin
foodbourne infection - ingestion of toxin producing bacteria |
|
|
Why should you not feed infants honey?
|
Honey often contains Clostridium botulinum spores and will give infants foodbourne infection.
|
|
|
What does EPEC and EAEC stand for?
|
Enteropathogenic E. coli
Enteroaggregative E. coli |
|
|
Are EPEC and EAEC food bourne infections or food poisoning?
|
foodbourne infections
|
|
|
What demographic is most commonly infected by EPEC and EAEC?
|
travelers
developing countries |
|
|
What functionally causes EPEC and EAEC symptoms?
|
EPEC and EAEC organisms will disrupt the small intestine microvillus and prevent water absorption. can be chronic
|
|
|
What is the Tx for EPEC, EAEC foodbourne infections?
|
supportive. NO antibiotics
|
|
|
What does EHEC stand for?
|
Enterohemorrhagic E. coli
|
|
|
What foods are EHEC found in?
|
cattle product:
beef, beef product, unpasteurized milk juice, water, vegetables |
|
|
What is the most common strain of EHEC causing infection?
|
O157:H7
|
|
|
What is unique about EHEC demographic and pathogenicity?
|
> 100,000 cases in the US a year
person to person spread (fecal-oral) zoogenic spread (petting zoos, even) |
|
|
What causes symptoms from EHEC?
|
Shiga-like toxin (AB5) which destroy villus by inhibiting protein synthesis and causes less water absorption
|
|
|
What are common symptoms from EHEC?
|
diarrhea, abdominal pain, vomiting, fever, bloody diarrhea after 2 days (hemorrhagic colitis)
symptoms last 4 - 10 days and are self-limiting |
|
|
What clinical findings will be present with EHEC?
|
NO fecal leukocytes, so you can tell that this is NOT dysentery
|
|
|
What is the EHEC Tx?
|
NOT antibiotics
just supportive |
|
|
What is the significance of Hemolytic Uremic Syndrome?
|
complication of EHEC affecting children causing microangiopathic hemolytic anemia (small blood vessels are blocked caused by Shiga-like toxin), thrombocytopenia (lack of platelets), acute renal failure
|
|
|
What is the relationship to renal impairment and EHEC?
|
If you a pt has EHEC, be aware that HUS can be a complication, and be cognizant of renal symptoms to catch HUS early.
|
|
|
What foods are Vibrio cholerae found in?
|
raw or undercooked shellfish as well as infected water
|
|
|
What symptoms are common with Vibrio cholerae GI infection?
|
watery "rice water" diarrhea (milky white watery)
vomiting |
|
|
What is the primary defense against Vibrio cholerae?
|
gastric acid. so for patients with low gastric acidity, much less Vibrio cholerae is needed to be infectious
|
|
|
What strains of Vibrio cholerae that cause cholera?
|
O1 (El Tor in US)
O139 |
|
|
What does Vibrio cholerae do cause symptoms?
|
Increase cAMP levels, increasing water and chloride secretion into the lumen.
|
|
|
What is the Tx of Vibrio cholerae infection?
|
Antibiotics
Rehydration/supportive |
|
|
What is the leading cause of gastroenteritis in the US?
|
Vibrio parahaemolyticus
|
|
|
What foods does Vibrio parahaemolyticus reside in?
|
undercooked or raw shellfish
|
|
|
What symptoms are common with Vibrio parahaemolyticus infection?
|
watery diarrhea, abdominal cramps, nausea, vomiting, fever, bloody diarrhea, headache
NO fecal leukocytes |
|
|
What two symptoms should concern you and cause you to do a work-up to differentiate between diarrhea and dysentery?
|
bloody stools
fever |
|
|
What is the Tx for Vibrio parahaemolyticus?
|
rehydration/supportive
|
|
|
What Genus species do ALL Salmonella belong?
|
Salmonella enterica has thousands of serotypes but are all enterica species
|
|
|
What is non-typhoidal Salmonella?
|
All Salmonella except typhi and paratyphi Salmonella
|
|
|
In which foods are non-typhoidal Salmonella found?
|
poultry, eggs, dairy, water
|
|
|
What routes of transmission is Salmonella infectious?
|
fecal-oral
food |
|
|
How does Salmonella infect the host?
|
phagosomes engulf Salmonella in small intestine, bacteria replicate in phagosome, localized inflammation, increase in cAMP, watery diarrhea
|
|
|
How does severe Salmonella present?
|
bloody stool with NO fecal leukocytes
|
|
|
What are common symptoms associated with Salmonella?
|
nausea, vomiting, diarrhea, abdominal cramping, fever, bloody stools
|
|
|
What is the Tx for Salmonella GI infections?
|
supportive/rehydration
Antibiotics for at risk patients |
|
|
What is the differential of Dysentery?
|
frequent stools (not necessarily watery)
fecal leukocytes mucus bloody stools large intestine infection and tissue damage that causes mucus, blood, leukocytes in the stool |
|
|
EIEC stands for what?
|
Enteroinvasive E. coli
|
|
|
What is the most common food source for EIEC infection?
|
imported cheese
|
|
|
What is the most common clinical presentation of EIEC?
|
watery diarrhea
|
|
|
What is the severe clinical presentation of EIEC?
|
fever, abdominal cramps, blood
|
|
|
What is the Tx for EIEC caused dysentery?
|
common: supportive
severe: antibiotic |
|
|
How is Campylobacter jejuni transmitted?
|
poultry, unpasteurized milk, people to people, pets
|
|
|
What is the clinical presentation of C. jejuni?
|
large range
|
|
|
When sending a suspected C. jejuni infected sample to the lab, what special consideration should be taken into account?
|
Campylobacter are microaerophiles.
5% O2, 10% CO2 |
|
|
What is the Tx for C. jejuni?
|
supportive
|
|
|
What are the two complications of C. jejuni?
|
Guillain-Barre syndrome
reactive arthritis |
|
|
What demographic is most commonly infected by Yersinia enterocolitica?
|
children < 1 year old
|
|
|
What food products are most commonly infected by Yersinia enterocolitica?
|
food, milk, water
|
|
|
What is the main differential of Yersinia enterocolitica?
|
appendicitis
|
|
|
What is the clinical presentation of Yersinia enterocolitica infection?
|
watery, mucoid diarrhea, abdominal pain, fever, bloody stools, fecal leukocytes, bacteremia
|
|
|
What complication should one be aware of with infants younger than 3 months diagnosed with Yersinia enterocolitica?
|
20 - 30% experience bacteremia
|
|
|
What are the two causative agents that cause 90% of Shigella infections in the US?
|
Shigella sonnei and Shigella flexneri
|
|
|
What is unique about Shigella foodborne infection?
|
highly contagious between people
|
|
|
What causes Shigella infection?
|
people to people, food, water
|
|
|
How is diagnosis of Shigella confirmed?
|
culture on a special media.
|
|
|
What is the Tx for Shigella?
|
Infected people need only supportive therapy for themselves, but they are also treated with antibiotics in order to stop transmission to others.
|
|
|
What is unique about Clostridium difficile GI infection?
|
It is usually associated with overgrowth due to antibiotic treatment
|
|
|
How does Clostridium difficile cause problems in the GI tract?
|
Clostridium is endospore forming which produces Toxin A and Toxin B causing colonic mucosa inflammation and fluid secretion
|
|
|
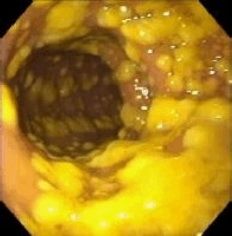
What is the clinical presentation of Clostridium difficile?
|
profuse, mucoid, greenish, malodorous water stools, fever, abdominal pain.
rarely: pseudomembrane may form (pic) in the colon or toxic megacolon |
|
|
What is the gold standard of Clostridium difficile?
|
isolate the pathogen and determine if this strand is producing the toxin, but that takes 3 days
|
|
|
What is more practical than the gold standard of Clostridium difficile when diagnosing?
|
rapid test kits, but they have low sensitivity (77%)
|
|
|
What treatment must one know for treatment of Clostridium difficile GI infection?
|
metronidazole first
vancomycin if metronidazole is not effective |

