![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
Why can large bacteria not infect the respiratory tract usually, and how do they get around the normal defense mechanism?
|
they usually get caught in the mucus layer in the upper respiratory tract, are moved back to the throat and swallowed.
they evade this by 1) anchoring to the mucosa, 2) inactivate the cilia that would normally mobilized them to the throat |
|
|
Why can small bacteria not infect the respiratory tract, usually, and how do they get around the normal defense mechanisms?
|
in the alveoli there are alveolar macrophages that take care of these bad boys
they evade this by 1) reproducing inside of the macrophages that engulf them |
|
|
Pharyngitis is caused by what bug most commonly?
|
Strep. pyogenes, but viruses cause most sore throats
|
|
|
Why should you not immediately jump to antibiotic treatment with a "sore throat?"
|
because they are usually caused by viruses. this is especially true if there is a cough or runny nose which are not present in a Strep. exclusive infection.
|
|
|
What is the most important virulence factors of Strep. pyogenes in pharyngitis?
|
M-protein that anchors Strep. into the throat
|
|
|
How can you verify the presence of Strep. pyogenes in the lab?
|
80% sensitivity rapid antigen test
culture |
|
|
What is the primary demographic of Strep. pyogenes pharyngitis?
|
children. rare in adults.
|
|
|
What are the complications of improperly or untreated Strep. pyogenes?
|
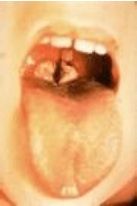
peritonsillar abscess, otitis media, sinusisits, mastoiditis, Scarlet fever, erythematous butterfly rash on the face, rheumatic fever, glomerulonephritis, white tongue -> red tongue caused by infection and then sloughing.
|
|
|
What causes Scarlet fever?
|
Strep. pyogenes carried lysogenic phage producing pyrogenic endotoxin. This is not carried by all strains of Strep. pyogenes
|
|
|
What is the cause of Rheumatic Fever?
|
One cause of this autoimmune disease is a complication of Strep. pyogenes pharygitis. Antibodies formed to the Strep. cell wall cross-react with human tissues, especially the heart.
|
|
|
What are the symptoms of Rheumatic Fever?
|
sore throat 2 to 6 weeks prior
polyarthritis or carditis Rheumatic heart disease heart failure |
|
|
What is the tx for Rheumatic Fever?
|
prophylactic penicillin is given to prevent further attacks by Strep. pyogenes. you cannot kill the antibodies responsible for Rheumatic Fever.
|
|
|
What annual life events must be proceeded with penicillin in a Rheumatic Fever patient?
|
visits to the dentist
|
|
|
What is the reasoning for acute glomerulonephritis caused secondarily by Strep. pyogenes pharyngitis?
|
Ag-Ab complexes deposited into the glomeruli leading to inflammation
|
|
|
What are the two most often encountered Haemophilus influenzae?
|
non encapsulated
type b |
|
|
How is Haemophilus influenzae type b transmitted?
|
respiratory droplets
|
|
|
What are the two diseases caused by Haemophilus influenzae type b?
|
Epiglottitis and Meningitis
|
|
|
How does epiglottitis progress?
|
rapidly progressing sore throat, fever causing swelling of the epiglottis -> difficulty breathing and swallowing
|
|
|
What is the vaccine that can prevent epiglottitis?
|
Hib
|
|
|
What are the 4 bugs that can cause epiglottitis in children?
|
Haemophilus influenzae type b, Haemophilus parainfluenzae, Staphylococcus aureus and Streptococcus pneumoniae
|
|
|
What is the most common demographic for current day epiglottitis?
|
adults
|
|
|
What is the most common demographic for current day meningitis?
|
children (who have not been vaccinated)
|
|
|
What is the causative agent of Diphtheria?
|
Corynebacterium diphtheriae infection of the upper respiratory tract.
|
|
|
What strain of Corynebacterium diphtheriae that causes diphtheria?
|
ones that carry the "tox" gene on a lysogenic phage of which produces A-B exotoxin. phage!
|
|
|
What is the significance of a diphtheria related exudate?
|
hallmark physical characteristic which leads to a pseudomembrane covering the tonsiles, uvula, palate and will cause bleeding when removed
|
|
|
How can diphtheria cause systemic problems?
|
The exotoxin A-B can cause cardiac and neurological issues.
|
|
|
What is the causative agent of Pertussis Whooping Cough?
|
Bordetella pertussis, Gram (-) bacillus
|
|
|
What is the most common demographic for Pertussis?
|
adult
|
|
|
How is Pertussis spread?
|
respiratory droplets
|
|
|
What strain of Pertussis is problematic?
|
1) AB5 exotoxin producing strains which causes increase of cAMP levels -> excessive respiratory secretions and mucus.
2) tracheal cytotoxin producing strains that inhibit cilia movement |
|
|
What are the three stages of Pertussis?
|
1) Catarrhal stage - 1-2 wks of runny nose, sneezing, low grade fever
2) Paroxysmal stage - 2-4 wks of whooping cough, vomiting, exhaustion from cough 3) Covalescent stage - several wks of chronic cough |
|
|
What is a less common causative agent of Pertussis?
|
Bordetella parapertussis
|
|
|
What are the 4 upper respiratory tract infection causing bugs and their corresponding diseases?
|
1) Strep. pyogenes - pharyngitis -> scarlet fever, rheumatic fever, acute glomerulonephritis
2) Haeomophilus influenzae type b - epilottitis, meningitis 3) Corynebacterium diphtheriae - Diphtheria 4) Bordetella pertussis - pertussis |
|
|
What pathogens cause typical pneumonia?
|
1) Strep. pneumoniae
2) Haemophilus influenzae (non-encapsulated) 3) Moraxella catarrhalis |
|
|
What pathogens cause atypical pneumonia?
|
1) Legionella pneumophila
2) Mycoplasma pneumoniae 3) Chlamydophila pneumoniae |
|
|
What is the strict definition of pneumonia?
|
fluid in the lungs
|
|
|
What is differentiating between typical and atypical pneumonia?
|
typical - without extrapulmonary findings
atypical - with extrapulmonary findings |
|
|
What broad category of pathogens cause typical pneumonia?
|
opportunistic pathogens
|
|
|
What is significant features of Strep. pneumoniae in regard to Pneumonia?
|
1) normal flora of nasopharynx
2) opportunistic 3) multiply in alveoli after viral infection |
|
|
What are the symptoms and complications of Strep. pneumoniae caused Pneumonia?
|
fever, cough, chest pain, otitis media, sinusitis, bacteremia, meningitis
|
|
|
What is the significant features of H. influenzae (non-encapsulated) in regard to Pneumonia?
|
1) normal flora of nasopharynx
2) opportunistic |
|
|
What preceding conditions are common to an opportunistic H. influenzae (non-encapsulated) infection causing Pneumonia?
|
COPD, upper resp. viral infections, cycstic fibrosis
|
|
|
What is significant about Moraxella catarrhalis in regard to Pneumonia?
|
1) normal flora of nasopharynx
2) opportunisitc 3) can cause otitis media and sinusitis |
|
|
What demographic is more common for Moraxella catarrhalis infections that lead to Pneumonia?
|
children, immunocompromised, COPD
|
|
|
What are the symptoms for atypical pneumonia caused by Mycoplasma pneumoniae?
|
fever, malaise, headache, sore throat, nasal congestion, non-productive cough, pneumonia
|
|
|
How does Mycoplasma avoid removal in respiratory infection?
|
adhesins allow anchoring, bacterium kills cilliated epithelial cells preventing its removal
|
|
|
What is Legionnaires Disease?
|
atypical pneumonia caused by Legionella pneumophila
|
|
|
How is Legionnaires disease transmitted?
|
inhalation of contaminated water vapor - if a lot of people in one building get this at the same time, then it could be in the air conditioning
NOT person to person! |
|
|
How does Legionnaires disease avoid removal by the immune system?
|
phagocytosed by macrophage in alveoli and multiplies in macrophage
|
|
|
What is Pontiac fever?
|
a mild form of the same causative agent of Legionnaires disease (Legionella pneumophila) that does not lead to pneumonia
|
|
|
What two causative agents are the 3rd most common cause of atypical pneumonia and are part of the Chlamydophila genus?
|
Chlamydophila pneumoniae
Chlamydophila psittaci which used to be Chlamydia pneumoniae and Chlamydia psittaci |
|
|
Recall the life cycle of Chlamydophila (and Chlamydia for that matter).
|
EB -> RB -> EB
|
|
|
What is significant about pneumonia related Chlamydophilia pneumoniae infection?
|
transmitted by respiratory droplet from person to person
usually asymptomatic, but can cause severe form and have high mortality |
|
|
What is significant about pneumonia related Chlamydophilia psittaci infection?
|
Referred to as ornithosis
transmitted from birds resp droplets or from direct contact asymptomatic to severe |
|
|
What is the causative agent of tuberculosis?
|
Mycobacterium tuberculosis, mycolic acid producing, non-gram staining, acid-fast staining
|
|
|
How is tuberculosis causing Mycobacterium tuberculosis transmitted?
|
respiratory droplets
|
|
|
How do they avoid the body's immune defense?
|
replicate in macrophages
|
|
|
Three possible outcomes of primary infection of tuberculosis causing Mycobacterium tuberculosis?
|
1) bacteria are killed by granuloma and everything is A-OK
2) bacteria overwhelm immune system and spread through lungs, blood, lymph causing cough, fever, weight loss, fatigue, bloody cough 3) bacteria and body stalemate where bacteria is encompassed in granuloma encapsulated by fibrin. bacteria don't die, and don't spread. 10% chance to escape from granuloma and spread |
|
|
Antibiotic Tx for Tuberculosis?
|
1) regular flavored TB - use 4 antibiotics for at least 6 months
2) MDR-TB (multi-drug resistance) - 4 different antibiotics for 18 months 3) XDR-TB (extremely drug resistant) - uh oh |

