![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
cognitive disability
|
An impairment that affects an individual's awareness and memory as well as ability to learn, process information, communicate and make decisions
|
|
|
|
crackles
|
High pitched breath sounds formerly referred to as railes that indicate lower airway pathology such as pneumonia or asthma
|
|
|
|
epiglottitis
|
A baterial infection of the epiglottis and supraglottic structures also cold acute supraglottitis
Typically affects children 2 to 7 years old No seasonal preference has been detected Rapid onset of symptoms 6 to 8 hours Can quickly progress to respiratory arrest Quiet wet stridor (is a late sign) muffle voice difficulty swallowing preference for setting up right and characteristic of supraglottic disorders absence of a cough is an important diagnosis clue Sudden onset of high fever 102-104 increased heart rate and ventilatory rate Typically no other family members are ill with an acute upper respiratory illness Intervention: do not examine the oropharynx Do not administered anything by mouth Maintain an oxygen saturation of 94% or higher |
|
|
|
greenstick fracture
|
The incomplete fracturing of an immature bone
|
|
|
|
gurgling
|
Abnormal respiratory sound associated with collection of liquid or semi-solid material in the patient's upper airway
|
|
|
|
grunting
|
a short low pitch sound heard at the end of exhalation that represents and attempt to generate positive endexpiratory pressure by exhaling against a closed glottis, prolonging the period of oxygen and carbon dioxide exchange across the alveolar capillary membrane, a compemsatory mechanism to help maintain patency of small airways and prevent atelectasis
|
|
|
|
head bobbing
|
Indicator of increase work of breathing in infants , the head falls forward with exhalation and comes up with expansion of the chest on inhalation
|
|
|
|
hyperpnea
|
Increase respiratory rate or deeper than normal breathing
|
|
|
|
hypoxemia
|
Insufficient oxygenation of the blood a decrease in the arterial blood oxygen tension in adults children and infants older than 28 days hypoxemia is defined as an arterial oxygen tension (PaO2) of less than 60 mmhg or arterial oxygen saturation (SaO2) of less than 90% in an individual breathing room air or with PaO2 and/or SaO2 below the desirable range for a specific clinical situation
|
|
|
|
petechiae
|
A tiny pinpoint rash on the upper area of the neck and the face may indicate near strangulation or suffocation caused by an occlusion of venous return from the head while arterial pressure remains normal ;may be present in mothers after childbirth reddish purple, nonblanchable discolorations in the skin less than 0.5 cm in diameter
|
|
|
|
purpura
|
Reddish purple nonblanchable discolorations greater than 0.5 cm in diameter large purpura are called ecchymosis
|
|
|
|
Respiratory failure
|
A clinical condition of inadequate blood oxygenation and /or ventilation to meet the metabolic demands of body tissues
|
|
|
|
retractions
|
Use of accessory muscles of respiration to assist in ventilation during times of distress sinking in of the soft tissues above the sternum or clavicle or between or below the ribs during inhalation
|
|
|
|
Accessory muscle
|
Muscles of the neck chest and abdomen that become active during labor breathing
|
|
|
|
Bacterial tracheitis
|
Inflammation of the mucus membrane of the trachea.
Complicated by copious thick pus filled secretions Life threatening illness is now more common than epiglottitis. Can occur at any age and in any season. 50% of children with bacterial tracheitis have an associated pneumonia. Patient frequently have several day history of viral upper respiratory symptoms such as fever cough stridor similar to croup This may be followed by a rapid onset of high fever respiratory distress and a toxic appearance. Interventions: maintain an oxygen saturation of 94% or higher if required endotracheal intubation should be performed with an endotracheal tube 0.5 to 1 mm smaller than that calculated for age because of swelling and inflammation frequent suctioning often is necessary to maintain the patency of the tube |
|
|
|
tripod position
|
Position use to maintain airway patency sitting upright and leaning forward with the neck slightly extended chin projected and mouth open and supported by the arms
|
|
|
|
Compensated shock
|
Any pediatric patient with signs of inadequate the peripheral (distal) perfusion which may include:
Altered mental status (e g agitation confusion) Increase pulse rate (tachycardia) Pale skin (pallor) Cool cyanotic lower extremities Delayed capillary refill Blotchy skin (mottling) weak or absent peripheral (distal ) pulses radial, tibial, pedal note: definition of shock in the pediatric patient doesn't depend upon blood pressure |
|
|
|
decompensated shock
|
Any pediatrics stations having a systolic blood pressure below. 7o mm/hg + 2 x in years or the following signs of inadequate central (proximal) perfusion
Altered mental status (lethargy, coma) Extensive cyanosis of all extremities Weak or impalpable central (proximal) pulses (femoral,brachial,carotid) |
|
|
|
Primary prevention
|
Involves measures that can be applied in advance to reduce the likelihood that an injury will occur
|
|
|
|
Secondary prevention
|
Includes interventions that help prevent or minimize an injury when it happens
|
|
|
|
tertiary prevention
|
Traditionally the prehospital professional's role in injury management has focus on emergency care of the victims after injuries occur
Measures lessen the severity of an injury and improve the patient's outcome after an injury such as advanced trauma care and rehabilitation |
|
|
|
Pediatric assessment triangle (PAT)
|
Summarize is the major points for the general impression assessment it is perform before approaching or touching the child (across the room survey)
It is a useful tool for quickly determining whether a child is sick or not sick 3 mean areas of assessment the PAT Appearance : refets to the child's mental status ,muscle tone and body position. Breathing : includes the presence or absence of visible movement at the chest or abdomen and signs of breathing efforts. Circulation: refers to the child's skin color. |

|
|
|
Circulation assessment
|
Significant internal bleeding may occur in the chest abdomen pelvis retroperitoneum and femoral areas.
Compare the strength and quality of the central and peripheral pulses although a peripheral pulse is not quite as strong as a central poles the rate should be the same. A weak central pulse may indicate decompensated shock. A peripheral pulse that is difficult to find, weak or irregular suggests poor peripheral perfusion and may be a sign of shock or hemorrhage. Decrease skin perfusion is an early sign of shock. Pale skin maybe observe and shop for respiratory failure. Cool, pale extremities are associated with decreased cardiac output as seen in shock and hypothermia. Blue cyanosis skin suggest hypoxemia or inadequate perfusion. Mottled skin suggest decreased cardiac output ischema and hypoxia but can be normal in an infant exposed to a cold environment. |
|
|
|
skin turgor (elasticity)
|
Good skin turgor indicates adequate hydration
poor skin turgor a sign of dehydration and or malnutrition Other signs of dehydration include dry mouth sunken eyes and absence of tears when crying and sunken or depressed fontanelles Capillary refill time of 3 25 seconds is delayed and may indicate poor perfusion or exposure to cold ambient temperatures Capillary refills time greater than 5 seconds is markedly delayed and such as shocked |
|
|
|
Foreign body fairway obstruction
|
May be seen at any age but children younger than 5 years are specially vulnerable.
signs/symptoms sudden onset of respiratory distress abnormal respiratory sounds including wheezing, inspiratory stridor or decrease breath sounds coughing or gagging, agitation and or cyanosis |
|
|
|
croup laryngotracheobronchitis
|
It is viral respiratory infection that affects the upper respiratory tract. the area below the glottis is most commonly affected resulting in swollen ,inflammed mucosa with associate it horseness, inpiratory stridor and a barking cough
Respiratory syncytial virus (RSV) most common in patients younger thatn 5 years affects comes children aged 6 months to 3 years,peaking at 2 years. RSV has a midwinter peak increasing numbers in spring croup is spread person to person or large droplets and contaminated nasopharyngeal secretions incubation period is 2 to 4 days s/s: URI for 1 to 2 days but may be spadmodic ( usually wakes from nap or sleep). its usually worst at night or when child is agitated. v/s : increased ventilatory rate and heart rate, low grade fever usually less than 102.2 degrees interventions: do not examine the oropharynx maintains spo2 og 94% ( oxy meter may be inaccurate due to large degree of upper airway obstruction is required to produce hypoxia in an other wise healthy child If child has mild croupmedical directions may instruct you to give nabulized saline moderate or severe nebulized racemic or levo-epinephrine |
|
|
|
Asthma
|
Is a reversible obstructive airway disease characterized by chronic inflammation hyperactive airways and episodes of bronchospasms.
Is the most common pediatric chronic disease. s/s: wheezing most common symptom dry cough chest tightness shortness of breath with exertion retractions tachypnes poor air entry prolong expiratory phase Interventions: aerosolized bronchodilators |
|
|
|
bronchiolitis
|
Is an inflammation of the smaller bronchioles caused by a virus . it is characterized by thick mucus inflammation and swelling make the small air passages in infants particularly vulnerable to obstruction.
Airway obstruction is usually gradual. RSV is the primary cause of bronchiolitis and pnuemonia in children younger than one year. infection can affect any part of the respiratory tract. is highly contagious and is spread from respiratory secretion close contact less than 6 feet with infected persons or contact with contaminated surfaces or objects. RSV occurs in yearly epidemics in mild climates, each winter and last four to five months. Most common in infants younger than 1 year of age Infants 1 to 4 months of age are at particular risk of severe infection and hospitalization s/s: low grade fever ,upper respiratory infection with runny nose and cough for several days, increasingly productive cough, increasing respiratory distress, ear infection, family history of asthma and allergies, contact with older siblings or children at daycare who have viral respiratory symptoms. Auscultation often reveals diffuse rhonchi fine rails or crackles and wheezes. Tachypnea and tachycardia often are present.signs of dehydration. Signs of severe life-threatening illness include nasal flaring retractions ,central cyanosis , tachypnea more than 70 breaths per minute listlessness and apnes spells the chest may be hyper expanded and almost silent on auscultation because of poor air exchange. |
|
|
|
Pneumonia
|
Is in inflammation and infection of the lower airway and lungs caused by a viral,bacterial, parasitic or fungal organism may occur as a primary infection or secondary to another illness or infection.
most common cause is RSV in infants respiratory viruses in children younger than 5 years Most prevalent in winter months Austin proceed my symptoms of an upper respiratory infection may include fever, malaise, anorexia and chest pain |
|
|
|
shock (hypoperfusion)
|
Is the inadequate circulation of blood through an organ or a part of the body.
Hypertension is a late sign of cardiovascular compromise in an infant or child |
|
|
|
hypovolemic shock
|
May be caused by a loss of blood ,plasma, fluids and electrolytes or by endocrine disorders.
Plasma loss may be caused by burns or third spacing as in (pancreatitis or peritonitis) Fluid and electrolyte loss may be from a kidney disorder excessive sweating cystic fibrosis diarrhea vomiting or dehydration. Shock also may be caused by endocrine disorders such as diabetes mellitus or hypothyroidism. s/s may include internal or external bleeding poor skin turgor decreased saliva and or tears or sunken fontanelle ( in infants). Interventions Maintain oxygen saturation at or greater than 94% Immediate vascular access is needed. Signs of shock should be treated with a bolus of 20 ml/kg of isotonic crystalloid normal saline or lactated Ringer's solution even if the blood pressure is normal. Check glucose levels if glucose is less than 60 mg d l administer iv dextrose. maintain temperature |
|
|
|
Distributive shock
|
Maybe cause buy a severe infection (septic shock)
Severe allergic reaction (anaphylactic shock) Spinal cord injury (neurogenic shock) or certain overdose is example sedatives , narcotics |
|
|
|
Septic shock
|
Suspect septic shock when a child with fever tachycardia and vaso dilation experiences changes in mental status.
septic shock occurs in 2 clinical stages early stage peripheral vasodilation (warm shock) is present the late stage (decompensated) is characterized by cool extremities (cold shock), late septic shock is usually indistinguishable from other types of shock. Most patients in decompensated septic shock required aggressive fluid administration. Carefully monitor the patience for crackle signing please work a breathing when given fluids is trials condition does not approve with fluids medical direction me order a dopamine or epinephrine i_v infusion i_v antibiotics will be given at the hospital. |
|
|
|
anaphylactic shock
|
Occurs when an individual is exposed to a substance to which the patient has been previously sensitized. on reexposure to the same substance histamine and other chemical mediators are released which produce the signs and symptoms of anaphylaxis.
epinephrine is usually ordered (site of choice is lateral aspect of the thigh) Other medications that may be ordered include bronchodilator therapy albuteral ,an antihistamine Dyphenhydramine and a steroid methylprednisolone or dexamethasone medical direction may order epinephrine iv and fluid boluses of normal saline or Ringer's lactate. Check glucose if less 60 m_g d l administered dextrose |
|
|
|
neurogenic shock
|
Caused by a severe injury to the head or spinal cord that results in a loss of sympathetic vascular tone below the level of the spinal cord injury .the loss of peripheral vascular tone results in widespread vasodilation between the level of the injury the total blood volume remains the same but vessel capacity is increased (relative hypovolemia)
Interventions cervical spine stabilization and administer oxygen maintainboxygen saturation greater than 94 percent IV access give a 20 ml/kg isotonic crystalloid solution normal saline or Ringer's lactate fluid bolus as ordered by medical direction if condition does not improve repeat boluses maintainbody temperature shock widespread vasodilation may result in loss of body heat be aware of possible hypothermia serum glucose if less than 60 mg/dl administer IV dextrose ,may be ordered vasopressors if poor perfusion despite adequate ventilation ,oxygenation and volume expansion |
|
|
|
Obstructive shock
|
Shocked that develops from cardiac tamponade tension pneumothorax or a massive pulmonary embolism because the common pathophysiology in these conditions is obstruction to blood flow from the heart .
cardiac tamponade and tension pneumothorax appear with clear lung sounds however lung sounds are unequal in a tension pneumothorax. Interventions oxygen, cardiac monitor, ivy ,boluses ,needle decompression if needed |
|
|
|
cardiogenic shock
|
Respiratory failure associated with decompensated shock leads to inadequate oxygenation, ventilation, and perfusion resulting cardiopulmonary failure.
Cardiopulmonary failure is a clinical condition identified by deficits in oxygenation ventilation and perfusion it will deteriorate to cardiopulmonary arrest. Cardiogenic shock occurs because of impaired cardiac muscle function that leads to decrese cardiac output may occur as a primary event in patients who have congenital heart disease or a complication of shock of any cause. Treatment is generally based on increasing contractility altering preload and afterload and controlling dysrhythmias if they are present and contributing to shock |
|
|
|
dysthymias
|
In pediatric patiens dysrhythmias are divided into four broad categories based on heart rate.
Normal for age slower than normal for age (bradycardia) faster than normal for age (tachycardia ) absent or pulseless (cardiac arrest) In children dysrhythmias are treated only if they compromise cardiac output or have the potential for deteriorating into a lethal rhythm Most often are because of hypoxia secondary to respiratory arrest and asphyxia. |
|
|
|
bradydysrhytmias
|
Can be classified as either primary or secondary primary is usually caused by structural heart disease because of atrioventricular block or sinus node disfunction physical examination may reveal a midline sternal scar and they may have an implanted pacemaker
Secondary is so slow heart rate from a non cardiac cause include increased vagal tone( vomiting ICP vagal maneuvers suctioning endotracheal intubation procedure) hypothermia hyperkalemia and injestions off medications such as calcium channel blockers (verapamil , diltiazem )beta blockers (ptopsnolol) Is an infant your child is symptomatic cause of bradycardia initial treatment is directed at assessment of the airway , breathing rather than given epinephrine, atropine or other drugs, problems with adequate oxygenation and ventilation are more common in children than are cardiac causes of bradycardia |
|
|
|
Seizure
|

It's a temporary change in behavior or consciousness caused by abnormal electrical activity of one or more groups of neurons in the brain.
febrile seizure is a generalize seizure that occurs with fever in childhood between the ages of 3 months in 5 years most occur between ages 6 and18 months a simpke febrile seizure is associated with core body temperature that increases rapidly to 38.8 °c (101.8°f) or greater. this seizure is usually tonic clonic and lasts a few seconds to 15 minutes is followed by a brief postictal period Of drowsiness. a complicated (also known as atypical febrile seizure lasts longer than 15 minutes the child may have repeated seizures within the same day. |
|
|
|
hypoglycemia and hyperglycemia
|
hypoglycemia, is comin in metabolically stressed children because a child is unable to store large quantities of glucose and mobilize what they can store in children alcohol intoxication increases susceptibility to hypoglycemia and alter mental status because alcohol suppress the ability of the liver to make glucose.
Intervention if the glucose level is less than 60 and gto stab list ivy axis administer text rose re check blood glucose level within 10 minutes and frequently there after until levels stabilizes. hyperglycemia, these to dehydration an kitoacidosis Common presenting symptoms of new onset or worsening diabetes include polydipsia,polyuria,polyphagia. slight increase may be seen in early diabetic kitoacidosis Kussmaul breathing develop later. tachycardia is common bp may decrease as a result of dehydration. do not give dextrose containing solutions. electrolyte imbalance particularly potassium may lead to ekg abnormalities and dysrhythmias |

|
|
|
meningitis
|

is an inflammation of the meninges which are the membrane that covering the brain and spinal cord. viral called ( aseptic meningitis) is most common.The inflammatory response causes the brain to become swollen and covered with a layer of pus.
newborns acquired by contact and aspiration of maternal intestinal and genital tract secretions shortly before or during delivery in older infants and children is usually secondary to another bacterial infection such as uri, ear infection, pneumonia,sinusitis. bacterial may occur from direct invasion of the cns by bacteria ex skull fracture (cfs leak) . enteroviruses most common cause of viral meningitis meningococcal meningitis most often occur in children<5 years |
|
|
|
Traumatic brain injury
|
a linear skull fracture is the most common type of skull fracture in a child.
In adults an epidural hematoma is usually from an arterial tear, typically the middle meningeal artery. a pediatric epidural hematoma occasionally may be the result of venous bleeding. this predisposes the child to more subtle s/s that occur over days. in children subdural hematomas most commonly occur in patients younger than 2 years, 93% of cases involving younger than 1 year. Chronic subdural hematomas are more often seen impatiens who have been subjected to shaken baby syndrome. An acute subdural hematoma is the most common cause of death in sports related head injuries because it also is associated with cerebral contusion and edema. A newborn or infant often presents with focal seizures, decreased level of consciousness, bulging fontanelle ,weak cry, pallor and vomiting.retinal hemorrhage which may occur as a result of primary injury are common. |
|
|
|
chess trauma
|
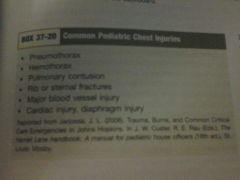
Child's chest wall is more flexible than that or adults.
rib fractures are most often caused by blunt trauma. Multiple rib fractures may result in inadequate breathing and pnuemonia. Flail chest is a life threatening injury when it is seen without a significant mechanism of injury suspected child abuse. A pulmonary contusion is one of the most frequently observed chest injuries in children. Many children with cardiac tamponade have no physical signs of tamponade other than hypotension. Is profound hypovolemia is present jugular venus distention is absent if bradycardia occurs the child is about to arrest. |
|
|
|
abdominal and pelvic trauma
|
It is the most common cause of unrecognize fatal injury in children.
The spleen is the most frequently injured abdominal organ during blunt trauma the rib cage does not extend down far enough to provide adequate protection The liver is the second most commonly injured solid organ in the pediatric patient with blunt abdominal trauma but the most common cause of lethal hemorrhage. |
|
|
|
Drowning
|
The major physiologic consequences of submersion are hypoxia acidosis and pulmonary edema hypoxia is the most important.
All victims should be transported for evaluation signs of pulmonary infection may appear many hours after the event. If incident not witness assume cervical spine injury and provide in line stabilization. Routine use of abdominal thrust or the Heimlich maneuver is not recommended these procedures can cause injury vomiting and aspiration and delay CPR. |
|
|
|
Sudden infant death syndrome SIDS
|
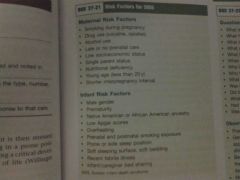
It has been suggested thats is is the final common pathway of three coinciding factors
1.an infant must first have an underlying vulnerability. 2. the infant is then stress by an outside source such as sleeping in the prone position and 3. the stress must occur during a critical developmental period as in the first year of life. The majority of SIDS deaths occurred during the first 6 months of life most between the ages of two and four months most of these infants died at home usually during the night after a period of sleep. |
|
|
|
Cerebrospinal fluid Shunts
|
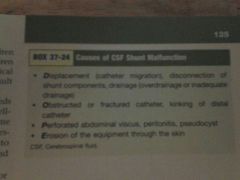
csf is pro duced in the choroid plecus located in the ventricles of the brain.
To drain excess CSF and reduce intracranial pressure on shunting system is surgically implanted into the brain to drain CSF from the ventricular system into another part of the body. The proximal catheter is usually inserted into one of the ventricles of the brain and exits the school through a surgically created hole (burr hole. The distal catheter is placed into a body cavity to allow drainage and absorption of CSF. Shaun malfunctions symptoms: Irritability, headache, neck pain ,vomiting ,a bulging or full fontanel in infants new seizures or a change in the child's seizure pattern behavioral changes . |
|

