![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
172 Cards in this Set
- Front
- Back
|
Things that cause arterial pressure waveform dampening
|
Arterial obstruction. Catheter occlusion or clot. Kinking of pressure tubing. Air in tubing. Loss of flush pressure in tubing. Transducer failure.
|
|
|
If a-line transducer below level of heart what does it do to BP
|
Overestimates. Remember - BP moves along WITH THE BED!!
|
|
|
A-line transducer above level of the heart
|
Underestimates BP. Remember - BP moves with bed!
|
|
|
Does moving the arm up or down (lateral position) change arterial BP measurement?
|
No
|
|
|
Does lateral positioning change noninvasive BP measurement?
|
Yes. Dependent arm has higher BP.
|
|
|
Transducer height and BP change: conversion factor. 1 mmHg =
|
1.36cm
|
|
|
Narrow cuff
|
Overestimates BP
|
|
|
Large Cuff
|
Underestimates BP
|
|
|
Things that cause Acquired QT prolongation
|
Antiarrhythmics class I:
-Quinidine -Procainamide. -Disopyramide. Anti arrhythmic class III: -Amiodarone. -Sotalol. -Ibutilide. -Dofetilide. -Dronedarone. Hypomagnesemia. Hypokalemia. Tricyclic antidepressants: -Amitryptiline. -Doxepin. -Imipramine. -Clomipramine. Non sedating antihistamines. Erythromycin. Pentamidine. Azole antifungal agents. Hypothyroidism. CVA. Liquid protein diets |
|
|
Which form of local anesthetic allows penetration of nerve membrane
|
Uncharged form (unionized)
|
|
|
Which form of local anesthetic blocks the sodium channel
|
The charged form
|
|
|
What does a low pKa mean about a local anesthetic
|
It has a great(er) percentage of unionized drug (uncharged molecules) at a given pH
|
|
|
What is the primary determinant of local anesthetic POTENCY
|
Lipid solubility
|
|
|
What determines speed of onset of action for local anesthetics
|
PKa. LOWER pKa will have FASTER onset of action.
|
|
|
What has faster onset of action: local with high pKa or low pKa?
|
Low
|
|
|
List the Ester Local anesthetics
|
Procaine. Chlorprocaine. Tetracaine.
|
|
|
How are ester local anesthetics eliminated
|
Bio transformed by hydrolysis
|
|
|
Order of blood levels based on site of administration
|
IV. Tracheal. Intercostal. Caudal. Epidural. Brachial Plexus. Sciatic Femoral.
|
|
|
How are ester local anesthetics eliminated
|
Bio transformed by hydrolysis
|
|
|
How are amide local anesthetics eliminated?
|
Metabolized by hepatic microsomal enzymes.
|
|
|
What genetic predisposition can delay metabolism/increase toxicity of ester local anesthetics?
|
Pts with atypical or low plasma cholinesterase may have delayed metabolism, potentially increasing risk of toxicity
|
|
|
What can increase risk of toxicity of amide local anesthetics?
|
Decreased hepatic blood flow, ie hepatic disease or heart failure
|
|
|
Cauda Equina Syndrome
|
Severe back pain, saddle anesthesia, bowel/bladder dysfxn, sciatica, leg weakness
Associated w intrathecal lidocaine. Associated w neurotoxic concentrations of drug. |
|
|
Contributing Factors of TNS (ONLY contributing factors)
|
Lithotomy. Knee scope. Outpatient status.
|
|
|
Resolution of TNS
|
Within 3 days, rarely 7. Symptoms show up within 12-24 hrs. Treat w NSAIDS.
|
|
|
Which has the least vasodilation, mepivicaine or lidocaine?
|
Mepivicaine
|
|
|
Prilocaine unique factor
|
High doses can result in accumulation of metabolite ortho-toluidine which can produce methemoglobinemia.
|
|
|
Bupivicaine consists of
|
Racemic mixture of isomers
|
|
|
Bupivicaine toxicity
|
Cardio toxicity!!!! Bupivicaine tends to remain in Na channel ("fast in/slow out") Favors unidirectional block which can result in re-entry. Disrupts conduction thru AV node. Decreased myocardial contractility.
|
|
|
Ropivicaine conformation
|
S - enantiomer of Bupivicaine.
|
|
|
Why is ropivicaine thought to be less toxic than Bupivicaine
|
More vasoconstriction thus slower uptake. Less fast in/slow out. PS (drug is less potent). Not really relevant here though.
|
|
|
Methemoglobinemia occurs in association with
|
Benzocaine or EMLA cream
|
|
|
What percentage of allergic reactions are associated with NMBs?
|
33+%
|
|
|
What causes proliferation of extrajunctional receptors
|
Prolonged inactivity. Denervation. Trauma/Burns. Sepsis.
|
|
|
Extrajunctional receptors bad effects (2):
|
(1). Remain open longer --> more ion flow. Contributes to HYPERKALEMIA WITH SUCCINYLCHOLINE. (2). Proliferation accounts for resistance to non depolarizing muscle relaxants.
|
|
|
Phase II Block
|
Achieved by repeated dosing of sux. Resembles block achieved by non depolarizing drugs. Not reliably reversed by reversal agents.
|
|
|
Side Effects of Succinylcholine
|
Cardiac Dysrhythmias:
-Sinus bradycardia. -Junctional rhythm. -Sinus arrest. Fasciculations. Hyperkalemia. Myalgia. Myoglobinuria. Increased intraocular pressure. Increased intra gastric pressure. Trismus. |
|
|
Sux is metabolized by
|
Plasma cholinesterase
|
|
|
How much sux reaches NMJ after injection
|
Small fraction
|
|
|
Is plasma cholinesterase present at the NMJ
|
NO.
|
|
|
What terminates the action of sux?
|
Diffusion away from NMJ
|
|
|
Things that cause decreased levels of pseudo cholinesterase
|
Drugs:
-Nitrogen mustard. -Cyclophosphamide. -Anticholinesterase. Liver disease. Renal failure. Cancer. |
|
|
Plasma cholinesterase wild type dibucaine #, duration of action, incidence
|
80, 5-10 min, normal
|
|
|
Plasma cholinesterase heterozygous atypical dibucaine #, duration of action, incidence
|
50-60, 20 min. 1/480.
|
|
|
Plasma cholinesterase homozygous atypical dibucaine #, duration of action, incidence
|
20-30, 1-3 HOURS, 1/3200
|
|
|
Molecular characteristics if NDMB
|
Highly ionized, water soluble, poor lipid solubility (can't cross bbb or placenta)
|
|
|
Things that prolong duration of action of NDMB
|
*Aminoglycoside antibiotics. *Dantrolene. *Magnesium Local anesthetics. Antiarrythmics. Lithium. Tamoxifen.
|
|
|
Clearance of Rocuronium
|
Unchanged in bile. Up to 30% by the kidneys.
|
|
|
Vecuronium metabolism/excretion
|
Hepatic metabolism. **one metabolite, 3-something, is 50-70% as effective as Vec. Excreted in bile. Renal failure --> slight prolongation of duration of action.
|
|
|
Which sodium channel conformational states do local anesthetics bind to the best, and what effect is this responsible for
|
Bind to activated and inactivated states much better than resting state. Thus repeated depolarization produces more effective anesthetic binding. This is called USE DEPENDENT OR FREQUENCY DEPENDENT BLOCK. May relate to which nerves are blocked more quickly.
|
|
|
Relationship between lipid solubility and time to onset (latency) of local anesthetic block
|
The higher the lipid solubility the faster the time to onset of block.
|
|
|
Things that correlate with duration of action of local anesthetic
|
Protein binding. Lipid solubility (inverse correlation)
|
|
|
A alpha nerve fiber: Myelinated? Relative conduction velocity? Function?
|
Myelinated. Fastest. Proprioception, large motor.
|
|
|
A beta nerve fiber: Myelinated? Relative conduction velocity? Function?
|
myelinated. second fastest. small motor, touch, pressure
|
|
|
A gamma nerve fiber: Myelinated? Relative conduction velocity? Function?
|
myelinated. 3rd fastest. muscle tone.
|
|
|
A delta nerve fiber: Myelinated? Relative conduction velocity? Function?
|
myelinated, but slower conduction. 4th fastest. pain, temperature, touch.
|
|
|
B nerve fiber: Myelinated? Relative conduction velocity? Function?
|
myelinated. 2nd to slowest. preganglionic autonomic
|
|
|
C nerve fiber: Myelinated? Relative conduction velocity? Function?
|
UNmyelinated. slowest. dull pain, temperature, touch.
|
|
|
chemical factors that delay local anesthetic uptake
|
high lipophilicity, high protein binding.
|
|
|
Mechanism of local anesthetic CNS toxicity
|
Selective depression of cortical inhibitory neurons leaving excitatory pathways unopposed ( local anesthetics are neuronal depressants)
|
|
|
EKG changes in local anesthetic toxicity
|
Prolongation of PR interval
Widening of QRS complex |
|
|
Type of local anesthetic most likely to produce allergic reaction and why
|
Esters- Produce metabolites related to PABA . Allergic reactions also can Be caused by Preservatives like methyl paraben
|
|
|
Unique side effects of procaine
|
Nausea
Hypersensitivity Also can cause TNS |
|
|
Unique Characteristics of tetraCaine
|
fairly long duration of action
high risk of TNS when used w/ Vasoconstrictor slow onset profound motor blockade potential toxicity slow metabolism |
|
|
Unique characteristics of Mepivicaine
|
Similar to lidocaine but:
- Less vasodilation -Slightly longer duration of action -Ineffective as topical anesthetic |
|
|
How does Prilocaine induced methemoglobinemia resolve
|
-Spontaneously subsides
- Can be reversed by methylene blue l-2mg per kg over 5 min |
|
|
Which enantiomer of bvpivicaine has less cardio toxicity
|
S-
|
|
|
Benefits of ropivicaine
|
Be+ter than bupivicaine with Cardiac Sodium channels
Produces more Vasoconstriction Motor blockade less pronounced C fibers preferentially blocked ? |
|
|
Drawbacks of ropivicaine
|
Less potent meaning more must be given to get same effect (potentially negating belter risk profile w/ cardiac toxicity)
More expensive |
|
|
what is the first ion change when action potential arrives at the NMJ ?
|
Influx of calcium ions causes release of Ach
|
|
|
What subunits do the NMBS bind to on the postjunctional receptor ?
|
The two alpha subunits
|
|
|
Chemical structure of NMDB that allows it to bind to alpha subunit
|
Quaternary ammonium , positively charged nitrogen atom binds to alpha Subunit
|
|
|
List the amino steroid NMDBS
|
PANCVRONIUM
VECURONIUM ROCURONIUM |
|
|
list the BENZYLISOQUINOLlNlUM NMDBS
|
AtraCurium
cisatraCurium Mivacurium |
|
|
Which NMBDs most likely to evoke the release of histamine & why
|
atrawrivm
cisatracurium - doesnt really do it MiVacurium related to fast infusion of high doses |
|
|
Elimination of roCuronivm
|
Liver
|
|
|
Elimination of mivacurium
|
metabolism by plasma cholinesterase
|
|
|
Elimination of atracurium or cisatracurium
|
Hoffman elimination
|
|
|
What diminishes the effect of NMBDs
|
calcium
corticosteroids phenytoin & anticonvulsants |
|
|
What can cause resistance to NMBD
|
Burn injury
CVA'S |
|
|
Cardiac effect of Pancuronium
|
modest blockade of cardiac postganglionic mUscarinic receptors
|
|
|
Pancuronium % renal excretion
|
80 %
|
|
|
% Renal excretion of Vecuronium
|
15-25%
|
|
|
Rocuronivm % renal excretion
|
10-25%
|
|
|
PanCuronium % hepatic degradation
|
10%
|
|
|
VecuroniUm % hepatic degradation
|
20-30%
|
|
|
RocuroniUm % hepatic degradation
|
10-20%
|
|
|
Pancuronium % Biliary excretion
|
5-10%
|
|
|
Vecuronium % Biliary Excretion
|
40-75%
|
|
|
Rocuronium % Biliary Excretion
|
50-70%
|
|
|
Pancuronium lntubating Dose
|
0.1 mg/Kg
|
|
|
Vecuronium lntubating Dose
|
0.08 - 0.1%
|
|
|
Rocuronium Intubating Dose
|
0.3 mg/kg
|
|
|
Atracurium intubating dose
|
0.5mg/kg
|
|
|
Cisatracurium Intubating Dose
|
0.1 mg/kg
|
|
|
Mivacurium lntubating Dose
|
0.25 mg/kg
|
|
|
Pancuronium- Duration to return to greater than or equal to 25%
|
60-90 min
|
|
|
Mivacurium - Duration to return to greater than or equal to 25%
|
12-20 min
|
|
|
Vecuronivm, Rocuronium, Atracurium, Cisatracurium - Duration to return to greater than or equal to 25%
|
20-35 min
|
|
|
What increases duration of action of pancuronium
|
Renal failure
|
|
|
What NMBD has a potent metabolite
|
Pancuronium - 50 percent as potent
|
|
|
Cardiac effects of pancuronium
|
modest 10-15% increase in HR, MAP t CO
|
|
|
How does pancuronium produce cardiac effects
|
Selective blockade of cardiac muscarinic receptors principally in SA node - more likely to occur in pts with AV conduction issues already
|
|
|
Clearance of Atracurium
|
Hoffman elimination
Ester hydrolysis by nonspecific esterases |
|
|
Metabolite of NMB that can cause CNS stimulation and what NMB
|
Laudanosine is metabolite
Atracurium Much less produced by cisatracurium |
|
|
Clearance of ciSatracurium
|
Hoffman elimination to Laudanosine- don't really see Laudanosine toxicity because cis is so potent
|
|
|
What could theoretically slow the hydrolysis of mivacurium and why
|
Neostigmine because it decreases plasma cholinesterase (pseudo cholinesterase activity)
|
|
|
List Major Criteria for perioperative Beta Blockade
|
Ischemic Heart Disease :
History of MI Use of Nitrates Q waves on ECG Current history of angina + Stress test Abdominal, thoracic, vascular surgery planned Any history of congestive heart failure Insulin dependent diabetes Any history of CVA Sewm Cr> 2.0 Arterial vascular disease |
|
|
Minor Criteria for perioperative Beta Blockade
|
Age > 70
Hypertension Total cholesterol > 240 Non Insulin Dependent Diabetes Current Smoker |
|
|
perioperative beta blockade -
3+ major criteria and any minor criteria -elective surgery |
1. Beta blocker indicated but patient needs further Cardiac workup
2. Refer to preop clinic 5-7 days before surgery |
|
|
Perioperative beta blockade
3+ major criteria and any minor criteria - emergent surgery |
1. Beta blocker therapy probably indicated
2. Consult cardiology or medicine |
|
|
Peri operative Beta Blockade
l-2 major criteria plus 2 or More minor criteria -elective surgery |
1. Beta blocker therapy indicated
2. Refer to preop clinic 2-5 days before surgery |
|
|
Peri operative Beta Blockade
no major criteria plus 0-1 minor criteria -elective surgery |
1. Beta blocker not indicated
2. Refer to preop clinic for routine eval 2-3 days before surgery |
|
|
Peri operative Beta Blockade
l-2 major criteria plus 2 or More minor criteria -emergent surgery |
l. Beta blocker indicated
Consult cards or medicine |
|
|
Contraindications to periop beta blocker
|
1. current symptoms of CHF or EF<30
2. sick sinus syndrome or 2nd or 3rd degree AV block without pacemaker 3. heart rate <55 without pacemaker 4. S3, rales, wheezing on exam 5. known intolerance 6. poorly controlled asthma or copd 7. sbp less than 100 8. same day or outpatient surgery |
|
|
Cardiac complication rate by risk factor - O, l, 2, 3 plus
|
0.4%, 0.9%, 7%, 11%
|
|
|
Independent Risk Factors for Cardiac Events (6)
|
l. High Risk Surgery
2. History of ischemic heart disease 3. Congestive heart failure 4. Cercbwvaswlar disease S. Insulin dependent diabetes 6. Cr>2.0 |
|
|
Prophylaxis for anesthesia for people with chronic atopy or having Procedures associated with allergic reactions like dye studies
|
Benadryl 25-50 mg
Cimetidine 300mg occupy peripheral sites responsive to histamine |
|
|
Central Anti cholinergic Syndrome and treatment
|
Delirium or Somnolence with Scopolamine or atropine
treatment - physostigmine up to 2mg IV |
|
|
H 2 blocker method of action
|
competitive inhibitor of histamine at parietal cells which help increase ph of fluid
names - ranitidine, cimetidine, etc |
|
|
What is the partial pressure of 60 % Nitrous at Sea level?
|
760 x 0.6 = 456 mmHg
760 = barometric pressure |
|
|
What amount of total airway resistance occurs in nasal passages
|
2/3
|
|
|
What innervates the nasal mucosa
|
Trigeminal nerve - V1 and V2 opthalmic and maxillary .
Called anterior ethmoidal, nas0palatine, & spheNopalatine |
|
|
What provides sensation to anterior 2/3 of tongue
|
Mandibular division of trigeminal -V3
Called Lingual Nerve |
|
|
What provides innervation to posterior third of tongue, soft palate and oropharynx
|
glossopharyngeal nerve - cranial nerve IX
|
|
|
What provides sensation to the hypopharynx
|
Internal branches of SUPERIOR laryngeal nerve - branch of Vagus
|
|
|
Independent predictors of difficult mask
|
1. Age over 55 years
2. BMI over 26 3. Beard 4. Lack of teeth s. History of snoring |
|
|
Superior Laryngeal Nerve Block - internal branch anatomy
|
Between greater cornu of hyoid bone and superior cornU of thyroid cartilage as they traverse the thywhyoid membrane to the Sub mucosa of the piriform sinus
|
|
|
Superior Laryngeal Nerve Block - internal branch approach
|
Needle walked off cephalad edge of thyroid cartilage or caudal edge of hyoid bone
|
|
|
Differences between infant and adult airway (7)
|
1. larynx at c3-4 in infants vs c4-5 in adults
2. tongue larger relative to mouth size in infants 3. epiglottis in infants larger, stiffer, and angled more posteriorly 4. head and occiput larger relative to body size 5. short neck 6. narrow nares 7. cricoid ring is the narrowest region |
|
|
how many cervical vertebrae are there
|
7
|
|
|
how many thoracic vertebrae are there
|
12
|
|
|
how many lumbar vertebrae are there
|
5
|
|
|
Level of iliac crests
|
L4
|
|
|
Most outlying point of lower neck
|
C7
|
|
|
Level of the lower border of the scapulae
|
T7-8 interspace
|
|
|
What vertebral body does the 12th rib intersect
|
L2
|
|
|
Level of posterior iliac spine - what is special about this level
|
S2 - caudal limit of dural sac in most adults
|
|
|
What level does the spinal cord end in infants
|
L3
|
|
|
What level does the spinal cord end in adults
|
L1
|
|
|
At what level does the dura terminate
|
Between S1 and S4
|
|
|
What prevents migration of drug from epidural to subarachnoid space
|
the arachnoid mater
|
|
|
How does an epidural block spread
|
Rostrally and caudally (up and down)
|
|
|
What and where is maximal depth of epidural space
|
6mm at midline L2
|
|
|
Anterior spinal artery syndrome
|
bilateral lower extremity motor loss. can be associated with surgery near aorta (AAA resection) or by stray epidural needle
|
|
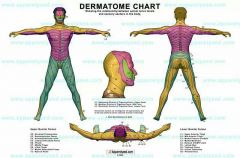
Name the dermatomes
|
|
|
|
Where does the artery of Adamkiewicz enter
|
through L1 intervertebral foramen
|
|
|
Posterior spinal artery - how many, where does it originate, what does it supply
|
Two.
emerge from cranial vault. supply dorsal (sensory) part of spinal cord have rich collaterals. |
|
|
Anterior spinal artery - how many, where does it originate, what does it supply
|
One.
originates from vertebral artery. Supplies ventral (motor) part of spinal cord |
|
|
Effect of increased intra-abdominal pressure or tumors/masses compressing the vena cava on epidural anesthesia
|
Blood is diverted from IVC and engorges veins in epidural space:
Increases likelihood of accidental vascular cannulation Greater longitudinal spread of local due to effective reduction of epidural space |
|
|
Contraindications to neuraxial block: Absolute & Relative
|
Absolute:
Patient refusal Infection at planned needle site Elevated lCP Coaguiopathy Relative: Multiple sclerosis or other neurologic disease Mitral stenosis Idiopathic hypertrophic subaortic stenosis Aortic stenosis |
|
|
Level and Significance of Sensory Block
Cutaneous level : Fifth digit Segmental level , Significance : |
Segmental level: c8
Significance: All cardioaccelerator fibers blocked |
|
|
Level and Significance of Sensory Block
Cutaneous level : Inner aspect of arm and forearm Segmental level , Significance : |
Segmental level: T1- 2
Significance: Some degree of cardioaccelerator block |
|
|
Level and Significance of Sensory Block
Cutaneous level : Apex of the axilla Segmental level , Significance : |
Segmental level: T3
Significance: Easily determined landmark |
|
|
Level and Significance of Sensory Block
Cutaneous level : Nipple Segmental level , Significance : |
Segmental level: T4-5
Significance: Possibility of cardio accelerator block |
|
|
Level and Significance of Sensory Block
Cutaneous level : Tip of the xiphoid Segmental level , Significance : |
Segmental level: T7
Significance: Splanchnics (T5-L1) may be blocked |
|
|
Level and Significance of Sensory Block
Cutaneous level : Umbilicus Segmental level , Significance : |
Segmental level: T10
Significance: Sympathetic nervous System block limited to the legs |
|
|
Level and Significance of Sensory Block
Cutaneous level : Inguinal Ligament Segmental level , Significance : |
Segmental level: T12
Significance: No sympathetic nervous system block |
|
|
Level and Significance of Sensory Block
Cutaneous level : Outer side of foot Segmental level , Significance : |
Segmental level: S 1
significance: Confirms block of root most difficult to anesthetize |
|
|
Site of action for intrathecal opioids
|
Dorsal horn of spinal cord where Opioids mimic enkephalins
|
|
|
neuroleptic malignant syndrome - etiology
|
Related to dopamine blockade in the basal ganglia and hypothalamus due to long term administration of psychoactive drugs
|
|
|
Respiratory changes of Old age
|
Increased residual volume
Increased closing capacity Increased chest wall stiffness Decreased alveolar surface area , decreased Pao2 Blunted response to hypercapnia and hypoxia |
|
|
Epidural & spinal changes with old age
|
Higher cephalad spread but shorter duration of analgesia and motor block- etiology unknown
spinals have longer duration of action |
|
|
Pharmacokinetic changes of old age
|
Decreased VD for water soluble drugs
Increased VD for lipid soluble drugs Decreased albumin binding of acidic drugs (opioids, BZD, barbiturates) Increased alpha protein binding of basic drugs (LA) Decreased Clearance of drugs |
|
|
What is produced by burning PVC ETT
|
HCl -a pulmonary toxin
|
|
|
What nerve roots supply LES tone
|
T6 -T1O
Vagus & sympathetics |
|
|
Drugs that increase LES tone
Drugs that decrease LES tone |
Increase: Antacids (bicitra), reglan, sux, beta blockers - metoprolol. , anticholinesterases
Decrease: Benzodiazepines, narcotics (most sedatives but not propofol or etomidate at low doses), volatiles, anticholinergics |
|
|
NIOSH limit for N2O amount in OR (1977)
NIOSH limit for N2O + volatile amount in OR NIOSH limit for volatile alone amount in OR |
1. 25 ppm
2. 0.5 ppm 3. 2 ppm |
|
|
Periop wrist drop - nerve injured
|
radial
|
|
|
Manifestations of citrate toxicity
|
Narrow pulse pressure
Hypocalcemia --> prolonged QT |
|
|
What is mixed venous O2 in cyanide toxicity?
|
High. cyanide toxicity blocks cytochrome oxidase in tissues and wont allow tissue use of O2 in blood.
|
|
|
What determines the duration of conduction block of local anesthetic
|
Protein binding
|

