![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
When are male and female reproductive organs developed?
|
embryologically
|
|
|
|
organs that make sex cells?
|
gonads
|
|
|
|
primary female gonads?
|
ovaries: make ova (eggs), gametes, sex cells, germ cels
|
|
|
|
primary male gonads?
|
testes (gametes = spermatozoa)
|
|
|
|
secondary sex organs?
|
internal and external organs, accessory sex organs
|
|
|
|
development of male gonads, details?
|
development of testes begins in abdomeno-pelvic cavity, then descend into the scrotum.
|
|
|
|
why do testes drop into scrotum?
|
need lower temperature outside for fertility and motility
|
|
|
|
what if testes do not drop? name of condition? possible risks associated?
|
crypt-ORCHID-ism.
increased risk for testicular cancer. most common reproductive cancer in young men (15-35 years). highly curable. removal of the tesis--orchi-ectomy, radiation and chemo |
|
|
|
function of testes? some anatomy associated
|
spermatogenesis: produce sperm in seminiferous tubules
surrounded by tunica albuginea: between seminiferous tubules and fibrous. |
|
|
|
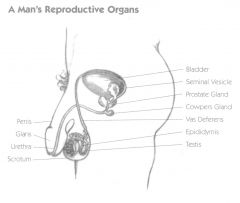
structure of the testes and function of parts? 5 parts.
|
1. myoid cells: surround seminif tubules. contract to help squeeze sperm and testicular fluids out of testes.
2. seminif tubules: "sperm factories." then converge. seminif tubules-->straight tubule-->rete testis-->epididymis. 3. interstitial cells: in between semi tubules. make androgens (most importantly testosterone). 4. epididymis: connects on one end of testis and other end to the vas defrens. (a) store sperm (b) make sperm fertile and motile (c) ejaculation: release of semen at organsm form epididymis. smooth muscle contracts. 5. vas defrens: tube from epididymis to urethra: passes the spermatic cord into the pelvic cavity--inguinal canal. |
MSI-EV
|
|
|
elaborate on vas defrens, different parts of it? 2 characteristics
how can this be used in birth control? |
1. ampulla: widened end. joins with a duct from the seminal vessicle (gland)--forms ejaculatory duct (short) joins urethra.
2. has smooth muscle. when a man ejaculates the muscle undergoes peristalsis 3. vasectomy: voluntary sterilization as birth control. block path of sperm. vas defrens is either clipped, piece cut out, cauterized on both left and right side. semen is produced but without sperm in it. normal erection, ejaculation and hormones. |
|
|
|
locate seminal vessicle, ejaculatory duct and vas defrens.
|
|
|
|
|
glands contributing to semen production?
|
1. seminal vessicles
2. prostate gland 3. bulbourethral glands |
|
|
|
function of seminal vessicle in sperm production
|
1. secretes alkaline fluid that counteracts acid in urethra and vagina
2. secretes fructose: key energy source for sperm. other nutrients: vit C. help motility and fertility. 3. prostaglandins: regulators of body functions, both reproductive and non. not actually a horomone because found in semen, not blood. also, affect woman, not man. a. in reproduction: stimulate smooth muscle, enhance changes of fertilization. b. in cervix of woman: make secretions less viscous, allows sperm to swim more easily. stimultes contraction of uterine muscle--reverse peristalsis in woman to help sperm make it up fallopian tube. |
|
|
|
function of prostate gland in sperm production. 5 points to cover
|
1. Overall, semen is basic but stuff from prostate is slightly acidic.
2. Contributes to 1/3 of volume in semen. 3. Contains citrate, feeds into kreb’s cycle. Also contains nutrients, H enzymes. 4. Enzymes that enhance fertility of the sperm 5. secretes prostate specific antigen (PSA) |
|
|
|
possible problems with prostate, function of PSA
|
1. Prostate specific antigen (PSA): a marker for risk of prostate cancer >4 mg/ml = increased risk
- Problem with PSA stuff is that it’s not completely certain. Can have false positives of false negatives. Regardless, a generally good marker. Can do additional tests for prostate cancer. how to feel prostate? Digital/rectal exam—make’s possible to feel prostate. 2. prostate cancer 3. benign prostatic hyperplasia |
|
|
|
Prostate cancer, characteristics, risks and treatment.
|
most common reproductive cancer in men.
increased risk if: high fat, old age, high calorie diet, genetics treatment: surgery. but if cut nerves accidentally, leads to impotence. radiation also helps--put seed with radioactive element. |
|
|
|
Benign prostatic hyperplasia charcteristics
|
enlarged prostate- not cancer. because more cells present.
1. Frequent urination- bc of pressure on urethra 2. Fairly common in older men |
|
|
|
bulbourethral glands and contribution to sperm. another name for this gland
|
also called cowper’s glands:
secrete thick muscus (as a lubricant). generally alkaline. contributes to smallest amount of semen compared to the other three glands. |
|
|
|
overall semen charcteristics. 4 points.
|
1. semen about 5 ml in 1 ejaculate.
2. ~250-400 million sperm in ejaculate. (~100 make it to fallopian tube) 3. pH is 7.2-7.6 4. other substances- enhance motility. a. suppress immune system of female so her antibodies don’t destroy sperm b. antibacterial proteins c. relaxin: in birth, helps relax vagina to help fetus move through birth canal. In men, helps stimulate prostate development. In semen, appears to have role of enhancing fertility of semen. |
|

