![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
3 forms of arteriosclerosis
|
1. atherosclerosis
2. Monckeberg medial calcific sclerosis 3. arteriololsclerosis |
|
|
The principal points of physiologic resistance to blood flow.
|
arterioles
|
|
|
2 principal mechanisms of vasucular disease
|
1- narrowing or obstructing vessel
2- weakening of vessel walls |
|
|
what are the 3 layer of blood vessels?
|
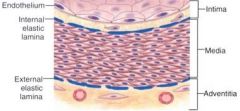
intima, media, adventitia
|
|
|
pathology affecting elastic and muscular arteries
|
Atherosclerosis
(b/c of size range) |
|
|
pathology affecting small muscular arteries and arterioles
|
HTN
(b/c of size range) |
|
|
different types of vasculitis affect different _______
|
calibers of vessels
|
|
|
classification of coronary and renal arteries
|
muscular
(smooth muscle) |
|
|
vasoconstriction and dilation occur in the _______ arteries
|
small arteries
|
|
|
blood flow in the small arteries is steady and ________
|
non-pulsatile
|
|
|
small arteries are < ____mm in diameter
|
2
|
|
|
Capillaries, which are approximately the diameter of a red blood cell (7 to 8 µm), have an endothelial cell lining but no ________.
|
media
|
|
|
In many types of inflammation, vascular leakage and leukocytic exudation occur preferentially in ______________.
|
postcapillary venules
(site of WBC migration) |
|
|
____________ constitute an important pathway for disease dissemination through transport of bacteria and tumor cells to distant sites.
|
Lymphatics
|
|
|
Among the diverse congenital vascular anomalies, two have importance: ____________ and ______.
|
1- developmental or berry aneurysms and
2- arteriovenous fistulas. |
|
|
AV fistulas may cause ______-output heart failure.
|
high
|
|
|
a generic term for thickening and loss of elasticity of arterial walls:
a) atherosclerosis b) arteriosclerosis c) arteriolosclerosis d) Monkeyberg medial calcific slerosis |
arteriosclerosis
|
|
|
3 types of arteriosclerosis
|
1 atherosclerosis
2 Monckeberg medial calcific sclerosis 3 arteriolosclerosis |
|
|
The least clinically important arteriosclerosis type
|
Monckeberg medial calcific sclerosis
|
|
|
Arteriosclerosis found in muscular arteries of people over 50.
|
Moncheberg medial calcific sclerosis
|
|
|
2 types of arteriolosclerosis
|
hyaline and
hyperplastic arteriolosclerosis |
|
|
type of arteriosclerosis assoc. with DM and HTN
|
hyaline arteriolosclerosis
|
|
|
cause of 50% of all death in US, Europe and Japan:
a) arteriosclerosis b) atherosclerosis c) arteriolosclerosis d) Monkeyberg |
Arteriolsclerosis - Zamam ("US, Europe, Japan")
Atherosclerosis - Robbins ("Western World") |
|
|
Atherosclerosis is characterized by intimal lesions called _______
|
atheromas
|
|
|
Arteriosclerosis results from an excessive ________ and proliferative response to various forms of injury to the endothelium and
smooth muscle of the arterial wall. |
inflammatory
|
|
|
Factors thought important in Arteriosclerosis' pathogenesis include:
|
- changes in lipid metabolism,
• increased endothelial permeability to serum lipoprotein complexes, • susceptibility of the intima to mechanical injury from flow turbulence at major bifurcations, • presence of hypertension, elastic tissue fragmentation and thrombosis or disruption of vasa vasorum. |
|
|
Surgical therapy is now commonplace for occlusive disease of the ________(3) arteries
|
coronary, carotid, and
mesenteric |
|
|
Arteriosclerosis may present as an occlusive process
when the disease attacks the intima more rapidly than the media and adventitia, but may present as an __________ when the reverse is true. |
aneurysm
|
|
|
Arteriosclerosis may present as an ___________________
when the disease attacks the intima more rapidly than the media and adventitia |
occlusive process
|
|
|
Arteriosclerosis may present as an ______________
when the disease attacks the media and adventitia more rapidly than intima. the , |
aneurysm
|
|
|
early human lesions begin at sites of ___________ endothelium.
|
morphologically intact
Thus, nondenuding endothelial dysfunction causing increased endothelial permeability, enhanced leukocyte adhesion, and alterations in expression of EC gene products is critical to the human disease. |
|
|
Chronic or repetitive endothelial injury is the cornerstone of the "response to injury" hypothesis of arteriosclerosis.
|
Duh.
|
|
|
Intimal plaques are composed of lipid deposits and
proliferated spindle cells made up of ______ and ________. |
fibroblasts and smooth muscle cells
|
|
|
What is the stereotypic response to vascular injury?
|

1,2,3
|
|
|
Atherosclerosis:
The earliest changes, which are considered to be reversible, are ____________of the intima. |
fatty dots and fatty streaks
|
|
|
Atheromatous plaques, the typical lesions of atherosclerosis, consist of an irreversibly altered softened central area filled with _____________and__________ surrounded by collagenous fibrous tissue
|
cholesterol crystals and cell debris
|
|
|
Atheromatous plaques aka
|
atheroma
|
|
|
composed of lipid-filled foam cells, are not significantly raised and thus do not cause any disturbance in blood flow.
|
fatty streaks
|
|
|
Fatty streaks appear in the aortas of some children younger than 1 year of age and all children older than ______ years, regardless of geography, race, sex, or environment
|
10
|
|
|
large lipid-laden cells that derive predominantly from blood monocytes (tissue macrophages), but SMCs can also imbibe lipid to become them
|
Foam cells
|
|
|
The four major risk factors of atherosclerosis that can be modified
|
hyperlipidemia, hypertension, cigarette smoking, and diabetes.
|
|
|
Describe monocytes role in atheromas
|
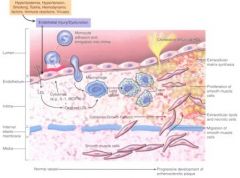
-
|
|
|
Macrophages produce interleukin 1 and tumor necrosis factor, which increase adhesion of ________
|
leukocytes
|
|
|
Macrophages produce toxic oxygen species that also cause oxidation of the _____ in the lesions
|
LDL
|
|
|
Macrophages eat the oxidized LDL to become _____
|
foam cells
|
|
|
an age-related degenerative
process in which the media of large and medium-sized muscular arteries undergoes calcification. |
Monckeberg medial
calcific sclerosis |
|
|
Hypertension is associated with two forms of small
blood vessel disease: |
1- Hyaline arteriolosclerosis
2- Hyperplastic arteriolosclerosis |
|
|
Left: hyaline arteriolosclerosis
Right: hyperplastic arteriolosclerosis |
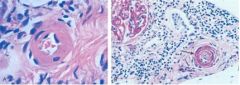
What's this? What's the difference?
|
|
|
Describe hyaline arteriolosclerosis
|
The arteriolar wall is hyalinized and the lumen is markedly narrowed.
|
|
|
Describe hyperplastic arteriolosclerosis
|
(onion-skinning) causing luminal obliteration (arrow), with secondary ischemic changes, manifest by wrinkling of the glomerular capillary vessels at the upper left
|
|
|
characterized by narrowing of
the lumen of arterioles due to the concentric proliferation of smooth muscle cells in the vessel wall. |
Hyperplastic arteriolosclerosis
|
|
|
Hyperplastic arteriolosclerosis is typically found in what conditions?
|
malignant hypertension,
progressive systemic sclerosis (scleroderma), chronic transplant rejection, and after radiotherapy. |
|
|
The process of occlusion probably begins in the iliac
arteries near what landmark? |
the aortic bifurcation
|
|
|
Thrombi and emboli can become secondarily infected by
what fungi? |
particularly Aspergillus and Mucor.
|
|
|
Leriche's syndrome
|
The syndrome of distal aortic thrombosis
|
|
|
How does Leriche's syndrome manifest itself?
|
an insidious onset and gradual progression of symptoms of pain and easy fatigability in the legs, hips, and back;
intermittent claudication; and sexual impotence, absence of pulses below umbilicus |
|
|
3 examples of arteries associated with some degree of fascial fixation.
|
1- ext. iliac artery behind inguinal ligament
2- superficial femoral artery (facial ring beneath adductor longus tendon) 3- anterior tibial artery (interosseous membrane) |
|

WTF?
|

Livedo reticularis
|
|
|
What are some complications of arterial occlusive disease?
|
Arterial embolism,
livedo reticularis, gangrene of lower extremities, ocular symptoms, cerebral infarct, GI Bleeding, renal HTN and failure |
|
|
What is livedo reticularis?
|
a vascular condition characterized by a purplish mottled discoloration of the skin, usually on the legs. This discoloration is described as lacy or net-like in appearance.
|
|

WTF?
|

Livedo reticularis
|
|
|
In arterial occlusive disease, simulataneous embolism to various organs may lead to a mistaken clinical diagnosis of _________ (PAN)
|
polyarteritis nodosa
|
|
|
What is Polyarteritis nodosa?
|
is a rare autoimmune disease featuring spontaneous inflammation of the arteries (arteritis).
|
|
|
How do you diagnose Polyarteritis nodosa? (3 of 10 things)
|
1. Weight loss greater than/equal to 4 kg.
2. Livedo reticularis (a mottled purplish skin discoloration over the extremities or torso). 3. Testicular pain or tenderness. (occasionally, a site biopsied for diagnosis). 4. Muscle pain, weakness, or leg tenderness. 5. Nerve disease (either single or multiple). 6. Diastolic blood pressure greater than 90mmHg (high blood pressure). 7. Elevated kidney blood tests (BUN greater than 40 mg/dl or creatinine greater than 1.5 mg/dl). 8. Hepatitis B virus tests positive (for surface antigen or antibody). 9. Arteriogram (angiogram) showing the arteries that are dilated (aneurysms) or constricted by the blood vessel inflammation. 10. Biopsy of tissue showing the arteritis (typically inflamed arteries). |
|
|
risk factors for atheroma
|
- Arterial hypertension
• Tobacco • Heredity (familial hypercholesterolemia) • Endocrine (DM, Postmenopausal, hypothyroidism • Reduced physical activity • Obesity • Male • Age |
|
|
modifiable risk factors for atheroma
|
Hypertension, hyperlipidemia, DM, smoking, activity.
|
|
|
major risk factors for atheroma
|
Htn, hyperlipidemia, DM, smoking
|
|
|
minor risk factors for atheroma
|
Obesity, rich diet, physical inactivity, type A, stress.
|
|
|
the most important risk factors under age 45 for atheroma
|
Hyperlipidemia and especially hypercholesterolemia
|
|
|
Homozygotes for FH can die by what age?
|
20
|
|
|
Heterozygotes develop AS by what age?
|
40
|
|
|
What are the steps of the injury hypothesis of atherosclerosis
|

-
|

