![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
Erythrocyte origin + life span? |
myeloid stem cell/precursor -> proerythroblast -> erythroblasts -> erythrocytes;life-span 120 days |
|
|
Erythropoietin synthesis occurs in? |
juxtatubular interstitial cells in kidneys in response to hypoxia |
|
|
Neutrophil origin? |
myeloblast -> promyelocyte-> myelocyte-> band form-> neutrophil |
|
|
Platelet: origin, function & lifespan? |
megakaryocytes; 10 days in circulation; role in 1˚ haemostasis;contribute to phospholipid -> promotes blood coagulation. |
|
|
MCH? |
MCH = Hb÷RBC
MCH = absolute Hb amount in individual red cell, tends to be parallel toMCV in macro/microcytic anaemia |
|
|
MCHC? |
MCHC = Hb÷Hct MCHC = concentration of Hb incell, related to shape, measuredelectronically with light scattering. |
|
|
Anisocytosis is...? |
abnormal size variation in RBCs |
|
|
Poikilocytosis is...? |
abnormal SHAPE of RBCs; target cells (obstructive jaundice, liver disease) elliptocytes (hereditary elliptocytosis + irondeficiency), sickle cells(HbS polymerisation;genetic), schistocytes (fragements) |
|
|
Atypical lymphocytes are typical of? |
Glandular fever/infectious mononucleosis *Glandular fever: EBV (Herpes) infection of B-cells via CD21 receptor + infected B cell proliferates & shows EBV antigens; therefore T-cell mediated response & acute infection resolved but life-long sub-clinical infection |
|
|
Left shift =? |
increase in non-segmentedneutrophils or neutrophil precursorsin blood |
|
|
Toxic granulation=? |
heavy neutrophil granulation due to infection, inflammation + tissue necrosis; also in normalpregnancy |
|
|
Hypersegmented neutrophil due to lack of? |
lack of vit B12/folic acid |
|
|
Rouleaux = Howell-Jolly body= Heinz bodies= |
Rouleaux = RBC stacks (alterations in PP) Howell-Jolly body= nuclear remnant in RBC (due to lack of splenic function) Heinz bodies= denatured haemoglobin; removed by spleen |
|
|
Haemostatic plug formation steps? |
vessel constriction (initialresponse, more important in small vessels, localcontractile response) unstable plug (two steps = plateletadhesion to damaged wall + plateletaggregation) plug stabilisation with fibrin(unstable plug breaks down on its own, fibrin network formation stabilises) fibrinolysis (plug broken down, clot dissolution, vessel repair). |
|
|
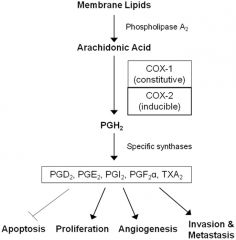
Prostaglandin metabolism? |
Products= prostacyclin in endothelial cells & Thromboxane A2 in platelets |
|
|
Aspirin is an inhibitor of which enzyme? |
COX inhibitor |
|
|
2 clotting cascade pathways? |
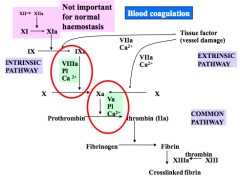
INTRSINIC + EXTRINSIC (briefly describe) |
|
|
Fibrinolysis initiated by which 2 proteins? |
Plasminogen (pp- plasma protein) & tissue plasminogen activator (tPA) Plasminogen -> plasmin by tPA ->breaks down clot |
|
|
What is APTT & what is it used for? |
Activated Partial Thromboplastin Time; detects intrinsic + common pathways abnormalities & measures clotting time; used to monitor heparin treatment (*-PT used to monitor warfarin treatment + extrinsic pathway abnormalities) |
|
|
MOA of Warfarin (anticoagulant) + indication? |
Warfarin inhibits vit K (inhibits assembly of active complexes on plateletsurface + reduces thrombin production)so stopgamma carboxylation by vit K Epoxide Reductase (stops clottingfactors binding to platelet surface) Used for LONG-TERM anticoagulant therapy (after treated for venous thrombosis + atrialfibrillation) |
|
|
MOA of Heparin (anticoagulant) + indication? |
Potentiates action of anti-thrombin by binding to it (so ↑f10a + thrombininhibition) & changes reactive loopposition Used for immediate anticoagulation in venousthrombosis + pulmonary embolism * Has TWO forms = low molecular weight heparin (favoursf10a inhibition) + standard/unfractionatedheparin (inhibits both). |
|
|
MOA & examples of anti platelets + indications? |
ADP receptor antagonists +COX1 antagonists: clopidogrel, abciximab (antibody – gp2b/3a antagonist), tirofiban (small molecule – gp2b/3a antagonist) Used in CVD; combos for angioplasty, stents |
|
|
Functions of: Gp1a Gp1b Gp2b/3a? (on platelets) |
Gp1a= allows platelets to bind DIRECTLY to exposed collagen Gp1b= VWF binds to collagen then platelets bind to VWF through Gp1b (INDIRECT) LACK= Bernard Soulier Syndrome Gp2b/3a=(on activated platelets) fibrinogen binds Lack=Glanzann’s Thrombasthenia |
|
|
Function of alpha granules on platelets? |
alpha granules – storage for proteins (factor 5, VWF), released when platelet activated (Also thrombin R and Gp on surface of platelets) |
|
|
Define Anaemia & what are 3 types (+ causes of each)? |
Low Haemoglobin concentration in a given volume of blood Microcytic (usually hypochromic,common causes are haem synthesis defect (irondeficiency, chronic disease) + globinsynthesis defect/thalassaemia (α or β chain synthesisdefects)) --> leads to reticulocytosis Normocytic Macrocytic (Abnormal HAEMOPOIESIS – failure to divide properly due to lack of B12 of folic acid, dugs that interfere with DNA synthesis:Chemotherapy, Azathioprine, liver disease/ethanol toxicity, Haemolytic anaemia, Major blood loss) |
|
|
Mechanisms of normocytic normochromic anaemia + causes? |
Mechanisms: Reduced production of Red cells by thebone marrow Loss of blood – haemorrhage Reduced survival of RBC’s in thecirculation – haemolytic Pooling of RBC’s in an enlarged spleen Causes: Peptic ulcers, oesophageal varices,trauma, hypersplenism (portal cirrhosis) Failure production of RBC’s: Early stages of iron deficiency, renal failure, bone marrow failure/suppression, Bone marrow infiltration. |
|
|
Define Haemolytic anaemia + its effects on vasc system? (also what do you expect to find?) |
Anaemia resulting from shortened survival of red blood cells in the circulation (can be inherited- sickle cell/G6PD def/hereditary spherocytosis or accquired- autoimmune, drugs) Intravascular:very acute damage Extravascular:defective red cells removed by the spleen Normochromic,normocytic/macrocytic, morphologically abnormal RBC’s, Evidence of increasedred cell breakdown, evidence of increased bone marrow activity |
|
|
What is hereditary spherocytosis & its treatments? |
Loss of cell memb w/o loss of cytoplasm. – Hereditary intrinsic defect
Cells increased MCHC Redcells become larger, rounder, and less flexible. Can’t move out of spleensinusoids so prematurely destroyed by spleen – extravascular haemolysis
Leads topolychromasia and Reticulocytosis
TREATMENT: Splenectomy + vitamins (folic acid, B12 and iron) |
|
|
Describe iron absorption in gut + what is the role of hepicidin? |
Movesfrom gut lumen into cell via Haem Carrier Protein/HCP-1 (Heme) or DMT-1 (Fe2+) Once incell moved to BM where enters blood via ferroportin Once inplasma binds to Transferrin Hepcidin= Keyregulator of the entry of iron into the circulation If hepcidin is high – indicates high iron in blood |
|
|
Role of ferritin & its levels in iron deficiency & chronic disease? |
Acute reactive protein + bind to iron and stores it (so indicates levels of iron stores in body)
Irondeficiency – Low Chronicdisease – High (BC IT IS ACUTE REACTIVE PROTEIN)
(* Transferrin -carrier protein for iron in the blood- levels: Irondeficiency – Increases Chronicdisease – Normal/Low) |
|
|
Why is ABO compatibilty important in blood transfusions? |
ABO incompatible transfusion --> fatal antibody-antigen interaction ---> agglutination then, cytokinestorm/lysis/cardiovascular collapse/death |
|
|
Why is it dangerous when RhD–ve mother has an RhD+ve baby? |
SENSITISATION: RhD negative CAN make anti-D antibodies (IgG) AFTER exposed to D antigen – exposed by transfusion or inpregnancy (RhD+ foetus). Anti-D ABs can cross placenta --> foetal RBChaemolysis --> hydrops fetalis --> death |
|
|
FFP (what is it + how it is produced/used)? |
FFP = Fresh frozen plasma Stored at -30˚C (frozen with6hrs, preserves coagulation factors + separated into cryoprecipitate + supernatant); 2yrshelf life; thawed at room temp.before use (proteins ‘cook’ at high temp.), use within an hour (coagulation factors degenerate) |
|
|
Platelets (how is it stored + matched)? |
Stored at room temp. (22˚C), constantly agitated (preventsaggregation) 5 day shelf life(risk bacterial infection); no need tocross-match but needs same ABO group (plateletshave low ABO levels) ONE pool from 4 donors is enough for 1 dose. |
|
|
RBCs (how is it stored + used)? |
packed cells (plasmaremoved); stored in 4˚ for 5 weeks inefficient to freeze blood – loseRBCs when thawed |
|
|
When is O2 dissociation curve shifted to the right? |
By factors that stabilise deoxyHb(decrease affinity, e.g. H+ +2,3-DPG + CO2 = BohrEffect) – so need higher [O2] for binding NB: As more O2 binds, Hb switches to relaxed form, can accommodate more O2!! |
|
|
Sicke Cell Anaemia (genetic cause, complications and effects) |
Point mutation at codon 6 so valine is substituted for glutamic acid --> HbAS (2 normal alpha chains and 2 variant beta chains) Complications: HbS causes formation of tactoid fibres that cause deoxyHb to form intratetrameric contact to form long polymers in the RBC, damaging it and distorting its shape. Effects: SICKLE CELL ONLY LASTS 20 days + no hypoxia as HbS readily gives up O2 at respiring tissues- lower affinity- so ANAEMIA); Acute chest syndrome; Pulmonary hypertension (free Hb depletes NO so vasoconstriction); asymptomatic and normal blood count |
|
|
What is used to distinguish between alpha and beta thalassaemia? |
Increased HbA2 levels in beta thalassaemia (found by electrophoresis) |
|
|
What are the iron-containing proteins (+ food)? |
Hb (biggest store; Fe2+ at centre), ribonucleotide reductase, myoglobin, cox, succinate dehydrogenase,cytochrome a/b/c, cytochrome p450, catalase. Food = meat, fish, vegetables, whole grain cereal, chocolate (* NB: Fe3+/Ferric iron cannot be absorbed- Tea converts Fe2+ to Fe3+ WHEREAS Orange juice increases Fe2+ absorbing ability) |
|
|
Why are B12 and folate vital? |
Both needed for the synthesis of deoxythymidine(dTMP), which is a crucial building block in DNA synthesis. |
|
|
Describe B12 absorption |
B12 binds to R protein (transcobalamin 1) Gastric parietal cells secrete Intrinsic factor B12 enters duodenum where it is displaced bypancreatic enzymes Free it binds to intrinsic factor In terminal ileum B12-intrinsic factor complexenters via receptor into cells.
Circulation B12 binds to Transcobalamin 2 makingit active B12 |
|
|
B12 deficiency tests? |
Neurologicalexamination, serum B12 level, plasma homocysteine (high in both B12 and Folatedeficiency), Serum methyl malonic acid levels (not freely available),holotranscobalamin levels (active B12) + Schilling test (not used anymore) |
|
|
Clinical features of a patient with a B12 and folic acid deficiency? ("JAAWS G!!") |
Jaundice: Ineffective erythropoiesis Anaemia: macrocytic, megaloblastic – SOB, weak,fatigue Angular Cheilosis: soreness in the corner ofyour mouth Weight loss + change in bowel habit Sterility Glossitis: red, raw tongue, painful |
|
|
Causes of B12 deficiency + consequences + treatment? |
Causes: Diet , Malabsorption- Crohns, Coeliac, Pernicious anaemia Consequences: Macrocyticand megaloblastic anaemia – reversible with treatment, Neurologicalproblems due to demyelination, Subacutedegeneration of the spinal cord -Cognitiveimpairment, Opticatrophy, Macrocytosis Treatment: Injections of B12, 1000 ug, 3 times a week for2 weeks. Thereafter every 3 months |
|
|
Vit B12 is co-factor for methionine synthase for...? |
homocysteine --> methionine conversion – reaction releases methyl groups --> methylate DNA (crucial for DNA synth) (NB: homocysteine = homologue of the amino acid cytosine, convertedto methionine by methionine synthetase and vitamin B12. High levels of it associated with atherosclerosis and premature vasc disease) |
|
|
Prenicious anaemia (causes + consequences) |
= Lack ofintrinsic factor (NEEDED FOR B 12 ABSORPTION) Causes: Autoimmune atrophic gastritis Patientsmay have intrinsic factor antibodies (20-40%) or parietal cell antibodies(80-90%) Consequences: macrocytic, megaloblastic anaemia, neurological damage. |
|
|
Describe folate absorption + reasons for malabsorption |
folic acid (folate polyglutamates)hydrolysed (acid pH) --> monoglutamates; folates absorbed as pteroglutamates --> methylated in luminal cells --> tetrahydrofolates Malabsorption due to: Coeliac disease (gliadin sensitivity --> subtotal villousatrophy + crypt hyperplasia in duodenum; anti-glandin/transglutaminase antibodies/duodenal biopsy used to diagnose), Surgeryor IBS, Drugs (colestyramine, sulfasalazine, methotrexate,anticonvulsants, alcohol) |
|
|
Consequences of folate deficiency + how is it diagnosed? |
Megaloblasticanaemia, Neural tube defects – spina bifida andanencephaly, increased risk of venous thromboembolism Fullblood count, Blood film, Blood folate level, Serumfolate: diurnal variation and affected by recent changes in diet, Red cellfolate: b12 deficiency = high serum folate, low red cell folate |
|
|
How does malignant haematopoiesis in chronic myeloid leukaemia? |
mutation occurs at GM-CFCphase --> increased prolif of myeloid cells |
|
|
Immature WBC (myelocytes + metamyelocytes) in blood film is indicative of...? |
Acute leukaemia (low Hb + platelets) (Only mature WBCs in normal infec + granular neutrophils) |
|
|
Causes of neutrophilia? |
Infection, tissue inflammation, malignant (myeloproliferative disorders, CML), physical stress, corticosteroids |
|
|
Causes of eosinophilia? |
Parasitic infections, allergic diseases, Hodgkin's Disease (Hodgkin’s Disease – ↑mediastinal mass on chest x-ray, ↑IL5 secretion --> reactive eosinophilia), Malignant chronic eosinophilic leukaemia (PDGFR gusion gene- detected by FISH)
|
|
|
Causes of monocytosis? |
RARE + chronic infec; TB, Brucella, typhoid; viral = CytoMegaloVirus, varicella zoster;sarcoidosis; chronic myelomonocytic leukaemia (MyeloDysplastic Syndrome) |
|
|
Causes of lymphocytosis? |
If MATURE cells - reactive toinfection(big nucleus, littlecytoplasm); CLL (esp in elderly), oligoclonal expansion (all cells look alike), autoimmune/inflammatory If IMMATURE cells (larger, big nucleus, see nucleolus) - ALL (acute lymphoblastic leuk); 2*= infection (EBV --> Herpes, CMV, toxoplasma, infectious hepatitis, rubella, herpes), autoimmune disorders, neoplasia, sarcoidosis |
|
|
How to differentiate between polyclonal and monoclonal antibody responses? |
POLYCLONAL - in resp to infection. 50:50 divide of Ҡ/λ lightchains in antibodies MONOCLONAL - all B-cells make either Ҡ OR λ only (NOT as a result of infec.) |

