![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
What are the 4 main categories of antiarrhythmic drugs?
|
Na Channel Blockers
K Channel Blockers Ca Channel Blockers Pacemaker current Modulators |
|
|
What are the 3 major types of protein channels that moderate ion control?
|
Passive Channels
Electrogenic Pumps Gated CHannels |
|
|
What are the two types of Gated Channels and how do they function?
|
Ligand Gated Channels - G proteins with second messenger systems. Typically activated by phosphorylations. Are also usually selective for one type of ion.
Voltage gated - membrane voltage dependent (ie when an action potential changes the membranes voltage sufficiently they open) |
|
|
What are two type potentials of basic cardiac cells?
|
Fast - Long duration Action Potential
Slow - ???Short duration Action potenital |
|
|
What are the phases of the fast potential type cardiac myocytes and what occurs at each phase?
|
Phase 4 - Resting potential (voltage gated channels must open for phase 0 to begin)
Phase 0 - Sodium influx (slope is descriptive of conduction velocity: Steeper = Faster) Phase 1 - Early K efflux and Cl ions enter. Phase 2 - Voltage Gated Ca Channels open and Ca enters the Cell. For a short while the potassium leaving the cell is balanced by the calcium. Phase 3 - Repolarization phase (Ca Channels inactivate and close while K efflux continues and more K effluxes than Ca comes in) Phase 4 - Although we have returned to phase 4 we have an imbalance of intracellular Na and extracellular K which is rectified by a Na/K ATPase |
|
|
Identify each phase of the fast potential type cardiac myocyte and what antiarrhythmics affect it?
|
Phase 4 - ??
Phase 0 - Na Channel Blockers (decreases slope) Phase 1 - No antiarrhythmics Phase 2 - Ca Channel Blockers Phase 3 - K Channel Blockers work from Phase 0 to middle of phase 3. Phase 4 - ?? |
|
|
At what voltage do Na Channels become inactive?
|
+55mV
|
|
|
At what phase does the refractory period begin and end and why would we want to prolong it?
|
Begins at Phase 0 and ends at the midpoint of Phase 3.
Prolonging it allows the muscle more time to relax before the next contraction to reduce the possibility of the muscles remaining in tetany. To increase refractory period Slow down K efflux so that repolarization takes longer |
|
|
Where are Slow Potential Cardiac Myocytes located?
|
SA and AV node
|
|
|
How is the slow potential different from the fast potential?
|
Slow potentials have:
Higher resting membrane potential: -60mV Phases 4, 1, 2, 3 are the same as fast potentials Phase 0 is not mediated by Na but by L-type voltage gated Ca Channels (aye theres the rub). Because of this the slope of phase 0 is fairly flat and is slow depolarizing so slow conducting. |
|
|
How do slow potential cardiac myocytes function as an intrinsic pacemaker?
|
They have a leaky membrane caused by the periodic opening of Na or K channels allowing the charges to slowly equilibrate. However, in addition there are T type Ca channels which open as the membrane potential approaches threshold
|
|
|
How do beta agonists increase HR?
|
They are linked to Na and K channels in the slow potential cardiac cells by 2nd messenger systems. By increasing If depolarization can occur faster due to decrease time to spontaneous depolarization
|
|
|
How do Ca Channel antagonists slow HR?
|
They block the L-type voltage gated channels of the Phase 0 in the slow potential myocytes increasing depolarization time.
|
|
|
What broad pharmacological categories of agents are used to modulate phase 4 to change HR?
|
Muscarinic and Beta Agonists
|
|
|
What is an ECG?
|
Don't try to answer this! That would be just stupid!
|
|
|
What is the slowest conduction area of the heart?
|
AV Node
|
|
|
What do the following represent:
P wave PR interval QRS T wave with regards to heart tissue function? |
P wave - Atrial depolarization starting with the SA node
PR interval - time to traverse through the AV node QRS - Ventricular depolarization T wave - Ventricular repolarization |
|
|
If you give a Na channel blocker what would you see on an ECG?
|
Widening of the QRS because of decrease of the speed of depolarization on the fast potential cells.
|
|
|
What will happen if you give a Ca channel blocker?
|
Decrease in Phase 0 of the slow potential causing a slowing of AV coduction which shows up as an increase in the PR interval and causes an increase in the time for SA node depolarization. So think decreased ionotropy and chronotropy!
|
|
|
What would happen to the heart on an ECG with a class III drug?
|
Increased repolarization time causing a lengthening of the QT interval
|
|
|
What could lengthening of the QT interval mean in regards to antiarrhythmic drugs?
|
Phase 0 lengthening causing increased depolarization time or slowed repolarization.
|
|
|
What utility would a Na or K channel blocker have on the AV node?
|
Minimal to none because they are slow potential cells with phase 0 onset by Ca channels not Na channels. And there is no phase 1 or 2 so no K channel blocker effect. SA node will be affected similarly however there may be an effect due to Na and K If current modifications (I don't know the last thing for sure)
|
|
|
What are some presumed causes of arrhythmias (you don't have to know these exactly but get a general idea and think on it some)
|
Changes in automaticity of Phase 4 or ectopic focus
Changes during repolarization: early after depolarization (a spontaneous firing of cells due to delayed refiring)or Delayed after depolarization(Most post MI arrhythmias are these. May also be Digitalis induced) Reentry Mechanisms - circular depolarization of the heart caused by a unidirectional conduction block through the tissue.) |
|
|
What effects on the heart does digitalis toxicity have?
|
It can cause elevated internal levels of Ca inducing an arrhythmia.
|
|
|
What is the meaning of the classification of each of the following arrhythmias:
Atrial tachycardia Ventricular Arrhythmia Junctional Arrhythmia Supraventricular Arrhythmia |
Atrial Tachycardia is an arrhthmia whose origin is the atria and is fast
Ventricular arrhythmia is a pacemaker in the ventricle Ventricular Tachycardia is a rhythm that starts int he ventricle Junctional arrhythmia is an arrhythmia in and around the AV node Supraventricular arrhythmia is anything above the ventricle. |
|
|
What is meant by an escape rhythm?
|
Typically SA node is the pacemaker because it is fastest, but if it doesn't function properly the heart keeps going from (in order) AV node, his purkinje, spontaneous cell depolarization.
|
|
|
What is the main treatment for most life threatening arrhythmias (v-tach and v-fib)?
|
Cardioversion (1.0)
|
|

Fill in the action and the drugs for these antiarrhythmics.
|
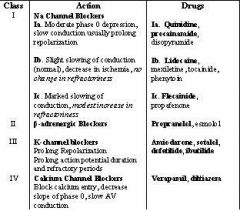
Copied from someone!
|
|
|
What effects are seen with Class IA, IB, and IC drugs, the ??? blockers?
|
Na-channel blockers
IA - slight widening of QRS and decrease in the slope of Phase 0 IB - No change in phase 0 or QRS IC - Marked widening of QRS and a large increase in the slope of phase 0 |
|
|
What are the 2 main effects of Class II agents, the ??? blockers?
|
Beta Blockers cause decrease phase 4 depolarization (catecholamine dependent) and slowing of the conduction rate of the AV node (affecting the Ca current in Phase 0)
|
|
|
What do Class III drugs do, the ??? blockers?
|
K-channel blockers
Increases action potential duration and refractory period |
|
|
What doe the Class IV agents do, the ??? Blockers?
|
Ca-Channel Blockers
Decrease conduction in the AV node. |
|
|
What are the three states of the Na channels and what do they mean?
|
Resting - m gate is closed and the h gate is open (read for depol)
Activated - depolling m gate opens and h gate stays open inactive - h gate closed m gate still opened but nothing happening because h gate is now closed. |
|
|
What is the effect of administration of TTX (tetrodotoxin from the puffer fish)?
|
the Na channels m-gate remains closed so resting state can't be changed to active
|
|
|
How do class I drugs work on the sodium channels?
|
they bind bothe the inactive and the active state preventing change.
|
|
|
What differentiates class I A, B, or C drugs?
|
Onset/Offset kinetics - the time they stay bound (tau)
|
|
|
Which class I drug has the shortest and the longest tau?
|
IB - Shortest
IC - Longest |
|
|
What is meant by a phasic block?
|
When giving lidocaine to v-tach patients heart rate decreases till it reaches a resting rate at which lidocaine won't affect the heart rate anymore. So essentially the higher the heart rate the more the effect!
|
|
|
What governs tonic vs phasic block?
|
Long Tau vs Short Tau - Class IC vs Class IC and how long the effect is.
A long Tau causes a tonic block while a short Tau causes a phasic block. |
|
|
What channels do Class IA block and what are their effects?
|
THey block both Na channels and K channels leading to a decrease in the slope of phase 0 and an increase in the action potential duration (moderate tau action)
|
|
|
Under what arrhythmic condition might Quinidine be contraindicated, why and what can be done?
|
Superventricular arrhythmias because quinidine is an anti-cholinergic causing a block say of 2:1 or 3:1 to become 1:1 allowing all pulses to go through the node. To combat this utilize a beta blocker, CCB, or digitalis before quinidine to slow the AV conduction first. Then quinidine can get rid of the reentry
|
|
|
What side effect is a hallmark of drugs that increase the QT interval and what is the primary treatment?
|
Torsades des pointes
Magnesium is the primary treatment |
|
|
What are the administration methods for Lidocaine with regards to arrhythmias?
|
IV only because of 95% first pass metabolism and very fast onset/offset time.
|
|
|
What channels are blocked by Class IB drugs and what are they used to treat??
|
ONly sodium channels
Only for V-tach (doesn't affect atrial or AV node tissue) |
|
|
What drug is an orally active form of lidocaine and what drug is a tricyclic antidepressant that is used to treat digitalis induced arrhythmias?
|
Mexilitine
Phenytoin |
|
|
What was the purpose of Class IC drugs?
|
Treat PVCs in MI patients
|
|
|
Describe some benefits of beta blockers?
|
Decrease AV conduction
Decrease oxygen consumption Indirectly decrease ventricular arrhythmias Disrupts reentry loops near the AV node |
|
|
What does amiodarone do?
|
Ca channel blocker, beta blocker, Na channel blocker, K channel blocker... oh wait doesn't bind to alpha channels... wow!
|
|
|
What is the drug of choice for v-tach and vfib in the ER?
|
Amiodarone
|
|
|
What does the ECG look like with Amiodarone?
|
Increased PR interval
Widened QRS Increased QT interval |
|
|
What causes people to turn into smurfs based on toxicity and what is the half life of Gargamel drug?
|
Amiodarone
Half life of Freaking 3.5 months!! |
|
|
What does Sotalol do and what class drug is it?
|
Beta blocker and K channel blocker
It is a Class III |
|
|
What do the new drugs Dofetilide and Ibutilide do and what class are they?
|
They are Class III drugs and they block specific sub class of K channel
|
|
|
What is the function and utility of Adenosine administration in the heart?
|
Causes a decrease in heart rate and breaking of AV node re-entry by decreasing AV conduction through activation of an inward K current hyperpolarizing the AV node. You can also cause asystole for 5 seconds before escape. IV only
|
|
|
What is digitalis and how does it work?
|
It is a cardiac glycoside and is an anti-arrhythmic that slows AV conduction but also increases vagal tone while decreasing sympathetic tone
|
|
|
What would atropine be used for in the heart?
|
Treats vagal bradycardia
|
|
|
What would you use Magnesium for in the heart?
|
Treatment for Torsades des pointes
|

