![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
102 Cards in this Set
- Front
- Back
|
what is the most common etiology for peripheral vascular disease?
|
Atherosclerosis
|
|
|
what area of the body is most affected by peripheral vascular disease?
|
lower extremities- calf areas
|
|
|
what is the primary symptom of peripheral vascular disease? what makes it better and worse?
|
Claudication: Aching, cramping, fatigue, weakness in the calves, thighs or buttocks brought on by walking and completely relieved after a few minutes of rest. Relieved with rest. Worse with exertion. Predictable.
|
|
|
what will you see of PVD on PE?
|
smooth, shiny, hairless skin on lower extremities.
Diminished or delayed distal pulses. Severe ischemia causes pallor, cyanosis, decreased skin temperature, ulceration and may cause gangrene |
|
|
how do you usually make the diagnosis of PAD?
|
the signs and symptoms
|
|
|
what is the ankle-brachial index? what's normal? what is PVD's index?
|
In normal patients, the systolic blood pressure in the leg is slightly higher than in the arm (ankle-brachial index > 1.0). In PVD, the index decreases. <.9=PVD
|
|
|
what is the function of ultrasounding for PAD?
|
to quantify the extent of dz. May also help dx those pts with noncompressible vessels
|
|
|
what happens to the ankle-brachial index as the disease progresses?
|
the index with decrease
|
|
|
what are the three phases of treatment of PAD?
|
1) conservative, 2) medical, 3) surgical
|
|
|
what are the tx options of conservative therapy?
|
lifetyle changes- regular walking may increase distance prior to claudication up to 400%. STOP SMOKING.
|
|
|
what are the medical txs that we can use for PAD?
|
pentoxifylline, cilostazol, lipid lowering agents, HTN agents, aspirin, clopidogrel
|
|
|
which medical tx looks the most favorable?
|
cilostazol
|
|
|
what are the indications for surgery?
|
-severe claudication that is resistant to medical therapy
-limb threatening ischemia -vasculogenic impotence |
|
|
what is acute limb ischemia?
|
VASCULAR EMERGENCY!
Sudden occlusion of a peripheral artery is caused by either arterial embolism or thrombosis in situ. |
|
|
what are the two major places that we get thrombi from?
|
deep veins and left atria (during a-fib)
|
|
|
what are the symptoms of limb ischemia from an arterial embolism?
|
Sudden onset of symptoms without history of claudication. Pain!
|
|
|
DVT vs Acute Limb Ischemia, how can you tell the difference?
|
DVT- warm foot or swelling because you are not getting a good outflow of blood.
ALI- cold, cyanotic and not swelling |
|
|
on physical exam, what does acute limb ischemia look like?
|
Cold, cyanotic (bluish) extremity
Absent pulses distal to the occlusion |
|
|
what two techniques can you use to diagnose acute limb ischemia? what can each one of these techniques determine?
|
hand-held doppler- assess flows at different arterial segments
transesophageal echocardiography (TEE)- to determine the potential cardiac source. |
|
|
what is the tx for acute limb ischemia?
|
anti-coag (IV heparin)
embolectomy catheter-directed infusion of plasminogen activator (tPA), a fibrinolytic emergent amputation if tissue necrosis |
|
|
how big is a normal aorta? when is it concerned an aneurysm? when does the size of the aorta start to become worrisome and requires intervention?
|
2 cm; 3cm; >5 cm
|
|
|
what is the major concerns of AAA's?
|
rupture which is an immediate life-threatening condition
|
|
|
In what type of population are AAA's more common?
|
older adults
|
|
|
what are the causes of AAA's? what is the main one?
|
Atherosclerosis*, Cystic Medial Necrosis (Marfans, Ehlers-Danlos), vasculitis with connective tissue disease (Takayasu’s arteritis, giant-cell arteritis), chronic infection (syphilitic aortitis), and trauma.
main- atherosclerosis |
|
|
when the risk of a rupture start to increase?
|
when diameter >5 cm
|
|
|
what are the symptoms and Signs of AAA?
|
nontender pulsatile mass BELOW umbilicus if <5 cm.
Hypotension, acute abdominal/ back pain |
|
|
what should prompt consideration of aneurysm rupture?
|
elderly pt with hypotension, acute abdominal/ back pain.
|
|
|
how do you diagnose AAA?
|
duplex ultrasonography
CT, MRA allow visualization of the thoracic and abdominal aorta and iliac arteries and its branches |
|
|
how do you tx an AAA (if they are inbtwn 3 and 5 cm)?
|
stop smoking
conrtol BP lower cholesterol come in for an exam every 6-12 months |
|
|
how do you tx an expanding AAA? (ie 6 months ago it was 3 cm and now its 4)
|
surgical repair.
Open surgical repair or percutaneous endovascular graft placement. |
|
|
where does the aortic dissection typically occur?
|
in thoracic aorta
|
|
|
what are the risk factors for aortic dissection?
|
HTN, cocaine use, trauma (like a car accident), herditary CT disease, vasculitis
|
|
|
what are the two types of aortic dissections based on the stanford system?
|
type a- involves the ascending aorta
type b- involves the distal aorta |
|
|
what are the three types of aortic dissection based on the debakey system?
|
type 1- entire aorta
type 2- only ascending aorta type 3- only descending aorta |
|
|
what is the key symptom of aortic dissection?
|
ripping or tearing pain
|
|
|
what can retrograde propragation of the Aortic dissection cause?
|
pericardial tamponade or CADissection w/ acute MI
|
|
|
how would you diagnose an Aortic dissection?
|
CT angiography and TEE (slow)
|
|
|
which type of aortic dissection is fatal without emergent repair (based on the stanford system)?
|
type A
|
|
|
besides for Type B, why else would surgery be required for pts with aortic dissection?
|
if blood flow is compromised to the legs, kidneys or other viscera.
|
|
|
what can prevent the growth of dissections and avoid aneurysms?
|
tight BP control
|
|
|
what areas does Raynaud's phenomenon mainly affect?
|
toes and fingers
|
|
|
what are the physical characteristics of Raynaud's?
|
episodic bilateral digital pallor, cyanosis and rubor
|
|
|
what relieves raynaud's?
|
warmth
|
|
|
what gender is more affected by Raynaud's?
|
women
|
|
|
what are the symptoms of raynaud's phenomenon?
|
recurrent episodes of digital ischemia with characteristic white- blue-red color sequence
|
|
|
what happens to the fingers inbetween attacks of raynaud's phenomenon?
|
the fingers are completely normal
|
|
|
what is the tx for raynaud's phenomenon?
|
avoid cold temperatures
protect hands aspirin calcium channel blockers reduce frequency and severity of vasospastic episodes |
|
|
what is Beurger's Disease? What age and gender is more commonly affected?
|
A non-atherosclerotic disease of the small-medium-sized arteries, veins and nerves of the arms and legs affecting mostly young men before the age of 45 years.
|
|
|
what is the cause of Buerger's disease?
|
unknown.. all pts have a history of heavy tobacco addiction
|
|
|
what are the symptoms of Buerger's disease?
|
claudication of the feet, legs, hands or arms.
skin changes (ischemia, ulcerations) found mainly in the extremities |
|
|
how do you diagnose Buerger's disease?
|
clinical presentation and biopsy which will show inflammatory intramural thrombi within the arteries and veins
|
|
|
what is the tx of buerger's disease?
|
complete tobacco and nicotene abstinance!
- iloprost (reduces limb ischemia and improve healing) -surgical amputation required in >40% of those pts who do not quit smoking |
|
|
what is considered a fever?
|
100.4 F
|
|
|
what is giant cell arteritis?
|
inflammation of the lining of the medium-large arteries
|
|
|
what type of vasculitis is giant-cell arteritis?
|
large vessel
|
|
|
T/F
Giant cell arteritis is immune-mediated |
true
|
|
|
what age group is most directly affected by giant-cell arteritis?
|
elderly >50 yoa (females>males)
|
|
|
worst headache i'v ever had.
|
subarachnoid hemorrhage
|
|
|
what are the symptoms of giant cell arteritis?
|
headache from temporal arteritis
jaw claudication from ischemia of masseteres visual loss due to ophthalmic artery dz |
|
|
what would you see on PE for giant cell arteritis?
|
sclap tenderness in the temporal artery area
pale edematous fundus |
|
|
what studies prove giant cell arteritis?
|
elevated CRP and sed rate (>50)
diagnosis confirmed by biopsy of arterial tissue |
|
|
what is the tx for giant cell arteritis?
|
high dose corticosteroids.
methylprednisolone |
|
|
do you wait for the biopsy befre treating giant cell arteritis?
|
NO!!
|
|
|
what is takayasu's arteritis?
|
Granulomatous vasculitis of the aorta, its main branches and the pulmonary artery.*
|
|
|
Who is most commonly affected by takayasu's arteritis?
|
young women of asian descent
|
|
|
what is the most common sign of takayasu's arteritis?
|
HTN
|
|
|
what can the inflammatory process of takayasu's arteritis lead to?
|
stenosis and/or aneurysm formation
|
|
|
what can be found on physical examination for takayasu's arteritis?
|
bruits over subclavian artery and aorta
diminished brachial pulses low brachial artery BP |
|
|
how do you tx takayasu's arteritis?
|
corticosteroids- 1st line
immunosuppressive agents- MTX |
|
|
what is an arteriovenous fistula?
|
Abnormal vascular communications which shunt blood flow from the arterial system directly into the venous system, bypassing the capillary beds that normally ensure optimal tissue perfusion and nutrient exhange.
|
|
|
what are the symptoms of AV fistula?
|
pulsatile mass, bleeding from spontaneous rupture, neurologic defiicts or seizures (If AVM is in the brain)
|
|
|
how do you diagnose AV fistulas?
|
MR, CT, Conventional angiography
|
|
|
what is venous thromboembolic disease?
|
The presence of coagulated blood, or thrombus in a vein. Encompasses both DVT (Deep Venous Thromboembolism) and PE (Pulmonary Embolus).
|
|
|
what is the incidence of venous thromboembolic disease?
|
1/1000 pts
|
|
|
what is the virchows' triad?
|
3 predisposing factors for venous thromboembolic disease
1. endothelial damage 2. venous stasis 3. hypercoagulation |
|
|
what can cause endothelial damage?
|
surgery or trauma
|
|
|
what can cause venous stasis?
|
prolonged bed rest or immobilization
|
|
|
what can cause hypercoagulation?
|
common with cancer and birth control pills
|
|
|
what is Trousseau's syndrome?
|
Migratory thrombophlebitis with noninfectious vegetations on the heart valves typically in the setting of mucin-secreting adenocarcinoma.
|
|
|
what is diseases are included under hypercoagulable states?
|
hereditary diseases such as deficiences in antithrombin III, protein C or protein S
|
|
|
what are some etiologies for DVTs?
|
surgery, immobility, birth control pills, atrial fibrillation, cancer, heart failure, pregnancy, venous catheters
|
|
|
how far down do we go to search for DVTs with ultrasound?
|
no lower than the popliteal artery
|
|
|
where do most DVT's begin?
|
in the calf
|
|
|
what are the symptoms of DVT?
|
pain and/or swelling!!!!
if in UE: superior vena cava syndrome and throacic outlet obstruction |
|
|
what would you see on physical exam of DVT?
|
Tenderness, erythema, warmth, and swelling below the site of thrombosis.
Pain with dorsiflexion of the foot (homan's sign) may be present |
|
|
what is a highly sensitive indicator of DVTs? when would you use this indicator?
|
D-dimer; use if your suspicions are low.
|
|
|
how do you diagnose DVT?
|
d-dimer (very non specific)
duplex US |
|
|
what is the tx for DVT?
|
1st- heparin (IV), or lovenox (SQ)
2nd- warfarin start after 1st meds |
|
|
how would you tx and upper extremity DVT in young pts?
|
consider thrombus removal by fibrinolytic infusion thru a catheter inserted directly into the affected vein or mechanical fragmentation of the thrombus
|
|
|
when would consider giving an inferior vena cava filter?
|
pts with proximal DVT who 1) either have an absolute contraindication to anticoagulation or 2) develop recurrent PE despite adequate anticoag.
|
|
|
T/F
Inferior vena cava filter reduces the incidence of PE and the recurrent DVTs |
FALSE
they increase the risk of recurrent DVTs |
|
|
when does a PE occur?
|
PE occurs when a thrombus dislodges from the deep veins of the upper or lower extremities and embolizes to the arterial blood supply of the lungs where it then blocks a pulmonary artery.
|
|
|
what are the symptoms of PE?
|
sudden onset of dyspnea, pleuritic chest pain, anginal chest pain, hemoptysis and syncope
|
|
|
pt comes into the ER complaining of chest pain, what MUST be on your diagnosis?
|
PE
|
|
|
what are the physical findings of a PE?
|
tachypnea, tachycardia, crackles, wheezing, pleural rub
|
|
|
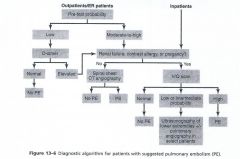
how do you diagnose a PE?
|
ABG- may reveal hypoxia
spiral CT of chest D-dimer (only use when index of suspicion is low) Spiral Chest CT angiography |
|
|
what is the modality of choice to diagnose PE?
|
spiral chest CT angiography
|
|
|
how do you tx PE?
|
anticoagulation-immediate!! IV Unfractionate Heparin
-warfarin after starting UFH -Thrombolytics reserve for pts with hypotension and/or severe hypoxemia |
|
|
how long to we continue anticoagulation in PE pts?
|
3 to 6 months after PE due to trauma or surgery.
-indefinitely for VTE due to cancer -Indefinitely for idiopathic VTE |
|
|
who should be give venous thromboembolism prophylaxis to?
|
surgical pts
hospitalized pts w/ acute illnesses (CHF, inflammatory disease, 3 days or longer of immobilization) |
|
|
what does VTE prophylaxis involved?
|
heparin, LMWH, pneumatic stockings, TED hose, early ambulation
|
|
|
GOOD TO KNOW
|

