![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
239 Cards in this Set
- Front
- Back
|
which hormone stimulates the maturation of red blood cells?
|
erythropoietin
|
|
|
what is the lifespan of a RBC?
|
120 days
|
|
|
Name the dz: back pain, decreased Hb, increased creatinine?
|
mulitple myeloma
|
|
|
with acute blood loss, what effect is there on platelets and WBCs?
|
there may be a reactive thrombocytosis and leukocytosis
|
|
|
What Dur(T)ie Salmon stage do you see physical findings of multiple myeloma?
|
Stage III
|
|
|
What indicates poor prognosis in multiple myeloma?
|
increased creatinine, elevated beta-2 microglobulin
|
|
|
What is MGUS?
|
m-spike w/o neoplasm or symptoms
|
|
|
what shape are erythrocytes?
|
biconcave discs
|
|
|
t/f... erythrocytes do not have organelles
|
true
|
|
|
which cells are the last in the erythroid line to have a nucleus?
|
normoblasts
|
|
|
which type of malaria is associated with the greatest morbidity and mortality
|
P falciparum
|
|
|
what does the haemopoietic stem cell look like?
|
small to intermediate sized lymphocyte
|
|
|
What cells are likely to be found in the peripheral blood of a CML patient?
|
immature granulocytes at various stages
|
|
|
what is the source of erythropoietin?
|
kidney
|
|
|
what metals are required for normal haemopoiesis?
|
iron, manganese, cobalt
|
|
|
which vitamins are required for normal haemopoiesis?
|
B12, folic acid, C, E, B6, thiamine, riboflavin, pantothenic acid
|
|
|
what is the most common cause of anaemia?
|
iron deficiency
|
|
|
what is the laboratory hallmark of iron deficiency?
|
microcytosis
|
|
|
what is the definition of microcytosis?
|
mean corpuscular volume less than 80 femtolitres
|
|
|
what is the best measurement of overall iron stored in the body?
|
serum ferritin
|
|
|
With low grade lymphoma, what are common lab findings?
|
Nothing - usually pretty normal, just find messed up things in biopsy
|
|
|
In promyelocytic leukemia (a AML variant), what are some typical findings?
|
Lots of promyelocytes in marrow + blood; often have hypo or hyper granules, odd nuclei; maybe thromboses or hemorrhage. Treat w/ ATRA
|
|
|
what is the most common cause of macrocytosis?
|
excess alcohol consumption
|
|
|
which deficiency can cause profound neurological damage?
|
Vitamin B12
|
|
|
what is Vit B12 deficiency most commonly caused by?
|
poor absorption from the bowel (often associated with pernicious anaemia)
|
|
|
Hodgkin's and non-Hodgkin's lymphomas are often described in term of what?
|
Hodgkins: lymphocyte morphology +/or phenotype; NH: morphology +/or phenotype, + overall pattern (diffuse vs follicular)
|
|
|
what substance is secreted by gastric cells?
|
intrinsic factor
|
|
|
What are peripheral blood and bone marrow findings for a patient w/ B-CLL?
|
Small, mature, round lymphocytes; express B cell antigens, some Ig; >30% of cells in marrow
|
|
|
where does folic acid absorption occur?
|
jejunum
|
|
|
which deficiency affects the peripheral nervous system only?
|
folate
|
|
|
which two conditions are associated with reduced haemoglobin concentration of the erythrocytes and are characterised by microcytic hypochromic erythrocytes?
|
iron deficiency and thalassaemia
|
|
|
what is the best screening test for iron deficiency?
|
serum ferritin
|
|
|
What is MGUS?
|
Dx for an asymptomatic patient w/ a monoclonal protein, but you can't find the cells that are making it. 20-30% later develop PCM (no bone lysis)
|
|
|
Is nodular lymphocyte predominant HL a form of classical? Is nodular sclerosis HL?
|
Nodular lymphocyte is not: expresses CD45 + CD20, + cell = H+L (popcorn); nodular sclerosis: CD15 + 30+, no B or T , lots of collagen. Main difference: the classicals have HRS, non doesn't
|
|
|
which two conditions result in rapid falls in haemoglobin concentration?
|
haemolysis and blood loss anaemia
|
|
|
What is the bad cell in Burkitt lymphoma? What pattern does it present with?
|
small non cleaved lymphocyte or follicular B-blast. Rarely has follicular pattern
|
|
|
What are the most common types of NHL? What are the most aggressive?
|
B cell (except in kids); aggressive: precursor B or T cell lymphoblastic leukemia/lymphoma, and Burkitt's
|
|
|
where is haptoglobin produced?
|
liver
|
|
|
what are the common causes of chronic blood loss?
|
In the United States: menorrhagia, gastrointestinal bleeding.
Worldwide: hook worm disease (necator americanus) |
|
|
which two pathways in the white matter of the spinal cord are affected by B12 deficiency?
|
the dorsal columns and the lateral corticospinal tract
|
|
|
List the common symptoms of anemia as well as the symptoms of severe anemia.
|
Common: pallor, fatigue, dyspnea on exertion.
Severe: angina pectoris, glossitis, gastritis, koilonychia, and Plummer-Vinson syndrome. |
|
|
What are the iron study patterns in iron deficiency anemia?
|
Serum iron is low.
TIBC is elevated. Serum ferritin is low. |
|
|
what is anaemia?
|
reduction in red cell number, haemoglobin or haematocrit
|
|
|
why does haemoglobin reduce in pregnancy?
|
haemodilution
|
|
|
what is the normal range for reticulocytes?
|
0.5% - 1.5%
|
|
|
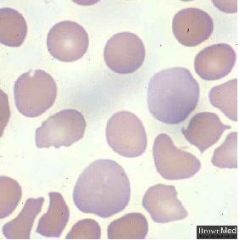
what fraction of a red blood cell is normally central pallor?
|
1/3
|
|
|
t/f... reticulocytes contains some RNA
|
true
|
|
|
what are the iron study patterns in the anemia of chronic disease?
|
Serum iron is low
TIBC is low. Serum ferritin is elevated. |
|
|
what is required for red cell production?
|
erythropoietin, vit B12, folic acid
|
|
|
where is erythropoietin produced?
|
kidney (and to a lesser extent the liver)
|
|
|
Which antibodies mediate warm antibody autoimmune hemolytic anemia versus cold agglutinin disease?
|
IgG: warm
IgM: cold |
|
|
what are the haematinics?
|
iron, B12, folate
|
|
|
What preventative measure can be taken to prevent erythroblastosis fetalis?
|
administer anti-D IgG antiserum to D negative mothers at the time of delivery of a D positive child. this causes fetal red cells to be removed from maternal circulation.
|
|
|
What are the possible causes of erythroblastosis fetalis?
|
Maternal alloimmunization to fetal Rh antigens.
ABO incompatibility. |
|
|
What is the pathophysiology of paroxysmal nocturnal hemoglobinuria?
|
Defect in the PIG-A gene causes impaired synthesis of the GPI anchor, which fixes CD55, CD59, and CD8 proteins to the cell surface. These proteins protect red cells from compliment mediated lysis.
|
|
|
What are the possible molecular defects in hereditary spherocytosis? What is its inheritance?
|
Spectrin, ankyrin, protein 4.1 or other RBC skeletal proteins.
Autosomal dominant. |
|
|
What is the pathophysiology of G6PD deficency? What is its inheritance?
|
Lack of G6PD reduces the body's ability to deal with oxidative stress. G6PD is an X-linked disorder.
|
|
|
what effect does anaemia have on viscosity of blood?
|
anaemia reduces viscosity of blood
|
|
|
what is the effect of reduced O2 delivery to tissues on blood vessels?
|
dilatation
|
|
|
which deficiency leads to both peripheral and central neurological signs?
|
B12
|
|
|
will deficiency of the haematinics be associated with a low or high reticulocyte count?
|
low
|
|
|
will haemolysis be associated with a low or high reticulocyte count?
|
high
|
|
|
What are the six symptoms of sickle cell anemia?
|
severe hemolytic anemia
chronic leg ulcers vaso-occlusive crises auto splenectomy aplastic crises (parvovirus) infectious complications (salmonella osteomyelitis) |
|
|
What are six clinical and laboratory signs of beta thalassemia?
|
severe anemia
severe splenomegaly distortion of skull facial bones and long bones microcytosis, hypochromia, target cells increased Hemoglobin F generalized hemosiderosis |
|
|
what type of anaemia will occur with marrow suppression/aplasia?
|
normocytic, normochromic
|
|
|
what type of anaemia do defects in Hb synthesis cause?
|
microcytic hypochromic
|
|
|
What is the spectrum of clinical abnormalities in alpha thalassemia according to the number of deletions?
|
one deletion: no abnormalities
two to three deletions: mild to moderate thalassemic symptoms four deletions: hydrops fetalis |
|
|
What is hepcidin?
|
A peptide hormone that decreases both intestinal iron absorption and the release of iron from macrophages. In anemia of chronic disease, proinflammatory cytokines induce hepatic synthesis of hepcidin. This causes serum iron to be low despite normal or even elevated iron stores (ferritin).
|
|
|
Where does the antigen-independent phase of plasma cell development occur?
|
bone marrow (heavy and light chain rearrangement, surface Ig expression)
|
|
|
Where does the antigen-dependent phase of plasma cell development occur?
|
spleen, LN (antigen presentation and somatic hypermutation)
|
|
|
when does rouleaux occur?
|
increased plasma proteins e.g. myeloma
|
|
|
which leakaemia is associated with Auer rods?
|
AML
|
|
|
What is plasmacytoma?
|
- isolated plasma cell tumor, or part of MM
- occurs in different sites (in skeletal or soft tissue) - skeletal involvement more likely progress to MM - local Tx with radiation |
|
|
what is the commonest form of anaemia?
|
iron deficiency
|
|
|
what are the two stores of iron in the body?
|
ferritin, haemosiderin
|
|
|
t/f... there is no effective excretion mechanism for iron
|
true
|
|
|
how is iron balance controlled?
|
iron absorption
|
|
|
what regulates iron absorption?
|
mucosal cells of proximal small intestine
|
|
|
what are the two pathways for dietary iron absorption?
|
iron attached to haem, iron in ferrous form
|
|
|
What are the two main clinical features of acute lymphoblastic leukemia (ALL)?
|
1. bone marrow failure
2. organ infiltration |
|
|
What does bone marrow failure result in?
|
1. anemia: pallor, lethargy
2. neutropenia: fever, malaise, infections 3. thrombocytopenia: bruises, bleeding |
|
|
what reduces ferric iron to ferrous form?
|
Dcytb (duodenal cytochrome b1)
|
|
|
what is the role of DMT1 (divalent metal transporter) in dietary iron absorption?
|
apical uptake
|
|
|
what transfers iron into the plasma from the enterocyte?
|
ferroportin (transfer is facilitated by hephaestin)
|
|
|
what is hepcidin?
|
peptide hormone secreted by liver
|
|
|
what is the function of hepcidin?
|
decreases functional activity of ferroportin
|
|
|
how does intestinal absorption relate to liver hepcidin expression?
|
absorption varies inversely with expression
|
|
|
which cells are destroyed by antibodies in pernicious anaemia?
|
parietal cells
|
|
|
what is the average daily loss of iron in men and non-menstruating women?
|
1 mg/day
|
|
|
Why would gout or renal impairement be a feature of CML?
|
excessive purine breakdown causing hyperuricemia
|
|
|
What are symptoms of myelodysplasia?
|
anemia
infections easy bruising/bleeding |
|
|
what is the most important lab marker of iron deficiency?
|
serum ferritin
|
|
|
what effect does iron deficiency have on serum transferrin?
|
raised
|
|
|
what percentage of oxygen in the blood is dissolved?
|
1.5%
|
|
|
You have determined that there is bone marrow failure (anemia, neutropenia, thrombocytopenia) and organ infiltration (sore bones) in a 4 year old girl. What is the most likely diagnosis?
|
ALL
|
|
|
what is the most common cause of vitamin B12 deficiency?
|
malabsoption due to inadequate intrinsic factor,disorders of terminal ileum; malnutrition due to chronic alcoholism
|
|
|
what is the Bohr effect?
|
oxygen carrying capacity of Hb at a particular PO2 is decreased by increased PCO2
|
|
|
what is the affinity of CO for Hb compared to oxygen?
|
200 times
|
|
|
what type of anaemia occurs in thyroid disease?
|
macrocytic
|
|
|
what volumes define microcytic, normocytic and macrocytic?
|
microcytic: <80 fl
normocytic: 80-99 fl macrocytic: >99 fl |
|
|
what type of anaemia occurs with impaired DNA synthesis?
|
megaloblastic (vit B12 or folate deficiency)
|
|
|
list some blood film changes in megaloblastic anaemia
|
oval macrocytes, aniso/poikilocytosis, hypersegmented neutrophils, may have low WCC and low platelets
|
|
|
how long do body stores of vitamin B12 last?
|
3-4 years
|
|
|
what is vitamin B12 bound to in the plasma?
|
transcobalamin (TC II)
|
|
|
where is vitamin B12 absorbed?
|
terminal ileum
|
|
|
what secretes intrinsic factor?
|
gastric parietal cells
|
|
|
what does B12 bind to in the stomach to travel to the terminal iluem for absorption?
|
intrinsic factor
|
|
|
which columns of the spinal cord are affected in B12 deficiency?
|
posterior and lateral
|
|
|
which peripheral fibres are affected in B12 deficiency?
|
peripheral sensory nerves
|
|
|
t/f... inadequate intake is a common cause of vitamin B12 deficiency
|
false, it is a very rare cause (only in true vegans)
|
|
|
What are some clinical features of Hodgkin's lymphoma?
|
1. painless, asymmetrical, firm superficial lymph nodes
2. splenomegaly (50%) 3. mediastinal enlargement 4. constitutional symptoms |
|
|
what is pernicious anaemia?
|
severe lack of intrinsic factor due to autoimmune disease affecting gastric parietal cells
|
|
|
is pernicious anaemia more common in men or women?
|
women (M:F 1:1.6)
|
|
|
which antibody is highly specific for pernicious anaemia?
|
anti-intrinsic factor (found in 95% patients)
|
|
|
how long do the body stores of folate last?
|
3-4 months
|
|
|
where is the body's store of folate?
|
liver
|
|
|
where is folic acid absorbed?
|
proximal jejunum
|
|
|
t/f... folic acid is absorbed via specific receptors
|
false, folic acid is absorbed via concentration dependent diffusion (B12 is absorbed via specific receptors)
|
|
|
when is there an increased need for folic acid?
|
pregnancy, prematurity, haemolysis, malignancy
|
|
|
which disease causes malabsorption of folate?
|
Coeliac disease
|
|
|
name some antifolate drugs
|
methotrexate, anticonvulsant, trimethoprim, alcohol
|
|
|
which measure of folate tests body stores not just recent intake?
|
red cell folate
|
|
|
name three situations in which serum folate will be raised
|
severe vitamin B12 deficiency
folic acid therapy sample haemolysed |
|
|
when might red cell folate be falsely normal?
|
blood transfusion
increased reticulocytes |
|
|
when will the peak reticulocyte response be observed after starting therapy for megaloblastic anaemia?
|
6-7 days
|
|
|
how long after beginning treatment for megaloblastic anaemia will the bone marrow be normoblastic?
|
48 hours
|
|
|
at what rate will the Hb rise after commencing treatment for megaloblastic anaemia?
|
Hb should rise by 10g/L per week
|
|
|
which cells are destroyed by antibodies in pernicious anaemia?
|
parietal cells
|
|
|
What are constitutional symptoms?
|
fever
pruritis (itching) weight loss weakness fatigue anorexia |
|
|
What are some clinical features of non-Hodgkin's lymphoma?
|
1. superficial (asymmetrical) lymphadenopathy
2. constitutional symptoms 3. oropharyngeal involvement 4. anemia 5. hepato/splenomegaly 6. other organ involvement |
|
|
A patient presents with asymmetric matted lymph nodes. Is it more likely to be leukemia or lymphoma?
|
Lymphoma
|
|
|
A patient presents with asymmetric lymph nodes, constitutional symptoms, splenomegaly and a sore throat. Is it more likely Hodgkin's or non-Hodkin's?
|
non-Hodgkin's sometimes presents with oropharyngeal symptoms
|
|
|
t/f... reduced affinity of oxygen for Hb is equivalent to a shift to the left of the O2-Hb curve
|
false, it is a shift to the right
|
|
|
list 4 factors that will decrease oxygen affinity for Hb
|
increased PCO2
acidosis increased temp increased 2,3-DPG |
|
|
A 60 year old patient presents with sudden severe anemia, thrombocytopenia and enlarged bleeding gums. What is the most likely diagnosis?
|
AML
|
|
|
In which hematologic malignancy is hypermetabolism a major feature?
|
CML
|
|
|
What are some clinical features of chronic lymphocytic leukemia (CLL)?
|
1. symmetric enlargement of cervical, axillary or inguinal nodes
2. anemia (thrombocytopenia) 3. splenomegaly (later stages) 4. immunosuppression |
|
|
how much iron do pregnany women lose every day?
|
3.5 mg/day
|
|
|
what is the average daily iron loss in menstruating women?
|
2 mg/day
|
|
|
How can abnormal platelet function present?
|
bruising, epistaxis, menorrhagia, hemorrhage
|
|
|
what is the sole physiologic means of iron transport?
|
transferrin
|
|
|
How does hypermetabolism present?
|
weight loss, lassitude, anorexia, night sweats
|
|
|
What are clinical features of chronic myeloid leukemia (CML)?
|
1. hypermetabolism
2. splenomegaly 3. anemia 4. abnormal platelet function 5. gout/renal impairement |
|
|
What is characteristic of the M4/M5 variants of AML?
|
gum hypertrophy
skin involvement CNS disease |
|
|
What is characteristic of M3 variant of AML?
|
disseminated intravascular coagulation (DIC)
|
|
|
What are clinical features of acute myeloid leukemia (AML)?
|
similar to ALL
mostly anemia, thrombocytopenia |
|
|
What does organ filtration result in?
|
tender bones
lymphadenopathy hepato/splenomegaly meningeal syndrome (headache, nausea, blurred vision) |
|
|
t/f... haem iron absorption is enhanced by ascorbate and meat and inhibited by phytates, bovine milk, tea and coffee
|
false, this is true for non-haem iron absorption (haem iron absorption is unaffected by composition of diet)
|
|
|
How do you Tx multiple myeloma?
|
1) alkyating agents (melaphalan, prednisone)
2) nonalkylating agents (vincristine, adriamycin, decadron) 3) thalidomide, revlimib |
|
|
What are the si/sx of hypercalcemia?
|
- ab pain, constipation
- confusion, lethargy - renal insufficiency (calcium is diuretic) |
|
|
How does multiple myeloma cause hypercalcemia?
|
osteoclast activating factors (mostly IL-1)
|
|
|
Criteria for Dx Multiple Myeloma:
|
1) M-spike in serum or urine
2) >10% clonal plasma cells in BM 3) end-organ damage 4) hypercalcemia 5) lytic bone lesions 6) anemia 7) renal insufficiency * hyperviscosity, amyloidosis |
|
|
How does multiple myeloma present?
|
- back pain, osteoporosis
- fatigue, anemia - high ESR - proteinuria |
|
|
What is multiple myeloma?
|
- diffuse plasma cell growth
- end organ damage |
|
|
t/f... most people with anaemia receive a transfusion
|
false, the only indication for transfusion is tissue hypoxia (severe anaemia)
|
|
|
What is MGUS?
|
- low grade clonal proliferation (<10% plasma cells in BM)
- asymptomatic - can convert to MM (1%) |
|
|
All the plasma cell disorders occur during the transition from _____ cells to plasma cells.
|
memory
|
|
|
what do oval macrocytes indicate?
|
B12 or folate deficiency
|
|
|
how many lobes does a hypersegmented neutrophil have?
|
>5
|
|
|
what do target cells indicate?
|
hypochromia
|
|
|
what is the normal size of a RBC compared to a lymphocyte?
|
RBC should be size of lymphocyte nucleus
|
|
|
What are possible causes of mechanical disruption leading to hemolysis? What is seen on the peripheral smear?
|
aortic valve prosthetics
disseminated intravascular coagulation thrombotic thrombocytopenic purpura smear shows schistocytes or helmet cells |
|
|
list 3 causes of macrocytic normochromic anaemia
|
B12 deficiency, folate deficiency, myelodysplasia, alcohol consumption
|
|
|
What is sickle-cell thalassemia?
|
Co-inheritance of hemoglobin S and thalassemia of the beta globin gene. Clinically similar to sickle cell anemia but less severe.
|
|
|
list some causes of haemolysis
|
immune attack on red cells (autoimmune, drugs e.g. methyldopa, alloimmune e.g. incompatible red cell transfusion, Rh disease), abnormal red cell membrane (HS), abnormal red cell metabolism (G6PDH deficiency), mechanical (malfunctioning prosthetic heart valve, DIC, malignancy)
|
|
|
Specifically, what is the genetic defect in hemoglobin S disorders?
|
A point mutation on chromosome 11 in codon six of the beta globin gene results in a substitution of valine for glutamic acid.
|
|
|
What percentage of African-Americans carry the hemoglobin S gene? What advantages does the gene confer?
|
Approximately 7%
The hemoglobin S gene confers resistance to malarial infection (Plasmodium falciparum). |
|
|
What is the inheritance of pyruvate kinase deficiency anemia?
|
autosomal recessive.
|
|
|
How can you differentiate the presentation of pyruvate kinase deficiency from G6PD deficiency?
|
In contrast to G6PD deficiency anemia, pyruvate kinase deficiency anemia is chronic and sustained.
|
|
|
What are sources of oxidative stress that can cause an episode of hemolysis in G6PD?
|
drugs such as primaquine (anti malarial), sulfonamides, other oxidant drugs.
fava beans infection |
|
|
what are the signs of anaemia?
|
pallor (conjunctival, palmar crease), cardiac decompensation (tachycardia, postural hypotension, CCF)
|
|
|
list the symptoms of anaemia
|
tiredness, headaches, dizziness, SOB, palpitations, angina (with pre-existing heart disease)
|
|
|
t/f... cardiac output increases in response to anaemia
|
true
|
|
|
what happens to senescent RBCs?
|
removed to the spleen by macrophages
|
|
|
cold agglutinin disease is a complication of what diseases?
|
infectious mononucleosis and mycoplasma pneumonia.
it may be a chronic complication of lymphoid neoplasms. |
|
|
what effect does hypoxia have on the production of EPO?
|
production is increased by hypoxia
|
|
|
What is polychromatophilia?
|
increased numbers of larger red cells that stain with a bluish cast. These are premature RBCs and would likely stain as reticulocytes.
|
|
|
what are some causes of aplastic anemia?
|
Toxic exposure
dysfunction of cytotoxic T cells radiation exposure chemicals such as benzene therapeutic drugs such as chloramphenicol, sulfonamides, gold salts, chlorpromazine, antimalarial drugs, and alkylating agents. Viral infection by parvovirus or hepatitis C. |
|
|
Name six causes of folate deficiency anemia.
|
dietary deprivation in alcoholics or dieters.
Pregnancy phenytoin or oral contraceptive therapy folate acid antagonist chemotherapy relative deficiency in hemolytic anemia intestinal malfunction due to sprue or Giardia |
|
|
How do you distinguish folate deficiency from vitamin B12 deficiency?
|
There are no neurologic abnormalities in folate deficiency.
|
|
|
Name eight causes of vitamin B12 deficiency megaloblastic anemia.
|
pernicious anemia, total gastric resection, disorders of the distal Ilium, a strict vegetarian diet, intestinal malabsorption syndromes, blind loop syndrome, broad-spectrum antibiotic therapy, Diphyllobothrium latum infestation (fish tapeworm)
|
|
|
What are the three peripheral blood findings in macrocytic anemias? What is seen in the bone marrow?
|
pancytopenia, global macrocytosis, hypersegmented neutrophils.
the bone marrow shows megaloblastic hyperplasia. |
|
|
How do you distinguish iron deficiency anemia from beta thalassemia minor?
|
In beta thalassemia minor, the alpha-2 hemoglobin is increased.
|
|
|
What groups are at risk for dietary deficiency of iron?
|
Premature infants: human milk is low in iron, and newborn iron is depleted within six months. Pregnant women may also require iron supplements.
The elderly are also at risk of dietary deficiency. |
|
|
What are the differences between sporadic and endemic Burkitt's?
|
Sporadic: in US, mostly in Peyer's patches, rarely have EBV; endemic = Africa, in jaw + abdomen, most have EBV
|
|
|
what are some causes of haemolytic anaemia?
|
hereditary spherocytosis, G-6-PDH deficiency, sickle cell anaemia, thalassaemia, immune disorders
|
|
|
what are the clinical features of haemolysis?
|
scleral jaundice, splenomegaly, increased reticulocytes, elevated LDH, asbence of serum haptoglobin, haemosiderin in urine
|
|
|
What are the malignant cells in NHL?
|
T or B cells that were screwed up at a certain developmental point so they recapitulate morph + immunology of some cell precursor (from lymph node stage)
|
|
|
What is smoldering myeloma?
|
A more indolent form when findings are not sufficient for outright PCM diagnosis. Pt often asymptomatic, may be stable for years
|
|
|
What does a PCM cell look like? How does the bone marrow look?
|
Cell: varying degrees of atypia; maybe multinucleated, or anaplastic. BM: may be patchy; see nodules or infiltrate of pc, trabeculae look thin + sparse
|
|
|
How do plasma cell myelomas lead to bone lesions?
|
PCM cells secrete osteoclast activating factor, which includes several substances like TNF-B + IL-1.
|
|
|
What are typical findings for a patient w/ plasma cell myeloma?
|
moderate to severe normochromic normocytic anemia; maybe neutro + thrombocytopenia; monoclonal protein in serum +/or urine; Bence Jones, inc calcium, renal abnormalities
|
|
|
What is the most common type of chronic lymphoid leukemia?
|
B - CLL
|
|
|
+ NSE in cells indicates which disease?
|
Chronic myelomonocytic leukemia; a CMPD (monocytes) + MDS (other cells lines) Must have >1000 monos
|
|
|
how does B12 deficiency result in neurological deficits?
|
fatty deposits accumulate in the myelin and predisposing to myeline breakdown and APs are slowed
|
|
|
What indicates AML?
|
Auer rods; MPO +; cells having antigen for CD13, 34, HLA-DR
|
|
|
hypersegmented neutrophils are a feature of which type of anaemia?
|
amegaloblastic anaemia
|
|
|
which deficiencies result in megaloblastosis?
|
vitamin B12 and folate
|
|
|
SLL is the nodal based disease comparative to ________
|
B-CLL (SLL = small lymphocytic lymphoma) cells =small, mature, express CD19, 20, light chain
|
|
|
What are some typical findings in a patient with plasma cell myeloma?
|
High lymphs; RBC rouleaux in smear; high protein, low albumin levels (suggest abnormal protein); hypercalcemia; SPEP = monoclonal spike; odd Ig levels; hypercellular marrow w/ lots of plasma cells
|
|
|
What antigens are expressed by cells in nodular sclerosing Hodgkin lymphoma?
|
CD15, CD30, no CD45, no CD20
|
|
|
What are physical findings with nodular sclerosing Hodgkin lymphoma?
|
effaced lymph node with lots of fibrosis and slightly nodular appearance; RSC surrounded by mileau (lymph, plasma, eos)
|
|
|
What is typical bone marrow appearance for a patient with PV?
|
Excess of RBC precurors and megakaryocytes; lack of iron stores,
|
|
|
All CMPD have an excess of what cell type in the bone marrow?
|
Megakaryocytes, which produce growth factors for fibros -> fibrosis
|
|
|
What are the blast %s that differentiate the phases of CML?
|
<5 = chronic; 5-19 = accelerated; >20 = blast
|
|
|
t/f... commitment to a cell lineage is reversible
|
false, this process is irreversible
|
|
|
What disease is characterized by absolute basophilia?
|
CML
|
|
|
where does haemopoiesis take place in the foetus?
|
in the liver and spleen up to 7 months gestation and in the bone marrow after that
|
|
|
How do you treat hyperviscosity?
|
plasmapheresis
|
|
|
Clinical features of waldenstrom?
|
hyperviscosity related, fatigue, lymphadenopathy
|
|
|
Pathophys of waldenstrom macroglob?
|
malignant lymphoma w/small lymphocytes that excrete IgM
|
|
|
what are the last cells of the erythroid line that can synthesise haemoglobin?
|
reticulocytes
|
|
|
what are the last cells capable of division in the erythroid line?
|
polychromatophilic erythroblasts
|
|
|
what deficiency is the result of chronic blood loss?
|
iron
|
|
|
Physical findings in multiple myeloma?
|
pain, fatigue (anemia and renal failure), infxn, mental status changes, hyperviscosity
|
|
|
how is increased production of RBCs by the marrow achieved?
|
expansion of the volume of red marrow and by shortening of transit time for red cell maturation
|
|
|
Major criteria for dx of multiple myeloma?
|
BM plasmacytosis >30%, M-spike, Bence-Jones, plasmacytoma
|
|
|
What is a Bence-Jones protein?
|
kappa or lambda light chains in urine found in multiple myeloma
|
|
|
What are the two main clinical features of acute lymphoblastic leukemia (ALL)?
|
1. bone marrow failure
2. organ infiltration |
|
|
What does bone marrow failure result in?
|
1. anemia: pallor, lethargy
2. neutropenia: fever, malaise, infections 3. thrombocytopenia: bruises, bleeding |
|
|
What does organ filtration result in?
|
tender bones
lymphadenopathy hepato/splenomegaly meningeal syndrome (headache, nausea, blurred vision) |
|
|
What are clinical features of acute myeloid leukemia (AML)?
|
similar to ALL
mostly anemia, thrombocytopenia |
|
|
What is characteristic of M3 variant of AML?
|
disseminated intravascular coagulation (DIC)
|
|
|
What is characteristic of the M4/M5 variants of AML?
|
gum hypertrophy
skin involvement CNS disease |
|
|
What are clinical features of chronic myeloid leukemia (CML)?
|
1. hypermetabolism
2. splenomegaly 3. anemia 4. abnormal platelet function 5. gout/renal impairement |
|
|
How does hypermetabolism present?
|
weight loss, lassitude, anorexia, night sweats
|
|
|
How can anemia present?
|
pallor, dyspnea, tachycardia
|
|
|
How can abnormal platelet function present?
|
bruising, epistaxis, menorrhagia, hemorrhage
|
|
|
Why would gout or renal impairement be a feature of CML?
|
excessive purine breakdown causing hyperuricemia
|
|
|
What are symptoms of myelodysplasia?
|
anemia
infections easy bruising/bleeding |
|
|
What are some clinical features of chronic lymphocytic leukemia (CLL)?
|
1. symmetric enlargement of cervical, axillary or inguinal nodes
2. anemia (thrombocytopenia) 3. splenomegaly (later stages) 4. immunosuppression |
|
|
What are some clinical features of Hodgkin's lymphoma?
|
1. painless, asymmetrical, firm superficial lymph nodes
2. splenomegaly (50%) 3. mediastinal enlargement 4. constitutional symptoms |
|
|
What are constitutional symptoms?
|
fever
pruritis (itching) weight loss weakness fatigue anorexia |
|
|
What are some clinical features of non-Hodgkin's lymphoma?
|
1. superficial (asymmetrical) lymphadenopathy
2. constitutional symptoms 3. oropharyngeal involvement 4. anemia 5. hepato/splenomegaly 6. other organ involvement |
|
|
A patient presents with asymmetric matted lymph nodes. Is it more likely to be leukemia or lymphoma?
|
Lymphoma
|
|
|
A patient presents with asymmetric lymph nodes, constitutional symptoms, splenomegaly and a sore throat. Is it more likely Hodgkin's or non-Hodkin's?
|
non-Hodgkin's sometimes presents with oropharyngeal symptoms
|
|
|
You have determined that there is bone marrow failure (anemia, neutropenia, thrombocytopenia) and organ infiltration (sore bones) in a 4 year old girl. What is the most likely diagnosis?
|
ALL
|
|
|
A 60 year old patient presents with sudden severe anemia, thrombocytopenia and enlarged bleeding gums. What is the most likely diagnosis?
|
AML
|
|
|
In which hematologic malignancy is hypermetabolism a major feature?
|
CML
|

