![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
What is made in the glomerulosa
|
Aldosterone
|
|
|
What is made in the fasciulata/reticularis
|
Cortisol and androgens
|
|
|
What does the left adrenal vein empty into?
|
Left renal vein (can lead to thrombosis and hemorrhage)
|
|
|
What does the right adrenal vein empty into?
|
Posterior aspect of the vena cava (can lead to thrombosis and hemorrhage)
|
|
|
CRH is from where and stimulates what?
|
Hypothalamus; stimulates ACTH in a pulsatile manner; has a diurnal rhythm (peak before awakening)
|
|
|
What is the main negative feedback for ACTH?
|
Cortisol (both long and short feedback)
|
|
|
What is the precursor molecule for ACTH
|
pro-opiomelancortin (POMC)
|
|
|
StAR protein
|
Steroidogenic acute regulator protein-->shuttles cholesterol from the outer to the inner mitochondrial membrane
|
|
|
P450scc
|
Cholesterol--side chain cleavage-->Pregnenolone
|
|
|
P450c17
|
Progesterone--->17-hydroxyprogesterone
|
|
|
P450c21 and P450c11
|
two hydroxylations from 17-hydroxyprogesterone--->active cortisol
|
|
|
Progesterone-->deoxycorticosterone
|
P450c21
|
|
|
Pregneolone--->androgen
|
P450c17
|
|
|
What is cortisol bound to
|
mostly corticosteroid-binding globulin
also albumin |
|
|
11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2)
rxn and location? |
Cortisol is metabolized to biologically inert steroid cortisone by the enzyme
In the Kidney It protects cortisol from binding to the same receptor as aldosterone |
|
|
What is the rate limiting step in cortisol production and secretion?
|
StAR protein-cholesterol entering the mitochondria
|
|
|
17a Hydroxylase (P450c17)
If there is a deficiency in the enzyme what are the effects? |
can hydroxylate either pregneolone or progesterone
Increased mineralocorticoids Decreased cortisol and sex hormones HTN, hypokalemia |
|
|
21 Hydroxylase (P450c21)
If there is a deficiency in the enzyme what are the effects? |
Hydroxylates Progesterone to 11-deoxycorticosterone or 17-hydroxyprogesterone to 11-deoxycortisol
decreases mineralcorticoids and cortisol Increases Sex hormones Hypotension, hyperkalemia, incr. renin, masculinization |
|
|
11B Hydroxylase (P450c11)
If there is a deficiency in the enzyme what are the effects? |
11-deoxycorticosterone to corticosterone or 11-deoxycortisol to cortisol
Decrease aldosterone but an increase in 11-deoxycorticosterone; increase in sex hormones Hypertension (d/t 11-deoxycorticosterone) |
|
|
Why is 11B-HSD2 enzyme important?
|
It is 100x more effective than aldosterone and therefore would lead to HTN and hyperkalemia if there wasnt 11B-HSD2
|
|
|
What are the effects of cortisol
|
Immune and inflammation
Gluconeogenesis (also increases insulin resistance) Appetite Depression, anxiety Growth and Reproduction Cardiovascular Tone (amplification of adernergic effects) |
|
|
What are the lab values in primary adrenal insufficiency
|
High ACTH
High Renin Low Aldosterone Low Cortisol HYPONATREMIA!! |
|
|
What is low in secondary adrenal insufficiency?
|
ACTH
Hyponatremia |
|
|
What are the sx of adrenal insufficiency?
|
Fatigue, malaise, lack of energy
GI: nausea, vomiting, anorexia, weight loss Hyponatremia, hyperkalemia (primary) Lymphocytosis |
|
|
Causes of 2ndary Adrenal insufficiency
|
(Withdrawal from) exogenous corticosteroid therapy
Pituitary/Hypothalamic Disease (Hypophysitis, drug induced (ipilimumab) may cause isolated ACTH deficiency |
|
|
Draw out the tx/dx plan for adrenal insufficiency
Sorry if the pic is small |

after low cortisol is determined...
|
|
|
What constitutes a normal cortisol response to ACTH
|
Peak response at 30 or 60 minutes >18 ug/dL
If it is low you need a ACTC measurement ACTH is ALWAYS elevated in patients with primary adrenal insufficiency |
|
|
In critically sick patients, why is the serum cortisol possibly not reliable?
|
May have low binding proteins (need to measure the free cortisol in the saliva)
|
|
|
What is the effect of estrogen on cortisol levels?
|
will have a significant increase in total cortisol levels that reflect an increase in CBG rather than any alteration of adrenal function.
|
|
|
What is a sensitive measurement of adrenal reserve?
|
Adrenal androgen production (DHEAS); rare to see a normal level in any type of adrenal insufficiency
|
|
|
Causes of PRIMARY adrenal infufficiency
|
Autoimmune polyglandular syndromes
Metastatic tumor or primary adrenal lymphoma Adrenal Hemorrhage (bilateral)-b/l adrenal vein thrombosis Tb, fungi, HIV Drugs: Ketoconazole, Metyrapone, mitotane, Etomidate Congenital adrenal hyperplasia, familial glucocorticoid deficiency, adrenoleukodystrophy |
|
|
Tx of primary adrenal insufficiency
|
Hydrocortisone (10-15 mg in AM and 5-10 mg in the afternoon) (need additional steroids if you are getting sick)
Monitor overall health; ACTH should remain elevated even with adequate hydrocortisone Solu-cortef-emergency injectable hydrocortisone Give Fludrocortisone daily (monitor electrolyte composition, and plasma renin activity) |
|
|
Treatment for Secondary Adrenal Insufficiency
|
Hydrocortisone in daily divided doses; lower doses needed compared to primary adrenal insufficiency
You DONT need mineralocorticoid replacement since renin-angiotensin and zona glomerulosa remain intact) |
|
|
Effects of Cushing's syndrome
|
Weight gain, facial fullness, Incr. supraclavicular fat, diabetes, osteoporosis, increase BP, myopathy, neuropsych disorders, edema, hypogonadism, androgen excess; Easy bruising
|
|
|
High Cortisol: ACTH dependent
|
Cushing's disease
or ectopic ACTH secreting tumor |
|
|
High Cortisol: Adrenal Dependent
|
Solitary adrenal adenoma
Exogenous glucocorticoid therapy Nodular adrenal hyperplasia |
|
|
Physiological hypercortisolism is d/t
|
Stress, alcohol, neuropsych disorders, starvation
|
|
|
What are the diagnostic tests for cushing syndrome
|
Late-night salivary cortisol (very sensitive/specific)
Overnight low dose dexamethasone suppression test (normally cortisol <1.8 in the morning) 24hr urine test: not typically used |
|
|
Write out the flow chart for diagnosing cushings syndrome
|
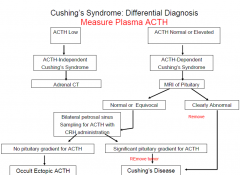
|
|
|
Treatment of Cushings syndrome
|
Surgery Always first! (remove the offending tumor)
Bilateral adrenalectomy in patients that have failed other tx (concern for Nelson's syndrome-regrowth of pit tumor) Radiotherapy Pasireotide-->somatostatin analog (where surgery isnt an option) Metyrapone-->11beta hydroxylase inhibitor Mifepristone-->inhibitor of glucocorticoid and progesterone receptor |
|
|
Pasireotide mech and tx
|
Somatostatin analog
Tx cushing's disease in patients where surgery isnt an option |
|
|
Metyrapone mech of action
|
11-beta hydroxylase inhibitor (stops the cortisol synthesis)
used in adrenal cancer since it is lytic in high doses |
|
|
Mifepristone mech
|
potent inhibitor of glucocorticoid and progesterone receptor
|
|
|
Write out the renin-angiotensin-aldosterone system pathway
|
Angiotensinogen--Renin-->Ag I---ACE---->Ag II (neg feedback on renin)--->constricts smooth muscle and releases aldosterone-->renal water and sodium retention
|
|
|
What channel does aldosterone work on?
|
ENaC channels
|
|
|
Effects of primary hyperaldosteronism
|
Adrenal adenoma-->increased aldosterone-->negative feedback shuts renin down
increased aldo leads to HYPOkalemia and increased blood pressure |
|
|
What is the first test to check for primay hyperaldosteronism?
|
Plasma aldosterone/Plasma renin ratioq
|
|
|
Causes of primary hyperaldosteronism
|
Aldosterone-secreting adrenocortical adenoma
Bilateral hyperplasia of zona glomerulosa |
|
|
Causes of 2ndary hyperaldosteronism aka high Renin
|
Renal ischemia
Decreased intravascular volume CHF Chronic diuretic or laxative use Hypoproteinemic states Chronic Renal failure Sodium wasting disorders |
|
|
Testing for presumed primary hyperaldosteronism
|
CT or MRI of adrenals-->if unilateral--> adenalectomy
If bilateral or normal-->selective venous cath-->medical management or unilateral adrenalectomy |
|
|
Medical management of hyperaldosteronism
|
Spironolactone
Eplerenone Both mineralocorticoid receptor antagonists Decrease sodium and water retention |
|
|
Apparent mineralocorticoid excess
|
11BHSD2 deficiency
|
|
|
Liddle's syndrome
|
mutations in the amiloride sensitive epithelial sodium channel. treated with amiloride and triamterene (potassium sparing diuretics)
|
|
|
Tumors of the chromaffin cells of the adrenal medulla
|
Pheochromocytoma
|
|
|
Paragangliomas
|
tumors that arise from extra-adrenal ganglia of the sympathetic nervous system
|
|
|
What to pheochromocytomas can secrete what?
|
both epinephrine and norepinephrine (primarily norepi)
|
|
|
What are some of the manifestations of catecholamine excess?
|
tachycardia, increased contractility, arrhythmias, HTN, decreased plasma volume (dehydrated); intestinal relaxation, suppression of insulin release (B cells), increased glucose, urinary retention, weight loss
Chest pain, dizziness, circulatory collapase |
|
|
Tests for epi and norepi levels?
|
24 hr urinary test for Catecholamines (Norepi and Epi)
Plasma levels of FREE METANPHRINES (metabolites of epi and norepi; Most sensitive) |
|
|
What is the treatment for Pheochromocytoma
|
Begin alpha-blockade (phenoxybenzamine)
Next, you can add B-blockers Hydrate Surgical therapy with adrenalectomy |
|
|
What type of cell is in the medulla?
|
Chromaffin cells (epinephrine)
|
|
|
What are the three layers of the adrenal cortex and what is in each layer?
|
- Zona glomerulosa (G): Mineralocorticoids (aldosterone) = “Salt”
- Zona fasciculata (F): Glucocorticoids (cortisol) = “Sugar” - Zona reticularis (R): Sex steroids (estrogens and androgens) = “Sex” |
|
|
Bilateral thickening of the adrenal cortex
|
Adrenocortical hyperplasia
|
|
|
What type of cells predominate in adrenocortical hyperplasia?
|
Predominantly fasciculata cells; Clear cells
|
|
|
Characteristics of Adrenocortical adenoma?
|
Encapsulated
1-2 cm Usually Non-functional Predominantly zona fasciculata cells (like hyperplasia) |
|
|
Characteristics of Adrenocortical Carcinoma
|
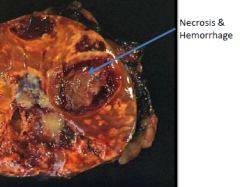
Rare
>200-300 grams; 5 cm in diameter Invasive Necrosis/hemorrhage invade adrenal vein and vena cava If poorly differentiated it will have more color in cytoplasm, large nuclei, and a lot of irregularity |
|
|
exogenous glucocorticoids leads to what change in the adrenal gland?
|
Cortical atrophy
|
|
|
Increased ACTH leads to what change in the adrenal gland?
|
Bilateral hyperplasia
|
|
|
ACTH independent hypercortisol leads to what change in the adrenal gland?
|
Adrenocortical adenoma or carcinoma
|
|
|
Hyperaldosteronism leads to what change in the adrenal gland?
|
Adrenal cortical adenoma (Conn Syndrome)
|
|
|
What is the indicator for malignancy for pheochromocytoma?
|
METASTASIS
|
|
|
What is the microscopic appearance of pheochromocytoma?
|
Zellballen: nests of cells within a rich vascular network; abundant cytoplasm that is granular (basophilic)
Stain with neuroendocrine markers (chromogranin, synaptophysin) |
|

|
Adrenal Pheochromocytoma
|
|
|
Extra adrenal pheochromocytoma
|
Paraganglioma
Common sites-->jugulotypanic, carotid body, vagal, aorticopulmonary |
|
|
What is the most common finding associated with endogenous Cushings
|
Bilateral hyperplasia
|
|
|
What is the pheochromocytoma rule of 10?
|
Pheochromocytoma 'rule of 10': 10% bilateral, 10% malignant (higher in familial cases), 10% extra-adrenal, 10% familial
|

