![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
Classical pathway [LO]
|
![[LO]](https://images.cram.com/images/upload-flashcards/56/20/01/2562001_m.jpg)
[LO]
|
|
|
Lectin pathway [LO]
|
![[LO]](https://images.cram.com/images/upload-flashcards/56/20/04/2562004_m.jpg)
[LO]
|
|
|
alternate complement pathway [LO]
|
![[LO]](https://images.cram.com/images/upload-flashcards/56/20/07/2562007_m.jpg)
[LO]
|
|
|
Role of constituent proteins [LO]
|
![[LO]](https://images.cram.com/images/upload-flashcards/56/54/45/2565445_m.jpg)
[LO]
|
|
|
role of the complement system in protecting from and causing disease. [LO]
|
[LO]
|
|
|
what is the role of the C3ac5a split product?
|
Aggregation of platelets.
Chemotactic for leukocytes (C5a >>>> C3a). Acts on mast cells --> histamine --> vasodilation --> ↑↑ vascular permeability. |
|
|
What is the role of the split product C3a & C5a
|
Are rapidly degraded by serum carboxypeptidase
|
|
|
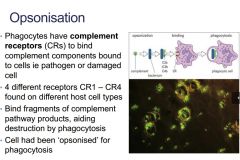
What is the role of the split product C3b
|
Opsonisation (process whereby opsonins make an invading microorganism more susceptible to phagocytosis).
Bystander lysis. |
|
|
What is the role of the split product C5b
|
Opsonisation (process whereby opsonins make an invading microorganism more susceptible to phagocytosis).
Bystander lysis. |
|
|
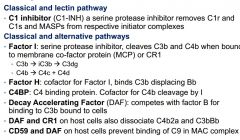
What is the role of the split product C1 INH
|
Removes C1r and C1s from C1q
Binds to C1rC1s blocking activity |
|
|
What is the role of the split product Factor 1
|
Cleaves C3b, C4b into inactive forms
|
|
|
What is the role of the split product Factor H
|
Inhibits C3bB formation
Disrupts C3bBb complexes Acts with Factor I – ↑ decay of C3b --> C3c + C3d |
|
|
What is the role of the regulatory protein CR1
|
Binds C4b, displacing C2b.
Binds C3b, displacing Bb. Cofactor for Factor I (FI; which regulates complement activation by cleaving cell-bound or fluid phase C3b and C4b. |
|
|
What is the role of the regulatory protein DAF
|
Same function as CR1 except it doesn’t at as a cofactor for Factor I.
|
|
|
What is the role of the regulatory protein MCP
|
Increases inactivation of C3b and C4b.
|
|
|
What is the role of the regulatory protein Vitronectin (S protein)
|
Prevents C5b, C6 and C7 binding to membrane.
|
|
|
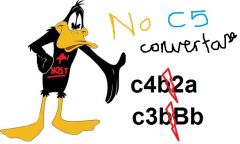
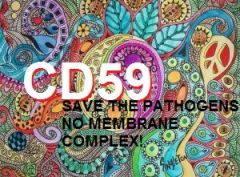
What is the role of the regulatory protein CD59?
|
Prevents C5b – C7 formation on homologous cells
|
|
|
What is the role of the regulatory protein (Thermal instability)?
|
Very short half life (T1/2).
|
|
|
What are the AgAb complexes in the Classical pathway?
|

C1q, C1r, C1s, C4, C2
|
|
|
What are the mannose binding lectin or ficolin binds carbohydrates on pathogen surfaces?
|

MBL, MASP-2, C4, C2
|
|
|
What are the proteins on the pathogen surfaces of the alternative pathway?
|

C3, B factor, D factor
|
|
|
What does C3a do?
|

peptide mediator of:
1. inflammation 2. phagocyte recruitment |
|
|
What is the function of C3b
|

1. Binds to complement receptors of phagocytes
2. Opsonisation of pathogens 3. Removal of immune complexes |
|
|
What are the Terminal Complement components?
|

C5b, C6, C7, C8, C9
|
|
|
Where does C1q bind?
|
Multiple Fc regions
|
|
|
Which Abs does C1q bind?
|
IgM, IgG1, IgG3
|
|
|
Where does complement reside?
|
It is confined to the surface on which it is initiated.
|
|
|
Describe what C1-INH does
|

|
|
|
Describe the actions of the C1 inhibitor
|

|
|
|
What removes C1r and C1s
|

|
|
|
What can remove MASPs?
|

|
|
|
What does the Factor I do?
|

|
|
|
What does Factor I have to be bound to be a regulator?
|
CR1 or the Membrane cofactor protein
|
|
|
What breaks c3b down to ic3b and C3dg?
|
Factor I
|
|
|
What does FI do to both C3b and C4b?
|
C3b --> ic3b and c3dg
C4b --> c4c, c4d |
|
|
What are the serine protease inhibitors in the complement system
|
C1-INH and Factor I
|
|
|
What displaces Bb in the alternate complement pathway?
|

Factor H
|
|
|
What is C4BP?
|

cofactor for factor I, cleaves c4b to C4d, C4c
|
|
|
function of DAF
|

Competes with B for C3b
Splits up C4b2a and c3bBb with CR1 And prevents MAC with CD59 |
|
|
Where does DAf reside? What does it to in conjunction with what?
|
on host cells also dissociate C4b2a and C3bBb in conjunction with CR1
|
|
|
What prohibits the MaC from forming?
|
CD59 and DAF on host cells prevent binding of C9 in MAC complex
|
|
|
What does CD59 do?
|
|
|
|
What are the classical pathway deficiencies?
|
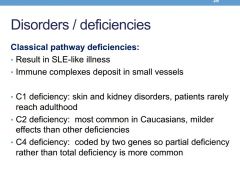
C1 deficiency
C2 deficiency C4 definciency |
|
|
What are the symptoms and prognostics of C1 deficiency?
|
skin and kidney disorders- pts rarely reach adulthood
|
|
|
What is the most common classical pathway deficiency?
|
C2 deficiency, has milder effects
|
|
|
What is C4 deficiency
|
coded in 2 genes
partial deficiency more common |
|
|
What are deficiencies associated with alternate and lectin pathways?
|

|
|
|
What happens if deficient in C1-INH
|
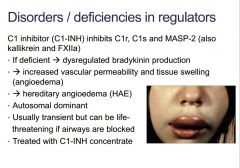
desregulated bradykinin production (Bradykinin is a peptide that causes blood vessels to dilate (enlarge))
|
|
|
What causes dysreagulation of bradykinin
|
C1-INH deficiency
|
|
|
What causes C1-INH deficiency
|
autosomal dominant hereditary angioedema
|
|
|
What is the good news about hereditary angioedema?
|
transient - however life threatening if airways blocked
|
|
|
How is hereditary angioedema treated?
|
C1-INH concentrate doses
|
|
|
What occurs if a factor H mutation exists
|
Impaired C3 convertase -->
atypical haemolytic uraemic sydrome endothelial damage --> fibrin depostion Haemolytic anaemia thrombocytopenia renal failure |
|
|
Which deficiency causes the following and why?
atypical haemolytic uraemic sydrome endothelial damage --> fibrin depostion Haemolytic anaemia thrombocytopenia renal failure |
Impaired C3 convertase by factor H deficiency - Factor H inhibits Bb and therefore cannot convert to c3a, c3b (positive feedback)
|
|
|
What deficiency causes PNH and complement mediated red cell lysis
|
CD59 and DAF
|
|
|
What does CD59 and DAF deficiencies cause
|
CD59 - prevent membrane complexes
DAF - usurps Bb for binding with c3b, membrane complexes and prevents c5 convertase when with - splits c3bBb, c4b2a Causes paroxymal nocturnal haemoglobinuria and complement mediated red cell lysis |
|
|
When is classical pathway used?
|
Ag Ab complexes
|
|
|
When is lectin pathway used?
|
microbes with terminal manose groups or acetylated sugars
|
|
|
When is alternative pathway used?
|
bacteria, fungi virus or tumour cells.
|
|
|
What deficiencies cause lupus like disease?
|
C1, C2, C4
|
|
|
What deficiencies cause severe recurrent bacterial infections?
|
C3
fH fI B D |
|
|
What deficiencies cause neisserial infection?
|
Factor P
|
|
|
What causes RECURRENT Neisserial infection?
|
c6, c7, c8, c9
|
|
|
What is complement testing performed on?
|
fresh serum
|
|
|
Describe classical pathway screen
|
|
|
|
Describe Alternative pathway screen
|
|
|
|
Describe Opsonisation
|
|
|
|
Describe the agents responsible for chemotaxis and inflammation
|
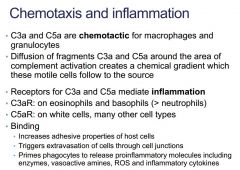
C3a and C5a:
‘anaphylatoxins’ |
|
|
What is the c3aR located on?
|
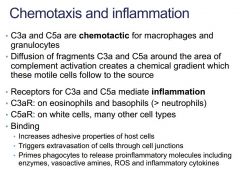
esinophils, basophils more than neutrophils
|
|
|
Where is the c5aR found?
|
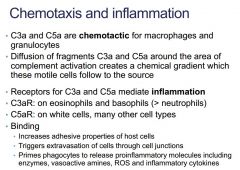
white cells
|
|
|
What does the binding of c3aR or c5aR do?
|
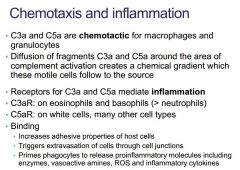
++ adhesive properties of host cells
+++ extravasion primes phagocytes to excrete enzymes, vasoactive amines and inflammatory cytokines • swelling, heat and pain • fever and shock • C3a and C5a: ‘anaphylatoxins’ |
|
|
What does C3b perform?
|
from classical pathway coats and opsonises the aggregated complex
|
|
|
What is the role of CR1 and where is it located?
|
CR1 on red cells binds C3b (and C4b) to carry the complex to sites of macrophage residency
|
|
|
What primes B cells?
|
Binding of antigen bound to C3 fragments enhances antigen specific B cell selection and maturation
Ag bound to BCR, C3 fragment (C3d) bound to CR2 |

