![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
What is a thrombus? |
A pathological blood clot which forms in a blood vessel |
|
|
What is an embolus? |
Clot that breaks off and travels through the ciruclation until obstructed by vessels of smaller diameter |
|
|
What are venous thrombi? |
Red clots = RBCs in a fibrin mesh |
|
|
What are arterial thrombi? |
White clots = platelets and fibrin |
|
|
What is a DVT and how is it classified? |
Deep vein thrombosis, location relative to the calf veins.
Distal = cofnined to the calf veins Proximal = involve the popliteal vein or above |
|
|
What is a PE? |
A pulmonary embolism |
|
|
What is Virchow's triad |
Stasis Vessel wall disorder Hypercoagulability. |
|
|
What are alternative causes of emobilsm (other than red and white clots) |
Air, amniotic fluid, fat. |
|
|
Where can venous thrombi lodge? |
Axillary vein, cerebral vein, mesenteric vein, portal vein. |
|
|
What are the relative frequencies of heritable and acquired and idiopathic causes of VTE? |
Heritable = 25%
Acquired = 50%
Idiopathic = 40%
many patient have heritable risk plus acquired. |
|
|
What is the cross over between DVT and PE? |
same patholigical process 40% of patients with DVT are asymptomatic for PE but evidence on lung scan. Majority of PE rise from DVT. |
|
|
Where do the majority of DVT's originate from? |
Calf venous sinuses.
25% extend proximally to the popliteal vein or above. 40% of those embolise 20% of those (2% of total) are fatal.
|
|
|
What is the incidence of VTE? |
1 in 1000 per year.
PE = the 3rd most common cause of CV death. Untreated mortality is 30% reduced to <5% with treatment.
slightly more commen in men and incidence strongly increases with age.
Most common cause of preventable postoperative death and maternal mortality.
|
|
|
What are the risk factors for VTE? STRONG |
STRONG: fracture of the hip or pelvis hip or knee replacement surgery major general surgery especially for malignancy. major trauma spinal cord injury hospitalisation with acute medial illness. |
|
|
What are MODERATE risk factors for VTE? |
Previous VTE Cancer (outpatient) CCF or resp failure Pregnancy COCP HRT Thrombophilia
|
|
|
What are WEAK risk factors for VTE? |
Age increasing Bed rest > 3 days Travel-related thrombosis Obesity Day-case surgery Varicose veins
|
|
|
How does DVT present? |
UNILATERAL Pain Erythema Swelling Tenderness Palpable cord Warmth Ipsilateral oedema
|
|
|
Why is objective diagnosis of VTE so important? |
Because 75% of patients with suspected VTE are negative on investigation
Drugs used to treat VTE cause serious/fatal side effects. |
|
|
What are potential DDX for VTE? |
Musculo-tendinous trauma, tendinitis RUptured baker's cyst. Superficial thromboplebitis Cellullitis Compression of iliac veins Congestive HF Post thrombotic syndrome. |
|
|
How can VTE be confirmed? |
1) Clincial pre-test probabiltity = wells score 2) D-dimer = non-specific marker of inflammation 3) radiological assessment: compression ultrasound as non-invasive; sometime venography (gold standard) e.g. if looking for calf DVT
(also may do a CT/MRI scan) |
|
|
What characteristics are scored in the pre-test probability system and what does the total score values indicate? |
Total score >= 2 means DVT is likely score total <= 1 means DVT is unlikely.
All rank + 1: Active cancer within the last 6 months Paralysis, paresis Recentely bedridden for >= 3 days, major surgery in <12 weeks. Localised tenderness along the distribution of the deep veins Entire leg swelling Pitting oedema on the symptomatic leg
Alternative Dx at least as likely = -2. |
|
|
Describe the outpatient diagnosis pathway for DVT starting with a pt presenting with DVT symptoms/signs. |
1 ) Low pre-test probability a. D dimer neg - no DVT post - b. ultrasonography - neg no DVT, post: DVT
2) High pre-test probability a. ultrasonography pos = DVT, neg - D-dimer => post = repeat ultrasonography in 1 week, neg = no DVT |
|
|
What are the key complications of DVT? |
PE extension of the clot Recurrent VTE episodes Post-thromobptic syndrome = recurrent pain and swelling in the leg that may progress to local skin pigmentation and ulceration due to venous hypertension (obstruction and valve damage)
presents to some degree in in 30-50% of patients with proximal DVT. |
|
|
What are the key modes of presentation of PE? |
Pulmonary infarct/haemorrhage with breathlessness and pleuritic chest pain occurs in 65%
Isolated breathlessness in 25%
Collapse, syncope, hypertension and shock in 10%
|
|
|
What are the key signs of PE? |
Tachpnoea and tachycardia crepitations and pleural rub clinical signs of DVT uncommon. |
|
|
What abnormalties might the following diagnositic tests reveal in the case of a pleural effusion? |
ECG: sinus tachycardia, R heart strain, T wave inversion. CXR often normal but may show small pleural effusion and wedge shaped density above the diaphragm. ABG: hypoxia and low CO2 often normal. |
|
|
What are potnetial DDX for PE? |
Pneuomonia or bronchiti COPD exacerbation Asthma ACS Anxiety Pneumothorax Lung cancer |
|
|
What are the diagnostic tests for PE? |
CTPA Isotope lung scan (V/Q scan)
Echocardiogram
Pulmonary angiogram.
Leg ultrasound
D-dimer |
|
|
How is the Wells score used for PE? |
>= 4 means PE likely, <= 4 PE unlikely.
Score 3 DVT signs Alternative diagnosis less likely.
Score 1.5 pulse >100 immobilisation or surgery in previous 4 weeks. previous DVT/PE.
Score 1.0 haemoptysis cancer in last 6 months
|
|
|
Describe the alogorythm for diagnosis of PE: |
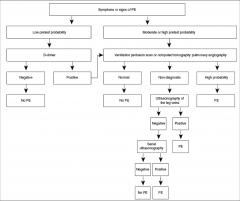
|
|
|
What is the prognosis for PE? |
10% mortality within 1 hr of symptom onset. 30% mortality within 2 weeks if not treated
If treated mortality reduced to <5% 5% of treated pts have persistent breathlessness.
Al-cause mortality at 1 year is 25% |
|
|
What is the core management for VTE? |
Full bloods, clotting screen, D-dimer, U+Es and LFTs. HEPARIN if DVT/PE likely. usually LMWH confirm diagnosis CONTINUE HEPARIN AND STARY WARFARIN stop heparin after minimun of 5 days and when INR is in the therapeutic range (2.0-3.0) for 2 consecutive days.
review again at 3 months.
|
|
|
What are the differnet types of heparin : unfractioned and low molecular weight. |
Unfractioned: IV of subcutaneous immediate sonset short half life: 60-90 mins Monitor by APTT vairable adjusted dose.
LMWH: agent of CHOICE AT LEAST AS EFFECTIVE AND SAFER THAN UFH more predictable subcut injection longer half life = 4 hrs. predominantly anti Xa no monitoring
Fondaprinux: synthetic polysaccharide half life of 18hrs. fixed dose. unsutiable is renail impariments GFR <30mL/min. |
|
|
What are the side effects of use of heparin? |
Major bleeding: 1-5% in the first week of treatmnet. Specfiic heaprin antagonists= protamine. Heparin-induced thrombocytopenia (HIT) = develops 5-14 days after the start of heparin. features are onset of moderate thrombocytopenia and high risk of thrombosis.
osteoporosis- only with prolonged exposure.
Heparin induced skin necrosis in patients with HIT |
|
|
What is warfarin? |
Vitamin K antagonsist = facotrs 11,7,9, 10 protein c and S given orally half-life of 36 hrs delayed onset of action primarily affects the PTT converted to ration (INR) dose adjusted to maintain INR in the range 2.0-3.0. 3.0-4.0 if recurrence whilst adequcuately anticoagulated. tearatogenicity = CI pregnancy. |
|
|
What are the side effects of warfain? |
Warfarin induced skin necrosis.
Major risk of bleeding 1-2% risk per year. fatal 0.2-0.4% per year. management of bleeding: stop warfain, consider a vitamin K 0.5-5mg orally or IV> starts working after 4hrs. |
|
|
What is the acute, intermediate and chronic management outline? |
picture |
|
|
What are new anticoagulants and where do they act?
|
FACTOR Xa IHIBITORS = RIVAROXABAN, APRIXABAN
THROMBIN INHIBITORS: DABIGATRAN ETEXILATE. |
|
|
What is the recurrence risk for VTE? |
Depends on reason for initial event: overall intially 5% risk per year, 30% by 10 years. |
|
|
What other interventions are avaiable? |
Thrombolysis = clot busting therapy. used in massive PE or limb-threatening DVT = 1-3% intracranial bleeding risk.
Inferior vena cava filter. = used if major CI to anticoagulation or if recurrence of PE despite intervention
Graduated elastic compression stockings. - knee length grade 2 stocking reduce incidence of post-thrombotic syndrome. |
|
|
What steps should be taken to investigate for occult cancer due to VTE? |
History, physical exam chest X-ray FBC, calcium and LFTs urinalysis.
if over 40 and 1st unprovoked VTE: consider: CT abdo and pelvis + mammogram. |
|
|
What is thrombophilia? |
Lab detected predisposition to thrombosis
heritable causes: factor V leiden 15% prothrombin G20210A variant protein C deficiency 1-2% protein S deficiency 1-2% Antithrombin deficiency <1%
|
|
|
Antiphospholipid syndrome |
Acquired form of thrombophilia: 1. Primary 2. Secondary to CT disorder eg. SLE 3. Clinical and lab features. |
|
|
What are the clinical indication for APS? |
Thrombosis = arterial or venous Pregnancy morbidity: 1 or more unexplained foetal deaths after 10 week, 1 or more premature deliveries before 34 weeks with pre-eclampsia or placental insufficiency 3 or more miscarriaged before 10 weeks.
|
|
|
What are the lab findings for APS? |
Lupus antigcoagulatn X2 >= 12 weeks apart and/or anticardilipin antibodies X2 >= 12 weeks apart and Anti-B2 glycoprotein 1 antibodies X 12 weeks apart.
|
|
|
What are the clinical manifestations of APS? |
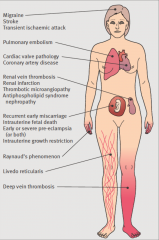
Migraine, stroke, TIA, PE, Cardiac valve pathology, CAD, Renal vein thrombosis, Renal infarction, thrombotic microangiopathy Recurrent early miscarriage. Early or severe pre-eclampsia. Raynaud's phenomenon. Livedo reticularis. DVT
|
|
|
What are some red flags for APS? |
Unexplained DVT or PE in patients under 50. Stroke in pts under 50. TIA in patients under 50 Recurrent thromobosis Thromobosis at unusual site. Unexplained fetal loss after 10 weeks gestation Severe or early pre-eclampsia Severe intrauterine growth restrictioPre-eclampisa Cardiac valve disease.n |

