![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
What are the 4 layers of all regions of the GI tract, from inside to outside?
|
Mucosa - epithelium, basal lamina and muscularis mucosae
Submucosa Muscularis externa - inner circular and outer longitudinal Adventitia/serosa |
|
|
There are two muscular layers, name them and give their main function(s)?
|
Muscularis mucosae (mucosal layer) - local control and adaptation to contents
Muscularis externa (inner circular/outer longitudinal) - peristalsis |
|
|
There are 2 types neuronal control over the GIT. Name them and describe the ways in which they affect gut motility.
Take courage in both hands... |
ANS: PNS (ACh excites gut, VIP and ADP inhibits gut), SNS (NA inhibits gut)
ENS (enteric NS): myenteric/Auerbach's (stim by ACh, inhib by VIP), submucosal/Meissener's (stim by ACh and VIP) |
|
|
What are the 2 plexuses which form the enteric nervous system, their alternative names and their function?
|
Submucosal (Meissner's) - control muscularis mucosae and submucosal vessels
Myenteric (Auerbach's) - between inner circular/outer longitudinal, controls peristalsis |
|
|
Which plexus control peristalsis, and where does it lie?
|
Auerbach's/myenteric plexus, in the muscularis externa, between the inner circular/outer longitudinal.
|
|
|
What cells control the initiation of peristalsis?
|
Interstitial cells of Cajal.
|
|
|
What is the surface epithelium of the oesophagus, how is the muscle arranged along it's length, and what provides lubrication?
|
Stratified squamous epithelium
Skeletal muscle at the top, mixed in the middle, smooth muscle only at the bottom Submucosal gland supply lubrication |
|
|
What change is noted at the gastro-oesophageal junction?
|
Change from stratified squamous to simple columnar epithelium.
|
|
|
What change can you see in the muscularis externa between the oesophagus and stomach?
|
Oesophagus has two layer (inner circular/outer longitudinal)
Stomach has three (inner oblique, middle circular, outer longitudinal) |
|
|
What is a gastric pit, versus a gastric gland?
|
A pit opens into the lumen of the stomach, whilst several glands will open into a single pit
|
|
|
Name the parts of a gastric pit and the glands which open into it?
|
Isthmus at the top (where glands converge), then each gland has a neck and a base
|
|
|
What type of cells might you find in the isthmus?
|
Parietal cells
|
|
|
What type of cells might you find in the neck of a gland?
|
Mucus neck cells, stem cells, parietal cells
|
|
|
What type of cells might you find in the base of a gland?
|
Peptic cells, parietal cells, mucus neck cells, neuroendocrine cells and stem cells
|
|
|
How do pits and glands vary in the pyloris?
|
Deeper pits, coiled glands, nearly all mucus-secreting, gastrin secreting as well
|
|
|
What do parietal cells secrete and how could you identify one under a microscope?
|
HCl-, abundant mitochondria, intracellular canneliculi, extensive microvilli and a tubulovesicular system (with reserves of membrane etc)
|
|
|
Why doesn't the stomach digest itself?
|
Surface epithelial cells secrete HCO3- which forms an alkali layer of mucus over the epithelium. HCl- penetrates this like a viscous finger.
|
|
|
What pH is required for the HCl to penetrate the mucous layer?
|
Must be above pH4.
|
|
|
What are the two distinctive features of the duodenum, and what do they do?
|
Brunner's glands - secrete HCO3- to neutralise stomach acidic contents
Villi - absorption |
|
|
What are the distinctive features of the jejunum and ileum?
|
There are 4:
Plica circulares, villi, microvilli and Peyer's patches. |
|
|
What are lacteals?
|
Lymphatics which run along villi, taking away fats in chylomicrons.
|
|
|
What cells would you expect to find in jejunal or ilial epithelium and what are their function?
|
1. Enterocytes for absorption
2. Goblet cells, secreting mucus 3. Crypts, with stem cells 4. Paneth cells, secreting lysozyme |
|
|
What are Peyer's patches?
|
Aggregates of lymphoid tissues, 10-200 nodules in the ileum. Contain M cells for phagocytosis in lumen.
|
|
|
How could you distinguish the colon, and what is it's primary function?
|
No villi, a thick outer muscular layer - tenai coli, Peyer's patches, crypts, microvilli, and function is water recovery
|
|
|
What type of glands do you find in the colon, and what type of epithelial cells?
|
Tubular glands. 2 types of cells - enterocytes with microvilli for absorption and goblet cells secreting mucus
|
|
|
What change occurs at the anorectal junction?
|
Abrupt change from simple columnar to stratified squamous epithelium.
|
|
|
What glands would you find around the anal orifice?
|
Apocrine sweat glands, releasing scent.
|
|
|
PNS stimulation is via which nerve to the sub-lingual and sub-mandibular glands?
|
Chorda tympani (VII)
|
|
|
SNS secretion acts on what receptors in salivary secretion?
|
NA stimulation of B-adrenergic receptors causes a vasoconstriction, then a vasodilation to cause a viscous secretion (protein rich)
|
|
|
Explain primary saliva secretion and how this is modified in the ducts.
|
Flow increases 5-10x fold, the result is a rich isotonic solution secreted by acinar cells, this collects in the lumen. Na+ and Cl- reabsorbed, K+ and HCO3- secreted, result is a hypotonic saliva.
|
|
|
What concentrations would you expect to see in hypotonic saliva?
|
Less concentrations of Na+ and Cl-, and higher in K+ and HCO3-
|
|
|
What are the four phases of gastric acid secretion?
|
Basal - Circadian rhythm, going up a meal times, low in AM, higher in evening
Cephalic - Sight, smell, taste of food stimulated secretion Gastric - Distention of gut stimulates further secretion Intestinal - Amino acids and peptides in duodenum cause further secretions |
|
|
List the secretory cell types in the stomach and what they secrete.
|
Neck cells - mucus secreting, protein rich
Parietal cells - HCl and intrinsic factor (for B12) Chief cells - Pepsinogen (becomes pepsin, protein digestion) Endocrine G cells - Gastrin, stimulates HCl secretion Endocrine D cells - Somatostatin, inhibits gastrin release |
|
|
What are the direct and indirect mechanisms stimulating secretion of HCl by parietal cells?
|
Direct - Gastrin in blood (G-cells) acts on CCK-2 receptors on parietal cells
Direct - ACh from PNS act on muscarinic M3 receptors on parietal cells Indirect - Gastrin acts on CCK-2 receptors on EnteroChromaffin-Like cells Direct - Activated ECL cells release histamin, which acts on H2 receptors on parietal cells |
|
|
Describe the main pathway of stimulation of parietal cells for HCl release?
|
Gastrin from G-cells stimulates CCK-2 receptors on ECL cells. They release histamine, histamine works on H2 receptors on parietal cells.
|
|
|
D-cells release somatostatin which inhibits HCl release, where are D-cells found in the stomach and how does this affect their method of activation?
|
D-cells are found in the pyloric antrum and the corpus of the stomach.
Antral D-cells are endocrine, releasing somatostatin to act systemically in response to rising intraluminal pH Corpus D-cells are paracrine, acting locally in response to neural/hormonal changes |
|
|
Somatostatin works directly and indirectly to prevent HCl release, how?
|
Antral somatostatin acts directly on parietal cell membranes, inhibiting adenyl-cyclase and antagonizing histamine acting on H2 receptors.
Antral somatostatin also inhibits gastrin release by G-cells, which indirectly inhibits HCl release Corpus somatostatin inhibits histamine release by ECL cells, which indirectly inhibits HCl release |
|
|
What inhibits somatostatin release?
|
It acts on D-cells as a self-inhibitory mechanism
|
|
|
What mechanisms outside of the stomach inhibit the release of gastric acid in the stomach?
|
Fats and acids in the duodenum and jejunum stimulate release of
a) Secretin, from duodenal S-cells b) VIP (Vasoactive Intestinal Peptide) c) GIP (Gastric Inhibitory Peptide) |
|
|
How does secretin inhibit gastric acid secretion?
|
It inhibits gastrin release by G-cells
|
|
|
How does VIP inhibit gastric acid secretion?
|
It stimulates somatostatin production by D-cells
|
|
|
What determines acidity in the stomach?
|
Not HCl, which is pretty continuous, but pepsinogen, which is alkali
|
|
|
How does Omeprazole work?
|
Irreversible blocker of H+/K+ ATP-ase, which is essential for getting H+ ion into parietal cells. 80% reduction in gastric acid secretion within 24hours.
|
|
|
What stimulates pancreatic enzyme secretion?
|
PNS ACh on muscarinic receptors, and secretin acting on CCK-2
|
|
|
What is the blood supply to the pancreas?
|
Splenic artery, running along it's superior surface
Superior and inferior pancreaticoduodenals, superior from Gastroduodenal, and Inferior from superior mesenteric |
|
|
What are the main components of pancreatic juice secretion?
|
Bicarbonate, proteolytic enzymes, lipases, amylase.
|
|
|
What order are secretions made within pancreatic cells?
|
Rough ER, Golgi, Condensing vacuoles, Zymogen granules.
|
|
|
Is GI smooth muscle single or multi-unit?
|
Single unit, cells connecting by gap junctions
|
|
|
Which mechanism operates within GI smooth muscle to limit the use of ATP?
|
The latch bridge mechanism
|
|
|
Actin and myosin are highly arranged in skeletal muscle, are they the same in smooth muscle in the GI?
|
No. Not highly arranged.
|
|
|
What effect does the PNS, CCK, GIP and secretin have on gastric motility?
|
PNS stimulation - increases motility
CCK - decreases motility Gastic Inhibitory Peptide - decreases motility Secretin - decreases motility |
|
|
Parasympathetic nerves can excite and inhibit GI motility, which neurotransmitters do what?
|
ACh - Excitatory
Vasoactive Intestinal Peptide and ADP - Inhibitory |
|
|
The sympathetic nervous system does what to GI motility, and via which neurotransmitter?
|
Noradrenalin, inhibits motility.
|
|
|
What is plasticity in relation to GI smooth muscle?
|
Ability to function over a wide range of lengths (occuring as it becomes distended with food)
|
|
|
What is the frequency of peristaltic waves in the stomach towards the pylorus?
|
3/min
|
|
|
What happens at the pylorus?
|
Vigorous mixing - either chyme is released into the duodenum (3ml), or forced back for further churning.
|
|
|
What 2 factors (one intrinsic and one extrinsic) regulate gastric emptying?
|
Extrinsic - Neural enterogastric reflex - when pH drops, gastrin secretion is inhibited
Intrinsic - Enterogastrone hormones (stop movement of food to anus) - CCK, somatostatin and GIP |
|
|
How fast do carbohydrates and fat move in the stomach?
|
Carbohydrate move quickly through duodenum, fats take longer so stay in the stomach
|
|
|
Describe the effects of these 4 hormones -
Secretin CCK GIP Motilin |
Secretin - stimulates secretion of HCO3- by pancreas, inhibits stomach activity
CCK - stimulates gallbladder release, contractions and emptying, inhibits stomach activity GIP - inhibits gastric contractions Motilin - increases gastric and intestinal motility |
|
|
How does the enteric nervous system affect gastric motility?
|
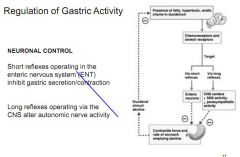
Short reflexes inhibit secretions and contractions
|
|
|
Describe the function and stimulation of the myenteric (Auerbach's) plexus and it's location.
|
Sits between inner circular and outer longitudinal smooth muscle layers, regulating their contraction.
Excited by ACh, inhibited by VIP |
|
|
Describe the function and stimulation of the submucosal (Meissner's) plexus and it's location.
|
In the submucosa, controlling muscularis mucosae and glands
Excited by VIP and ACh |
|
|
Other than their known individual functions, what functions do both the myenteric and submucosal plexuses perform?
|
Regulate absorption, blood flow and cell growth
|
|
|
How does secretin inhibit gastric emptying?
|
Inhibits contractions of the antrum, and stimulates contraction of the pyloric sphincter.
|
|
|
Are the nerves in the myenteric and submucosal plexuses myelinated?
|
No.
|
|
|
Are there inhibitory secretomotor neurones in the ENS?
|
No.
|
|
|
What is a peptic ulcer?
|
Chronic lesion in GI tract due to acid exposure
2:1 more common in men 99% in stomach/duodenum 4:1 duodenum to stomach |
|
|
Other than medication, what relieves a duodenal ulcer?
|
Eating - due to release of HCO3- from gall bladder, and reducing stress
|
|
|
Gastric ulcers damage the epithelium in the stomach, what is the difference between penetration and perforation?
|
A penetrating ulcer burrows into the pancreas or liver
A perforating ulcer goes through stomach and into the peritoneal cavity (causing peritonitis) |
|
|
What causes a gastric ulcer?
|
Low/normal HCl secretion, ulcer caused by defect in mucosal resistance. 75% infected with H.Pylori
|
|
|
What causes a duodenal ulcer?
|
Increased secretion of acid/pepsin causing defect. 95% infected with H.Pylori
|
|
|
How does H.Pylori survive in acidic conditions and go on to cause ulcers?
Grace a beef cheeks |
Secretes urease, converts urea -> bicarb + H20
Stimulates increased gastrin and pepsin secretion, causing raised levels of HCl secretion Also, some strains produce toxins (esp those with the CagA gene) which damage the mucosa |
|
|
What gene is said to determine pathogenicity of H.Pylori?
|
Cag
|
|
|
How does H. Pylori protect itself from the acidic environment of the stomach?
|
Secretes a urease which converts urea to HCO3- and CO2, protecting itself from gactric acid secretion.
|
|
|
Other than H.Pylori, what else causes gastric ulcers?
|
NSAIDs, smoking, cirrhosis, alcohol and Zollinger-Ellison syndrome
|
|
|
How do NSAIDs cause gastric ulcers?
|
Inhibit production of protaglandins, PGE stimulates epithelial and mucous neck cells to secrete mucus, and also inhibits parietal cells releasing HCl.
|
|
|
How does omeprazole work at neutral and acidic pH?
|
At neutral pH drug does not work but accumulates. At acid pH (<3) converted to Sulfenamide an irreversible antagonist of the H+ K+ ATPase (proton pump), leaving no energy to drive H+ secretion
|
|
|
Other than proton pump inhibitors like Omeprazole, what other drugs are used to treat ulcers?
|
H2 receptor blockers reduce effectiveness of histamine on parietal cells, but reduce effectiveness of other drugs so less preferred.
|
|
|
What is sucralfate and how does it work?
|
Enhances mucosal protection in duodenal ulcers and stress ulcers. The sulfated negative sucrose binds to and neutralises HCl, forming a viscous adhesive in the ulcer crater, and raises secretion of HCO3- and mucus
|
|
|
How does sucralfate work?
|
Binds HCl, forms a viscous adhesive which binds H+ in the ulcer crater. Buffering acid, also stimulates secretion of mucus, PGs and HCO3-
|
|
|
What is bismuth chelate?
|
Chelation therapy - aims to protect mucosa by coating ulcer, absorbs pepsin, stimulates mucus secretion, HCO3- and PGs.
|
|
|
Why are antacids prescribed?
|
Neutralise gastric acid, stopping pepsin from working. Provide mostly symptomatic relief.
|
|
|
What is misoprostil?
|
Stable PGE analogue - mimicks PGE, which stimulates mucus cells to secrete mucus, and inhibits parietal release of HCl
|
|
|
Why give antibiotics in a peptic ulcer case?
|
Kill H.Pylori, prevent relapse. Within a year 90% of patients have a relapse without antibiotic treatment, while under 10% relapse with antibiotic treatment.
|

