![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
What are the three barriers that invading microorganisms face?
|
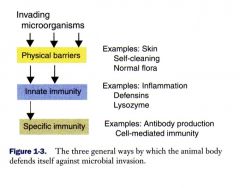
see the slide
|
|
|
what is the first line of defense in viral infections?
|
interferons (Interferon α/β are released from virus-infected cells
within a few hours after viral invasion) |
|
|
What are the major biological actions of interferson?
|
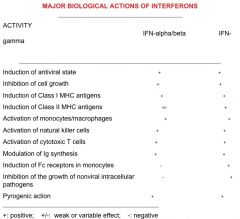
IFN gammas are the ones that stimulate the immune system.
The induction of MHCs is important as well as the pyrogenic action |
|
|
How long does it take the acquired immune system to peak?
What are the two pathways of it? |

Two weeks
TH1 helps Cytotoxic T's TH2 helps B Cells. T-cells recognize the processed antigens presented by MHC1 (with CD8), or the helper cells recognize MHCII (as they have CD4) |
|
|
What are the two main categories of invaders in terms of where they inhabit the host - and the immune responses necessary to target them?
|
1) Extracellular (exogenous)–live outside the cell
-Most bacteria, fungi most protozoa, helminths Humoral immune response Antibody destroy extracellular invaders Antibodies produced by plasma cells (fully differentiated B cell) 2) Intracellular (endogenous)-live inside the cell -Viruses -intracellular bacteria, protozoa Cell-mediated immune response T cell mediated |
|
|
What are some of the many roles of antibodies within humoral immunity?
|
1. Opsonization
2. MAC Cytolysis 3. Antibody-dependent Cellular Cytotoxicity (ADCC) by NK Cells 4. Neutralization of Exotoxins 5. Neutralization of Viruses 6. Preventing virus Adherence to Host Cells 7. Agglutination of Viruses 8. Immobilization of Viruses. |
|
|
What is cell-mediated immunity?
|
It is an immune response that involves the activation of macrophages and NK-cells, the production of antigen-specific cytotoxic T-lymphocytes, and the release of various cytokines in response to an antigen.
|
|
|
What are the antigen-presenting cells?
How do they interact with T cells? |
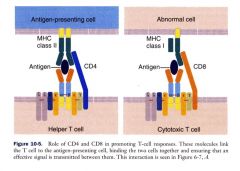
Macrophages, Dendritic cells, or B cells.
These guys present MHCII to helper T cells. In contrast to abnormal cells that are virus-infected or tumor cells - they will present MHCI which will be recognized directly by Ctyotoxic T cells that will lyse them through perforins and granzymes. |
|
|
How do vaccines work?
|
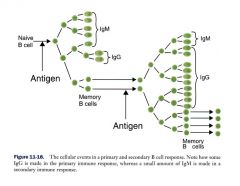
The first antigen is the primary vaccine, the second is the booster.
You're inducing memory B and T cells by stimulating IgM and then the second time lots of IgG. |
|
|
There are 8 types of vaccines - what are they?
|
1 Live whole virus vaccines - very important for intracellular pathogens, like virus
2 Killed whole virus vaccines - very important for extracellular pathogens, like bacteria 3 Subunit vaccines;- purified or recombinant viral antigen 4 Recombinant virus vaccines --Marker vaccine 5 Synthetic peptides 6 Anti-idiotype antibodies - will mimic the antigen by forming its complement shape to bind to it 7 DNA vaccines 8 Peptide vaccine - 19 or 20 peptides used to produce mulitclonal antibodies for research purposes. |
|
|
What are the core vaccines of puppies?
|
Puppies: Canine Distemper, Canine adenovirus-1, Canine adenovirus-2, Canine parvovirus-2, Canine parainfluenza virus, Leptospira bacterin
First dose between 6-9 weeks Second dose between 9-12 weeks Third dose between 13-16 weeks Rabies vaccine given at 16 weeks If the risk of kennel cough is great, a vaccine against bordetella is recommended. |
|
|
What are the core vaccines of kittens?
|
Feline rhinotracheitis, feline calicivirus, & feline panleukopenia virus (distemper)
First dose 6-9 weeks; Second dose 9-12 weeks; Third dose 12-14 weeks Feline Leukemia virus (FeLV) First dose 9-12 weeks; Second dose 12-14 weeks Rabies virus vaccine given at 12 weeks. |
|
|
What are the vaccination protocols for calves and foals?
|
A safe rule is to vaccinate no earlier than
3 to 4 months of age followed by one or two revaccinations at 4-week intervals. The precise schedule will depend on the vaccine used and the species to be vaccinated. Animals vaccinated before 6 months of age should always be revaccinated at 6 months or after weaning to ensure protection |
|
|
What type of vaccine should you use intranasally and intraorally?
|
Inactivated antigens are usually not effective in triggering IgA response.
Modified live vaccines can trigger significant IgA response. Respiratory tract vaccines Bovine or feline rhinotracheitis, bovine PI-3 Live oral vaccines Transmissible gastroenteritis (TGE) vaccine in piglets Rotavirus vaccine in calves [to prevent diarrhea (calf scours)] Polio vaccine in humans |
|
|
What is the antibody that responds in the respiratory and intestinal tract?
|
Microbes which cause local infections such as the respiratory tract (rhino virus) or the intestinal tract (rota virus), IgA response is effective in preventing the infection
|
|
|
Can you induce secondary immune response on mucosal surfaces? Why or why not?
|
Secondary immune responses for IgA are difficult to induce on surfaces. You may get secondary IgG response from boosters, but not to block the mucosal surface.
Multiple doses of vaccine may not increase the intensity or duration of the local immune response. This occurs because high levels of IgA can block antigen absorption and prevent it from reaching antigen-presenting cells (APCs). |
|
|
What are the basic types of evasion strategies?
|
Passive Mechanisms - won't kill the cell or effect the immune system
2 Active Mechanisms - Host-specific and highly subversive, active strategies often involve the production of pathogenic immunomodulatory proteins which alter normal host protein function and general immune function. 3 Aggressive Mechanisms - directly target the immune system (like HIV) |
|
|
What are the four kinds of passive mechanisms of evasion?
|
1 Evasion by noncytocidal infection
2 Evasion by cell-to cell spread (membrane fusion - form a giant syncytia) - by doing that, the virus isn't exposed to the immune system. 3 Evasion via infection of nonpermissive cells 4 Restricted Viral Gene Expression - will hide inside the cell without producing proteins (eg Herpes virus) |
|
|
Which viruses replicate in rodent hosts without killing the cells? What kind of evasion strategy are they utlizing?
|
Arenaviruses
Hantaviruses These guys use Evasion by noncytocidal infection - a passive mechanism of evasion. |
|
|
What viruses cause adjacent cells to fuse together and enable the viral genome to spread contiguously from cell to cell without ever being exposed to the host's immune system?
What mechanism of evasion are they utilizing? |
Lentiviruses (EIAV)
Morbilliviruses (CDV) CMV - cytomegalovirus They use Evasion by cell-to cell spread (membrane fusion), a passive mechanism of evasion. |
|
|
What is evasion via infection of nonpermissive cells?
What are two viruses that employ this strategy? |
A type of passive evasion.
Evasion by infecting of nonpermissive, resting, or undifferentiated cells: Papillomaviruses: nonpermissive in basal cells of stratifies epithelium, but productive in fully differentiated cells near body surface. Herpesviruses: latent in ganglionic neurons or B cells but productive infection in mucosal epithelial cells. |
|
|
What is the strategy of restricted viral gene expression used for?
|
This is a passive mechanism of evasion.
Eg: Herpesviruses: only a few genes being expressed during latency to avoid host immune actions. |
|
|
One of the mechanisms of active evasion used by viruses is the evasion of neutralizing antibody. How does this mechanism work?
|
Making immune decoy molecules:
Flioviruses Arenaviruses They express two forms of the same glycoproteins: one forming its surface peplomers the other is a truncated version of the same protein, but made in large amount, can “soak up” the neutralizing antibody and protect the virus. |
|
|
How can viruses interfere with endogenous antigen processing as part of the active mechanism of evading immunity?
|

see pic
|
|
|
How does the active mechanism of evading the immune system by evading the complement pathway work?
|

This is another one employed by herpes virus. There are many different pathways that can be blocked - everything in red are different steps where a virus can block the complement pathway.
|
|
|
How does the aggressive mechanism of evading the immune system work? (two mechanisms mentioned)
|
Infect cells essential for immune function (T and B lymphocytes, monocytes), thereby causing immunosuppression.
-HIV, the measles virus, EBV 1. Destruction of immune cells (HIV destroy CD4 T cells and macrophages, Virokines) 2. Virus-induced immunosuppression The best known example is AIDS, Measles and influenza infection can reduce host resistance to other infectious agents, which may lead to secondary infections--especially bacterial. Examples: pneumonias due to Streptococcus pneumoniae or Hemophilus influenzae following influenza or measles virus infections. |
|
|
What do virokines do to interfere with the immune system?
|
Virokine: counteract cytokine actions
Viruses have developed intricate mechanisms to circumvent the protective actions of cytokines. Epstein-Barr (EB) virus codes for a protein termed BCRF-1, which shows a high degree of homology to the cytokine IL-10. One of the major functions of IL-10 is to inhibit the synthesis of cytokines produced by the TH1 subset of T cells, i.e., the generation of IFN-gamma, IL-2, and TNF-beta/lymphotoxin. |
|
|
Where are B cells mostly found?
|
Secondary lymphoid orgains - spleen, lymph nodes
T cells circulate |
|
|
What is a serpin?
|
SERum Protein INhibitors - anti-apoptotic, anti-inflammatory
|
|
|
Summarizing question. What are strategies that viruses can evade the immune response?
|
-Induction of non-neutralizing antibody
-Induction of immunologic tolerance -Infect immunologically previleged tissues (eyes, brain, testes) -Integration of viral genome into host cell genome -Genetic/antigenic drift -Inhibition of MHC class I-restricted Ag presentation -Inhibition of MHC class II restricted-antigen presentation -Destruction of CD4 T cells, Macrophages -Inhibition of natural killer cell lysis -Interference with apoptosis -Inhibition of cytokine action -Evasion of humoral immunity |

