![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
Describe the structure of Vibrio Cholera?
|
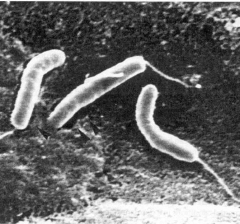
gram (-), Curved bacilli (comma shaped)
Flagellum (motile) Faculative aerobe or anaerobe Commonly found in saltwater Lactose non fermenter Oxidase + Ferments glucose (seperates from p. aeruginosa) |
|
|
What is MOA of cholera toxin?
Who shares this MOA? |
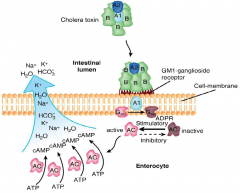
AB toxin
ribosylates Gs increasing cAMP -> increases Cl secretion & decreases Na absorption -> Loss water resulting in watery diarrhea and dehydration This is the same MOA as E Coli Enterotoxins (LT/ST) |
|
|
How does one treat Vibrio Cholera?
|
Oral/IV rehydration therapy
If oral use Glucose + Na to utilize Na-Glu cotransporters of small intestine Tetracycline |
|
|
What is the clinical manifestations of Vibrio Cholera?
|
Voluminous rice water stools (w/ mucous)
Dehydration & electrolyte imbalance |
|
|
How is Cholera Diagnosed?
|
stool cultures showing "comma shaped" rods
flat yellow colonies on TCBS agar |
|
|
How can we prevent Vibrio Cholera? What is the world spread of Vibrio Cholera?
|

Killed cell vaccine (limited efficacy)
Cook seafood General Sanitation ----------------------------------- First case US 1911, Many in 1970s - Associated with Gulf and inadequately cooked crab & shrimp 1991 Latin America - Endemic in peru - mexico Assoc. Infrastructure deterioration - Zimbabwe &n Haiti |
|
|
How is Vibrio Cholera spread? What are predisposing factors?
|
Spread by contaminated water but may remain in inactive state in plankton, crustaceans ect.
|
|
|
What is the pathogenesis of Vibrio Cholera?
|
Requires large inoculums (overcome Gastric HCl) -> produces mucinase to bypass protective layer in small intestine ->Attaches using TCP (toxin corrugated piili?) to small intestine (no invasion) and secretes CT.
|
|
|
How does one die from Vibrio Cholera?
|

From the dehydration aspect. It can cause Metabolic acidosis (loss HCO3)
Hypovolemic shock & death w/o treatment |
|
|
What are the properties of Helicobacter Pylori?
|
Microaerophilic (8-10% O2)
polar flagellum (motile) Small curved bacilli (spiral shaped) gram (-) bacteria Produces urease |
|
|
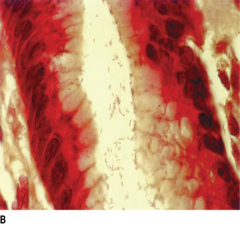
Describe the histological pathology that H Pylori causes?
|
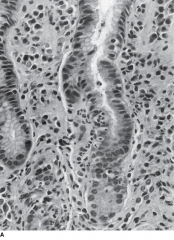
Gastritis that leads to Ulcers (think anemia)
Gastric mucosa shows infiltration of neutrophils and destruction of epithelial cells. |
|
|
What cancers are associated with H Pylori?
|
Gastric adenocarcinoma (WHO class 1 carcinogen)
Gastric Mucosa Associated Lymphoma (MALT) - which can be reveresd by antimicrobial treatment |
|
|
How does H Pylori clinically present?
|
Often asx for decades
Acute - gastritis Chronic - antral/pan gastritis, peptic ulcers (anemia?) Can cause nausea, epigastric pain, bleeding, perforation which can lead to acute abdomen |
|
|
What are the virulence factors of H. Pylori?
|
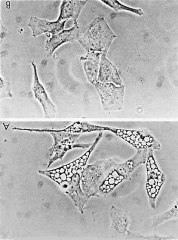
1. Urease - allows organism to survive low pH enviroment through production of NH3
2. Vacuolating Cytotoxin (VacA) - causes apoptosis after entering cell. (forms multiple large cytoplasmic vacoules) 3. Cag protein - Injected & causes actin reorganization & activation of host proteins 4. |
|
|
What is the pathogenesis of H pylori?
|
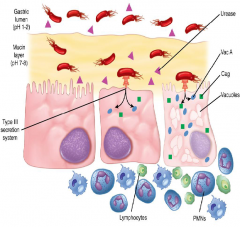
Stomach Colonization (2)
motility aids in penetration of mucus & urease raises the pH (inhabitable) Injection (type 3 secretion) Injects both VacA & Cag proteins into host Inflammation Caused by Urease, VacA, & Cag proteins Uncertain how it progresses to ulcer |
|
|
What is the PAI in H pylori important for?
|
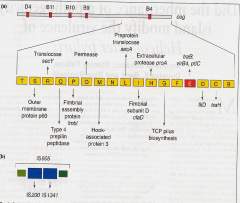
Presence of secretion systems, Cag & VacA proteins
|
|
|
How is H pylori diagnosed?
|
Endoscopy - culture Gram (-) bacilli on special agar or detection of urease
Serology - IgG or IgA Abs Can detect stool Ag and this is used to follow therapy Unique - labeled urea breath test |
|
|
How is H Pylori treated?
|
Bismuth salts - peptobismol
Antibioitics - metranidazole, tetracycline, amoxycillin, clarithromycin Bismuth salts + PPI + 2 Antibiotics = 95% cure rate |
|
|
How is H pylori transmitted?
|
fecal-oral or oral-oral
|
|
|
How is Campylobacter jejuni spread?
|
Carried in poultry, dogs, domestic animals & can be transmitted fecal-oral or in unpasteurized milk
|
|
|
What is the structure of Campylobacter jejuni?
|
Microaerophilic (8-10% O2)
Gram (-) curved bacilli (s shaped) Polar flagellum (motile) slow growing Low infecting dose (10^2-10^3) Negative for Urease (oppose H pylori) |
|
|
Why does Campylobacter jejuni cause disease?
|
colonizes ileum/colon and invades, ? releases enterotoxin and cytotoxin
Causes fever, ill-smelling diarrhea & bloody stools |
|
|
What neurological syndrome is associated w/ Campylobacter jejuni and how might this occur?
|
Guillian-Barre syndrome
A demylinating neuropathy (ascending paralysis) that often shows up 1-3wks after infection Thought to be type 2 hypersensitivty w/ molecular mimicry of LPS that cross reacts w/ peripheral nerve myelin |
|
|
How would campylobacter jejuni present?
|
1-7d post ingestion
Fever with Diarrhea to dysentery spectrum Causes lower Abdominal pain It is responsible for 5-30% of diarrhea worldwide |
|
|
How is campylobacter jejuni diagnosed?
|
Cultured on a routine media (2-4days) in microaerophilic conditions
|
|
|
Why don't we see more cholera in the US?
|
Good infrastructure and sanitation standards are in place. Generally crabs and shrimp are well cooked
|
|
|
How does H Pylori survive the acidic environment in the stomach?
|
It has urease which secretes NH3 that aids in raising the pH.
|
|
|
What type of growth are Vibrio cholera, Campylobacter jejuni and Helicobacter jejuni?
|

|
|
|
How is Campylobacter jejuni treated?
|
Ciproflaxacin or erythromycin
It is generally self limiting after 3-5days |

