![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back

|

|
|
|
|
|
|
Osteoblast
|
Bone cell that produces osteoid
|
|
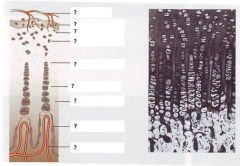
Label
|
|
|
|
Osteoid
|
ECM matrix produced by osteoblasts
|
|
|
Osteocytes
|
Trapped osteoblasts
|
|
|
Lacunae
|
Spaces in calcified bone containing osteocytes
|
|
|
Canaliculi
|
Small canals linking lacunae with trapped osteocytes
|
|
|
Haversian systems
|
3D structure or concentric rings within compact bone
|
|
|
Osteoclasts
|
Cells (multinucleated) that remodel bone
- monocyte/macrophage lineage |
|
|
Periosteum
|
Connective tissue membrane covering bone
|
|
|
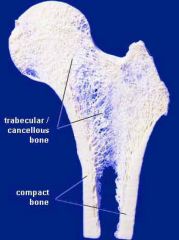
Compact bone (type of lamellar bone - mature)
- brief description |
Outer layer of cortex of all bones
- filled with densely packed Haversian systems |
|
|
Spongy or cancellous bone (type of lamellar bone - mature)
- what is it? - where's it found? |
Spicules of bone arranged as a trabeculae meshwork or lattice
- form a network within the ends of long bones and core of short and flat bones - medullary cavity (spaces filled with bone marrow) |
|
|
Bone & skeleton
- 3 main functions |
Strength: structure and support
Mobility: movement Mineral reservoir |
|
|
Main components of cartilage
|
Cells: chondrocytes
ECM (collagen proteoglycans ) water (80-90%) ***NO bvs, lymphatics, nerves*** |
|
|
Main components of bone
|
Cells: osteocytes, osteoblasts, osteoclasts
ECM (mineral, collagen, GAGs) **Blood vessels, lymphatics, nerves** |
|
|
Collagen resists ? strain
|
? resists tensile strain
|
|
|
Proteoglycans resist ? strain
|
? resists compressive strain
|
|
|
2 main types of bone
|
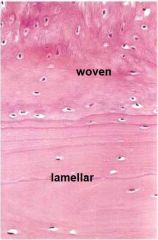
Woven (immature)
Lamellar (mature) |
|
|
2 types of lamellar bone
|
Compact (cortical)
Cancellous (trabecular, spongy) |
|
|
Immature bone
- where found (3)? |
Confined to areas of rapid bone formation
- developing skeleton - fracture callus - bone diseases (eg hormonal, tumours) |
|
|
2 types of ossification
|
Intramembranous ossification
Endochondral ossification |
|
|
2 sites of intramembranous ossification
|
Bone development at;
- flat bones - periosteal surfaces (is this repair?) |
|
|
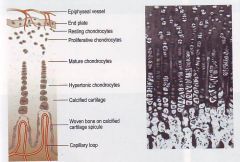
Endochondral ossification
- 4 overall steps |
Chondrocyte proliferation and hypertrophy
Periosteal invasion bringing blood vessels and osteogenic cells Woven (immature) bone deposited Lamellar (mature) bone replaces woven bone |
|
|
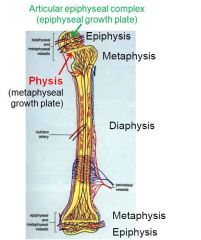
Articular cartilage provides ? growth
|
___ cartilage provides epiphyseal growth
|
|
|
Growth plate cartilage provides ? and ? growth
|
___ ___ cartilage provides metaphyseal and diaphyseal growth
|
|
|
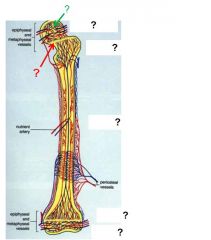
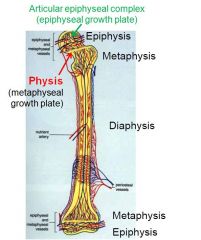
Articular epiphyseal complex = ____
Metaphyseal growth plate = ____ |
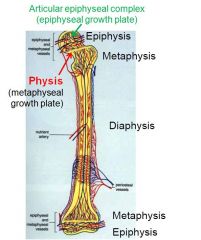
___ = (epiphyseal) growth plate
___ = physis |
|
|
Define modelling
- what are the two types |
Modelling is the processes leading to changes in size and shape of bone
- primary remodelling - secondary remodelling |
|
|
Define stress
|
___ is the force exerted on bone
|
|
|
Define strain
|
__ is the effect of the stress on bone
|
|
|
What are the two types of strain on bone?
- where do they act? - which cell types are most active? |
Tensile strain:
- convex, osteoblastic Compressive strain: - concave, osteoclastic |
|
|
Primary remodelling
- occurs when? |
___ remodelling occurs during growth and is the replacement of young bone with adult bone
|
|
|
Secondary remodelling
- occurs when? |
___ remodelling continues throughout life and is the replacement of old bone with new bone
|
|
|
Molecules that allow osteoblasts and osteoclasts to communicate (coupling)?
|
RANK-L and RANK-R
|
|
|
Why does hypercalcaemia occur during some cancers?
- associated with what cancers in the dog? |
Some tumour cells secrete a soluble form of RANK-L triggering osteoclastic activity.
Some tumours secrete a PTH-like molecule triggering Incr. osteoclast activity - commonly lymphoma & anal gland adenocarcinoma |
|
|
3 main molecules controlling bone composition
|
VitD
PTH Calcitonin |
|
|
Actions of VitD in two main sites
|
Intestine
- incr. Ca and P absorption Bone & cartilage - incr mineralisation |
|
|
__ are the major sensors of variation in plasma calcium
|
Parathyroid gland cells are the major sensors of plasma ___
|
|
|
When plasma calcium falls, ___ synthesis and release is enhanced
|
When ___ falls, PTH synthesis and release is enhanced
|
|
|
Actions of PTH at 2 main sites
|
Kidney
- incr tubular resorption of Ca and tubular excretion of P - incr. VitD active form Bone - incr osteoclast numbers and activity |
|
|
___ is the physiologic antagonist of PTH
and is secreted by ___ |
Calcitonin is the physiologic antagonist of ___
and is secreted by the parafollicular (C) cells of the thyroid |
|
|
Actions of calcitonin at 2 main sites
|
Kidney
- decr. tubular resorption of Ca & P Bone - decr osteoclast activity |
|
|
When plasma calcium rises, ___ secretion is enhanced.
|
When ___ rises, calcitonin secretion is enhanced
|
|
|
Fractures repair by the process of __ __
|
Fractures repair by the process of secondary intention (edges not in close apposition)
|
|
|
List the stages of fracture repair
- include duration |
Reactive
- haematoma (immediate) - granulation (within 48h) Reparative - primary callus (after 7d, max 3w) - secondary callus (mo - y) Remodelling (mo - y) |
|
|
Discuss organisation and granulation tissue formation in fracture healing
|
Within 48h,
capillaries & fibroblasts enter haematoma produce granulation tissue - has potential to undergo metaplasia to cartilage and bone |
|
|
What comprises a primary callus in fracture healing
|
Fibrous tissue, cartilage, woven bone
- osteoprogenitor cells in periosteum and endosteum produce external and internal calluses - woven bone laid down in these calluses - bridge forms between ends |
|
|
What comprises a secondary callus in fracture healing
|
Endochondral ossification of cartilage
- woven bone is replaced by lamellar bone |
|
|
Factors (8) contributing to delayed union of bone fractures
|
Movement (instability, mechanical stress)
Infection High glucocorticoids Poor blood supply Displaced bone ends Necrotic fragments in bone Foreign body at fracture site Underlying primary bone disease |
|
|
Factors (2) causing non-union of bone fractures
|
Fracture ends united by scar tissue
Poorly differentiated fibrocartilage over bone ends |
|
|
Likely 2 fates of necrotic bone at a fracture site
|
May be incorporated into the callus and repopulated by osteoblasts and osteocytes providing blood supply re-established. Eventual remodeling
Persist as necrotic sequestrum, cyst or abscess |
|
|
Pseudoarthrosis
|
Can form after fracture repair with poorly differentiated fibrocartilage over bone ends and central cavity lined by synovial cells
|
|
|
Effects on bone of increased mechanical stress in
- young - adult |
Young: increases metaphyseal trabecular bone & thickness of cortices
Adult: Reduces remodelling, conserves bone present |
|
|
Effect of mechanical reduced stress on adult bone
When is this important? |
Increases resorption -> decreased bone strength
- imp when bone immobilised, weightless, prolonged disuse |
|
|
What is the weakest part of a long bone in the growing animal?
|
The growth plate
|
|
|
What is epiphyseolysis?
When can it occur? What is the prognosis? |
Complete seaparation of epiphysis from metaphysis in growing animal
- dt horizontal shear forces Prognosis is good if the proliferative zone and blood supply remain intact. |
|
|
Why can epiphyseolysis at the proximal femur result in avascular necrosis
|
Greater risk of vascular damage as the nutrient vessels run along the neck of the femur
|
|
|
How can an angular limb deformity result?
|
Damage to blood supply and/or chondrocytes in the proliferation zone on one side only of a growth plate
|
|
|
What are exotoses
|
Localised outgrowth of new bone beneath the periosteum dt periosteal damage leading to activation & proliferation of osteoblasts
|

