![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
141 Cards in this Set
- Front
- Back
|
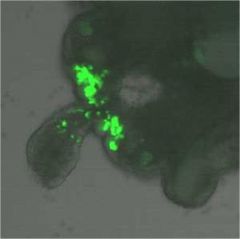
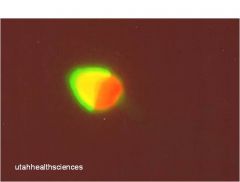
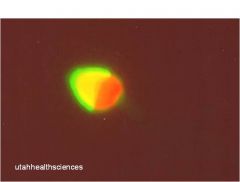
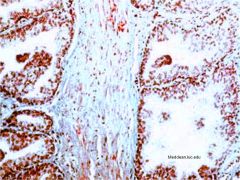
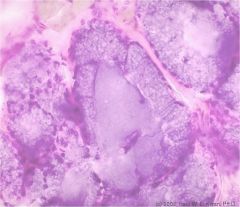
primordial germ cell migration
notice yolk sac towards left and bright green germ cells in the genital ridge |
|
|
purpose of the yolk sac
|
Germ cells come from yolk sac
Once primitive gut starts to form, the cells migrate out of the yolk sack to the genital ridge of the celomic cavity to be. |
|
|
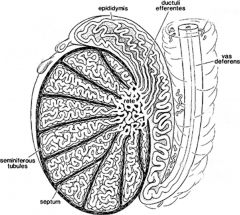
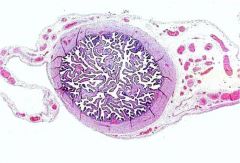
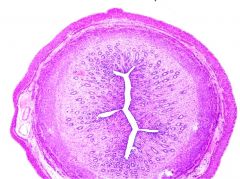
know the structures of the testis, epididymus, etc
|
|
|
|
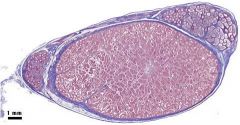
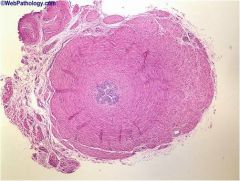
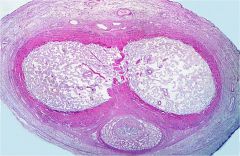
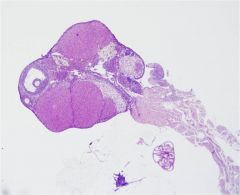
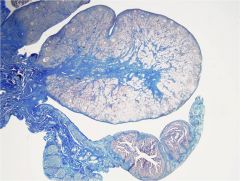
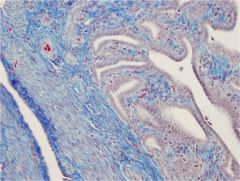
testis (center)
epididymus (mickey's ears) notice the fibrous tunic trichrome stain |
|
|
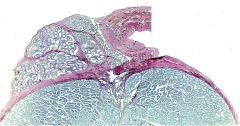
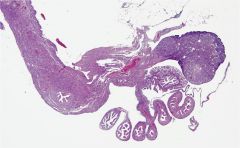
testis (bottom)
fibrous tunic (purple) epididymus (top left) collecting ducts (to the right of the epididymus) trichrome |
|
|
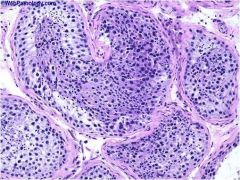
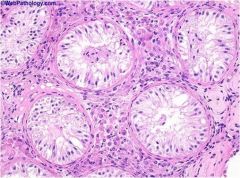
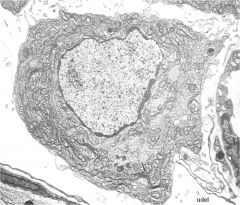
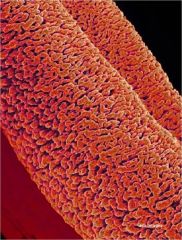
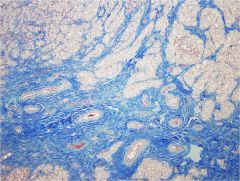
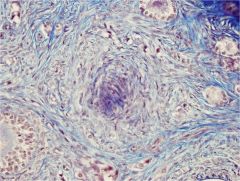
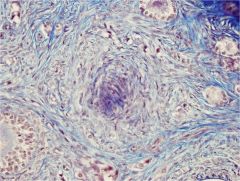
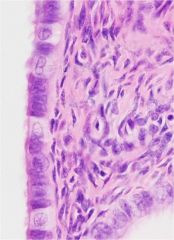
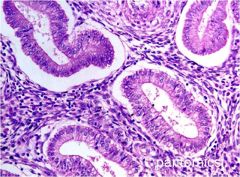
semininferous tubules (cross section of convoluted tubules)
each tubule is separated from each other by fibrous tissue and some smooth muscle |
|
|
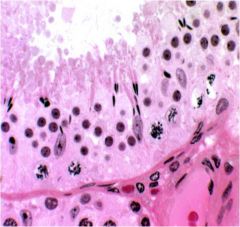
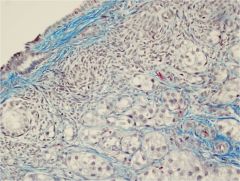
spermatogenesis
spermatogonia (diploid) - outermost 2 layers spermatocytes (haploid) - next 2 layers spermatid (haploid) - next 2 layers not nearly as much CT or smooth muscle maturation occurs from lamina -> luminally |
|
|
spermatogonia
these are the cause of cancer |
|
|
|
primary spermatocyte
|
|
|
secondary spermatocyte
|
|
|
primary spermatocyte
|
|
|
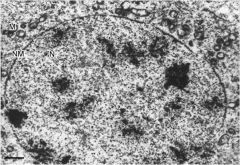
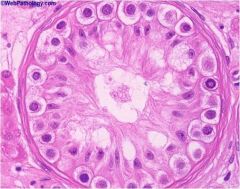
round spermatid
big open nuclei with prominent nuclear membrane |
|
|
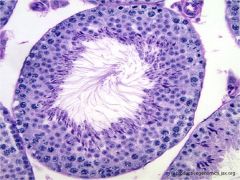
acrosomal cap
|
|
|
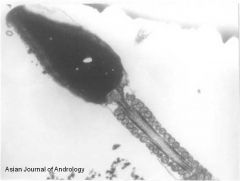
spermatid
nucleus basal plate flagella |
|
|
acrosomal cap
|
|
|
sertoli cells
Oriented perpendicular to basal lamina Kite shaped nuclei Prominent nucleoli Reaches inbetween spermatid Tight junctions Fxn - Nutrient suppport - Structural support - For sperm development |
|
|
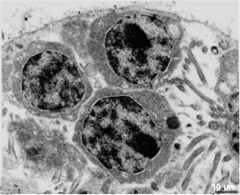
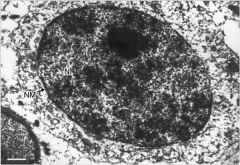
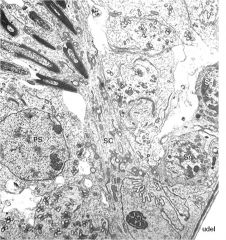
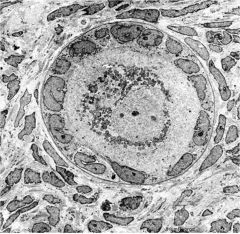
sertoli cell (SC)
- Nuclear indentation - prominent nucleolus. - well defined mitochondria - Processes extend luminally PS = spermatocyte Sg = spermatogonia |
|
|
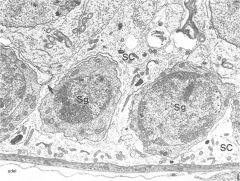
sertoli cell around spermatogonia
|
|
|
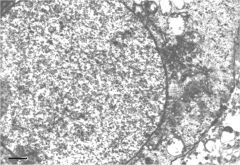
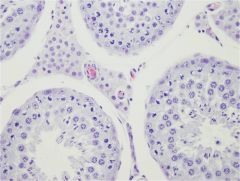
sertoli-cell-only syndrome
(germ cell aplasia) |
|
|
maturation arrest
spermatogonia forget how to function so only have sertoli cells and spermatogonia |
|
|
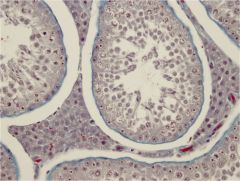
leydig (interstitial) cells
Polygonal to round Lipid present Foamy Produce testosterone when leutenizing hormone present |
|
|
leydig (interstitial) cells
Polygonal to round Lipid present Foamy Produce testosterone when leutenizing hormone present |
|
|
leydig cell
Polygonal to round Lipid present Foamy Produce testosterone when leutenizing hormone present |
|
|
rete testis
|
|
|
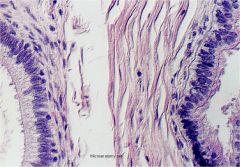
vas deferens
smooth muscle around and fibrous CT around that proximal end used for storage |
|
|
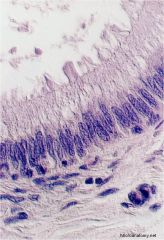
vas deferens
lined by pseudostratified columnar epithelium with basal layer goes to urethra where it becoms transitional epithelium |
|
|
efferent ducts
Columnar ciliated cells And cuboidal secretory cells |
|

|
epididymus
smooth muscle surrounded by fibrous CT movement within epididymus is by peristaltic contraction of smooth muscle (only during ejaculation) |
|
|
epididymus
|
|
|
epididymus (left)
smooth muscle loose CT efferent duct (right) |
|
|
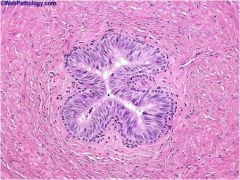
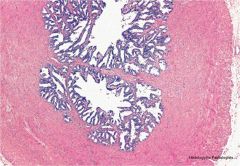
ampullary region of vas deferens
highly branched glands that open directly into vas deferens most secretory fxn in - nutritive - control pH - change viscosity |
|

|
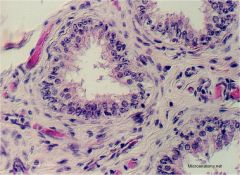
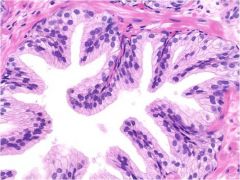
seminal vesicle
lobulated pinna, areolar form, papillary forms columnar epithelium produces very viscous, sugar laden fluid (fructose) |
|

|
seminal vesicle
lobulated pinna, areolar form, papillary forms columnar epithelium produces very viscous, sugar laden fluid (fructose) |
|
|
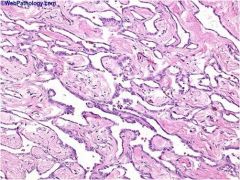
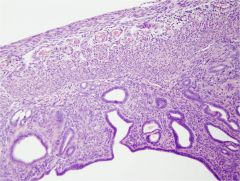
prostate (trichrome)
dense to loose CT pathological = increase CT in dogs human neoplasia = increase epithelium |
|
|
prostate
cuboidal to columnar ciliated epithelium |
|
|
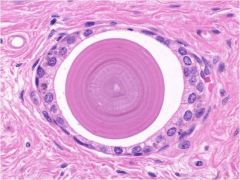
prostatic corpora amylacea
|
|
|
describe the prostate
|
Sits around urethra on either side
2 forms Capsular form - What you feel on rectal - Barbie’s butt Disseminated form - No distinct capsule |
|
|
bulbourethral gland
flattened basal nucleus mucinous alkaline material in lumen |
|
|
bulbourethral gland
flattened basal nucleus mucinous alkaline material in lumen |
|
|
corpora cavernosa
|
|
|
penis (cross section)
loose areolar CT around outside squamous epithelium (outside) dogs = more vascular ruminants = more fibrous type |
|
|
primordial germ cells become
|
spermatogonia
|
|
|
supportive cells become
|
sertoli cells
|
|
|
some mesenchymal cells become
|
intersitial cells (leydig cells)
|
|
|
genital ridge mesenchyme forms
|
CT
blood vessels intersitial tissue stroma etc. |
|
|
coelomic epithelium migrates into the genital ridge forming _____
|
supportive cells
female - follicular epithleium male - sertoli cells |
|
|
primitive sex cords contain what cell types?
where do they start? where do they go? |
contain
- gametogenic cells (from primordial germ cells) - supportive cells (from coelomic epithelium) start at periphery (cortex) of the gonad and penetrate into the center (medulla) |
|
|
how is sexual differentiation hierarchal
|
Determined 1st by chromosomal makeup, then by gonadal makeup, then by other cells that tell it what to do
Differentiation is: 1) Chromosomal (XX or XY) 2) Gonadal (ovary or testes) 3) Phenotypic (accessory glands, uterus, ducts, etc) |
|
|
female with male characteristics
|
no mullerian inhibiting hormone from sertoli cells
|
|
|
male with female characteristics
|
no testosterone or inadequate testosterone receptors
testosterone is from leydig cells |
|
|
ovary formation
|
in absence of Sex Determining Region Y, primitive gonad becomes an ovary
primordial germ cells become oogonia then primary oovytes supportive cells become follicular epithelium some mesenchymal cells become thecal and stromal cells (leydig cells) the cortical primitive sex cords become follicles |
|
|
duct systems in males are originally
|
both mulllerian (paramesonephric) and wolffian (mesonephric) ducts
|
|
|
both mulllerian (paramesonephric) and wolffian (mesonephric) ducts
|
both mulllerian (paramesonephric) and wolffian (mesonephric) ducts
|
|
|
male duct development
|
expression of SRY causes sertoli cells to produce anti-mullerian hormone which makes mullerian duct degenerate
testosterone produced by leydig cells leads to differentiation of the wolffian duct into the epididymis, vas deferen, and the seminal vesicle |
|
|
female duct development
|
in the absence of anti-mullerian hormone, the mullerian duct persists.
the mullerian duct gives rise to uterus, cervix, upper 1/3 of vagina, and fallopian tubes in the absence of testosterone, the wolffian duct degenerates and gives rise to broad ligament of the uterus and dorsal vaginal wall |
|
|
male and female external genitalia differentiation
|
Male
- penis and scrotum differentiate from lateral plate mesoderm under testosterone - prostate is derived from urogenital sinus which is derived from the cloaca female - external genitalia differentiate from lateral plate mesoderm - lower vaginal vault is derived from the urogenital sinus, which is derived from the cloaca |
|
|
_____ is the site of spermatogenesis
|
testis
|
|
|
spermatogeneisis is regulated by
|
FSH (stimulates spermatogenic epithelium)
LH (stimulates testosterone production) |
|
|
is the testis functionally endocrine or exocrine
|
it is both
|
|
|
describe the testis
|
surrounded by dense white fibrous CT (tunica albugenia) which extends inward to form a central septum (mediastinum testis) that arborizes to subdivide the testis into numerous lobules.
w/in each lobule are highly coiled seminiferous tubules (convoluted tubules) the convoluted tubules converge into lobar straight tubules whihc lead into the rete testis |
|
|
describe each seminiferous tubule
|
surrounded by 1-4 layers of smooth muscle cells
smooth muscle abuts a basal lamina supporting tubular seminiferous epithelium which is composed of 2 types of cells (spermatogenic & sertoli cells) |
|
|
spermatogenic cells
|
undergo serial maturation w/in the seminiferous tubule
the most mature cells are closest to the lumen takes about 2 mo spermatogonia spermatocytes spermatids spermatozoa |
|
|
spermatogonia
|
diploid
differentiated from primordial germ cells always in contact with basal lamina 2 subtypes - A: stem cells - B: precursors that undergo multiple mitoses to finally form spermatocytes |
|
|
spermatocytes
|
larger than and lie luminal to spermatogonia
hapliod cells are in prolonged 1st meiosis or rapid second mitosis after 2nd mitosis they are spermatids |
|
|
spermatids
|
lie in the luminal part of the seminiferous epithelium
small with an initially very light eccentric nucleus that becomes smaller and darker |
|
|
the last part of spermatogenesis is _____
|
spermiogenesis
maturation of spermatids to spermatozoa |
|
|
describe spermatozoa
|
head
- nucleus - anterior is covered by acrosome (contains enzymes impt in fertilization) - posterior forms basal plate neck - short and attached to basal plate - transversely oriented centriole is located immediately behind the basal plate - 9 segmented colums of fibrous material that continue into the tail tail - connecting - principle - end piece - in connecting and principle piece, the axonema and dense fibers are surrounde by a sheath of mitochondria |
|
|
what is the fxn of sertoli cells
|
provide mechanical and nutritive support for the spermatogenic cells
secrete numerous proteins including hormones (inhibin and activin) which provide + and - feedback on FSH secretion from the pituitary |
|
|
describe sertoli cells
|
irregularly columnar
extends from basal lamina to lumen extend processes b/w spermatogenic cells nucleus kite shape, large, pale, with large nucleolus |
|
|
between the seminiferous tubules is _____
|
continuous interstitial region composed of loose, highly vascualrized fibrous CT & leydig cells
|
|
|
______ produces androgens (testosterone)
|
leydig cell
|
|
|
rete testis
|
lobular straight seminiferous tubules converge into the rete testis in the mediastinum tesis
the rete is a cavitary labyrinth lined by low cuboidal to flattened epithelium supported by fine fibrous septa |
|
|
testicular efferent ducts
|
from rete testis, spermatids enter effernt ducts
lined by cuboidal absorptive epithelium and cuboidal ciliated epithelium of varying heights duct epithelium is supported by fibrous CT efferent ductular absorptive cells remove up to 90% of luminal fluid produced during spermatogenesis ciliated cells move sper to epididymus |
|
|
epididymus
|
coiled tube which spans the length of the testis
lumen is lined by pseudostratified columnar epithelium with long apical stereocilia (not motile, but secretory and absorptive fxns) lipid droplets in basal cells lamina propria - vascular loose (areolar) CT thickness of muscularis increases proximal to distal (most conspicuous at the tail) sperm moved by spontaneous peristaltic contractions in head and body sperm undergo final matuation in middle segment tail is a site of storage for mature spermatozoa |
|
|
vas deferens
|
fibrovascular wall tube with highly folded mucosa lined by pseudostratified columnar cells
muscularis thick with 2 distinct layers |
|
|
the proximal portion of the vas deferens is a component of ______ and serves for _____.
the distal end _____ |
spermatic cord
serves for sperm storage widens to form an "ampulla" |
|
|
vesicular glands
|
seminal vesicles
rimmed by thin smooth muscle layer epithelium is tall columnar |
|
|
accessory glands of the male repro system
|
ampullary glands
seminal vesicles prostate gland bulbourethral glands urethral glands secrete serous and mucinous fluids branched tubular to tubulo-acinar glands arranged in lobules |
|
|
seminal vesicle fluid
|
viscous
contains - fructose (providing sperm energy) - prostaglandins (stimulates sperm mobility and enhances viability) - coagulating proteins |
|
|
secretions of the prostate
|
thin and alkaline
enhance motility of sperm may contribute to copulatory plug |
|
|
bulbourethral gland secretions
|
cowpers's glands
alkaline mucus-like fluid neutralizes the acidity of the urine residue in the urethra neutralizes the acidity of the vaginal secretions not present in dog |
|
|
penis
|
adjacent to penile urethra are 3 columns of erectile tissue
- 2 dorsal columns (corpora carernosa - single midline ventral column surrounding the urethra (corpus spongiosum) erectile tissue composed of numerous small vascular sinuses - associated fibrous CT and smooth & striated musc |
|
|
difference b/w fibrous and vascular penice types
|
fibrous
- CT includes elastic fibers & smooth musc extends from dense fibrous CT capsule to cover erectile components - some elastic fibers may be incorporated into the sinusoidal erectile tissue vascular - CT capsule is minimal - erectile tissue (vascular sinuses) well developed and rich in elastic fibers |
|
|
female reproductive tract
|
|
|
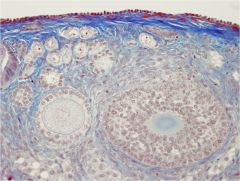
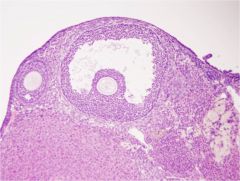
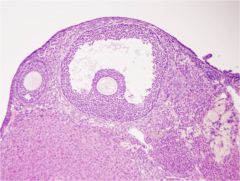
ovary (H&E)
medulla through middle cortex all around secondary and antral follicles |
|
|
ovary (trichrome)
medulla (fibrous CT) through middle cortex around it |
|
|
ovary (medulla)
very vascular b/c makes oocytes/ follicles & makes hormones that need to get into blood stream |
|
|
ovarian cortex
top left - germinal epithelium blue capsule (tunica albugenia) beneath that cortical stroma beneath that bottom left - primary follicle |
|
|
primary follicle
(primary have more cuboidal cells) (primordial have more flattened, squamous cells) |
|
|
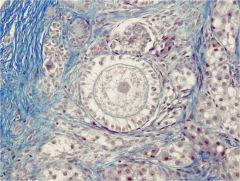
ovarian cortex (trichrome)
primordial follicles up top primary follicles - middle left secondary follicle - bottom right |
|
|
Primary follicle
single layer of cuboidal follicular epithelial cells |
|
|
|
secondary follicle
|
|

|
secondary follicle
|
|

|
Primary Follicle (top right)
Secondary follicles - multiple layers with epithelial cavitary fragmenting |
|
|
Primary Follicle (top right)
Secondary follicles - multiple layers with epithelial cavitary fragmenting stromal CT surrounds & supports |
|
|
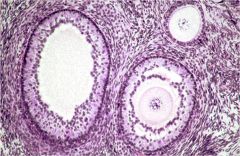
tertiary follicle (antral follicle)
oocyte (corona radiata is the 1st layer of cell surrounding it) zona pellucida cumulus oophoris antral cavity granulosa cells (follicular epithelial cells) thecal cells |
|
|
tertiary follicle (antral follicle)
oocyte (corona radiata is the 1st layer of cell surrounding it) zona pellucida cumulus oophoris antral cavity granulosa cells (follicular epithelial cells) thecal cells |
|
|
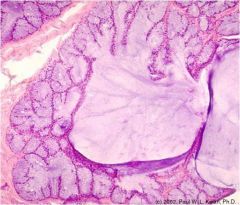
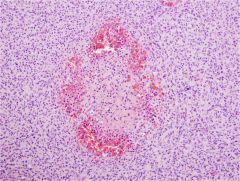
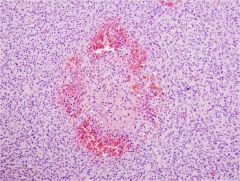
corpora hemorrhagicum
(bloody body) indicates that there was a follicle that ovulated |
|
|
corpora hemorrhagicum
(bloody body) indicates that there was a follicle that ovulated |
|

|
corpora luteum
if everything goes right, preg is maintained & goes to corpora luteum which produces progesterone & estrogen |
|
|
corpora fibrosum
if no pregnancy, rather than expanding to corpora luteum, it continues to collapse to corpora fibrosum |
|
|
corpora fibrosum
if no pregnancy, rather than expanding to corpora luteum, it continues to collapse to corpora fibrosum |
|
|
oviduct
left - muscular wall right - columnar ciliated epithelium (propels egg into uterus) |
|
|
oviduct ampulla region
|
|
|
oviduct
ciliated and peg cells peg cells are more cuboidal, microvilli, secretory |
|

|
oviduct
|
|
|
uterus
outer - perimetrium myometrium stratum vasculare myometrium innermost - endometrium |
|
|
mesometrial attachment (top)
notice stratum vasculare |
|
|
uterus cross section
endometrium at bottom cuboidal to columnar epithelium continuous with glands |
|

|
endometrium
see stroma, glands, surface epithelium |
|

|
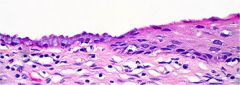
uterine luminal epithelium
some ciliated |
|

|
uterine luminal epithelium
some ciliated |
|
|
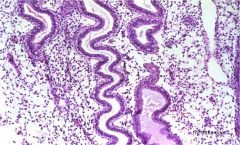
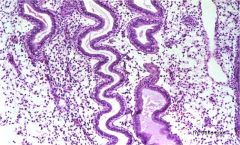
endometrial glands
proestrus to estrus (proliferation of cells, mitotic figures) |
|
|
endometrial glands
metestrus to diestrus (more convoluted forms) |
|
|
endometrial glands
metestrus to diestrus (more convoluted forms) |
|

|
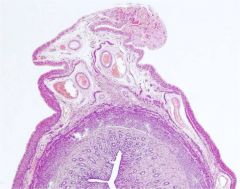
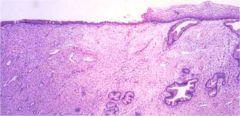
cervix
highly folded (oblique) tubular strx cuboidal mucin cells proximally stratified distally |
|
|
cervix
columnar to stratified epithelium |
|
|
cervix
columnar to stratified epithelium |
|
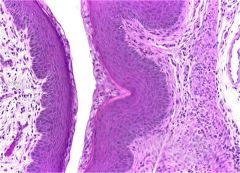
|
cervix
fibrous and muscular wall |
|
|
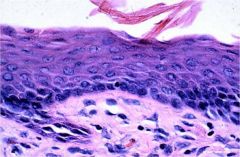
vaginal epithelium
with cornification (keratinization): during estrus |
|
|
_____ is the site of oogenesis
|
ovary
|
|
|
oogenesis is regulated by
|
FSH
- stimulates the follicular epithelium LH - stimulates progesterone production |
|
|
the ovary is composed of
|
germ line cells
epithelial cells supportive stromal cells |
|
|
does the ovary have endocrine or exocrine function
|
both
|
|
|
the ovary is divided into
|
cortex
- composed of follicles, corpora leuta, interstitial stromal cells - aerolar but more cellular with aggregates of pleomorphic fibroblasts medulla - large vessels and nerve fibers supported by areolar connective tissue that is continuous with the mesovarium |
|
|
where are follicles found
|
in the cortex
|
|
|
ovary is covered by
|
squamous epithelium (modified peritoneal mesothelium)
subjacent to surface epithelium is dense fibrous CT that encloses the cortex |
|
|
what stage of follicle is present at birth
|
primordial
- diploid but arrested in meiosis - primary oocyte and scant fluid -single layer squamous epithelium - located in clusters immediately below tunica |
|
|
in what follicular stage does the epithelium begin secreting estrogen
|
primary follicle
- single layer cuboidal cells |
|
|
when do you start seeing theca and membrana granulosa
|
secondary follicle
epithelium becomes stratified - begins to form membrana granulosa rim of a few rows of intersitial cells become epitheloid to form "theca" (cup of follicular cells) increased fluid fragments the epithelium |
|
|
when do you see the oocyst isolated to mound of epithelial cells (cumulus oophorus)
|
tertiary (antral) follicle
|
|
|
when a mature follicle ruptures, wht is released
|
oocyte and corona radiata released into the infundibulum of the oviduct
|
|
|
______ produces progesterone for length of pregnancy
|
corpora luteum
|
|
|
the majority of follicles undergo
|
apoptosis
|
|
|
where do you find fimbria
|
the luminal aspect of the infundibular portion of oviduct
|
|
|
are there glands found in the submucosa of the oviduct?
|
no
|
|
|
muscularis of oviduct
|
inner (longitudinal)
middle (circular) outer (longitudinal) |
|
|
layers of the uterus (which is equivalent to mucosa, serosa, and muscularis)
|
endometrium (mucosa)
myometrium (muscularis) perimetrium (serosa) |
|
|
vestibular portion of vulva
|
includes the clitoris
contains - cavernous vascular tissue - adipose - smooth muscle - surrounded by dense fibrous CT |
|
|
vulvar submucosa
|
stratified squamous
richly innervated |
|
|
cervix luminal surface
|
covered by goblets with some columnar kino-ciliated cells that transitions to stratified squamous epithelium distally
|

