![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
88 Cards in this Set
- Front
- Back
|
4 big risk factors for PERIPHERAL VASCULAR DISEASE (PVD/ PAD/ POAD)
|
DM
smoking HTN hyper-cholesterolaemia/ lipidaemia |
|
|
6 P's for acute limb ischaemia
|
Pulseless
Perishingly cold Pale Paralysis Pain on squeezing Paresthesia |
|
|
Signs of acute limb ischaemia
(POAD inspection: PHU-PAV) |
Pale
Hair loss Ulcers Pigmentation/ gangrene Amputations Varicosities |
|
|
S&Ss of DVT
(remember: may be aysymp) |
unilateral swelling (oedema)
discomfort/ cramp tender (weight-bearing) warmth (rubor), fever discolouration PE pyrexia superficial vein distension |
|
|
Predisposing risk factors for DVT
|
long haul flight
recent trauma / surgery immobility FH cancer obese preg/ the pill smoking |
|
|
how does heart increase O2 supply/ extraction
|
increasing coronary blood flow
|
|
|
3 special coronary adaptations
|
↑capillary density
↑basal blood flow ↑O2 extraction |
|
|
which coronary artery is likely affected in an;
- anterior MI - anterolateral MI - lateral MI |
ant: LAD
ant-lat: LAD & circumflex let: circumflex |
|
|
which coronary arteries likely affected in a;
- posterior MI - inferior MI |
post: post interventricular (of RCA)
inferior: R marginal (other) |
|
|
3 INTRINSIC regulations of coronary blood flow
|
- ↓PCO2 = coronary vasodilatation
- metabolic hyperaemia = ↑O2 extraction - adenosine (from ATP metabolism) = vasodilatation |
|
|
2 EXTRINSIC regulations of coronary blood flow
|
- symp control to heart B2 = vasoDILATATION
- adrenaline (adrenal medulla)--> B2 = coronary vasoDILATATION (a1 = vasoCONSTRICTION to non-vital organs) |
|
|
which sympathetic GPC receptor signals via IP3 to cause smooth muscle vasoconstriction
which GPCR & 2nd messenger does it use |
a1 - Gq - phospholipase C - IP3 - Ca+
|
|
|
which phase in cardiac cycle is coronary blood flow greatest?
what importance does this have in ↑HR |
diastole
↑HR= shorter diastole = ↓perfusion |
|
|
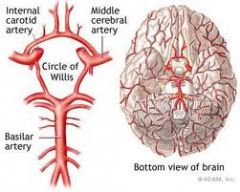
cerebral arteries: which 2 important blood vessels anastemose to form what
|
|
|
|
What protective regulation guards the brain against changes in MAP
|
AUTOREGULATION from MYOGENIC resposne
when MAP ~70-105 |
|
|
what danger does hypercapnia ↑PCO2 pose to the cerebral blood flow
|

↑PCO2 = cerebral vasoDILATATION (overrides autoregulation)
ceretral hyperaemia |
|
|
calc cerebral perfusion pressure (CPP)
what effect does raised ICP have on cerebral blood flow |
CPP= MAP - ICP
↑ICP = ↓CPP |
|
|
concept of BBB
what is the BBB permeable/ impermeable to |
capillaries have highly sensitive, very TIGHT intracellular junction
Permeable: O2 & CO2, glucose (facilitated dif) Impermeable: hydroPHILIC molecules (ions, proteins...) |
|
|
what the resistance in the po circulation like (compared to systemic)
what benefit does this have |
LOW resistance! = ↑flow
ABSORPTIVE forces > filtration (ie protects against po oedema) |
|
|
what the po vascular response to hypoxia and why
|
vasoCONSTRICTION
diverts blood away from poorly ventilated areas |
|
|
difference between ischaemia & infarct
|
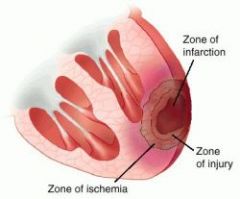
ischaemia: impaired vascular perfusion, reversible
infarct: ischaemic NECROSIS (secondary to ischaemia) reversibility depends on regenerative ability of tissue. |
|
|
compare haemostasis & thrombosis
|
haemostasis is physiological: maintain fluidity of blood & clot where appropriate
thrombosis: PATHOLOGICLA corruption of haemostasis |
|
|
causes of acquired hypercoaguability
(can also be genetic) |
MI, prosethetic heart valves, DIC
Ca immobilisation tissue damage heparin-induced (AF, cardiomyopathy, the pill, preg, smoking, sickle cell anaemia) |
|
|
changes in blood flow (stasis or turbulence) is part of Virchow's triad. How does this pathologically contribute to thrombosis
|
platelets contact endothelium
activated clotting factors activated endothelial cells |
|
|
4 examples of conditions predisposing to changes in blood flow
|
DVT (impaired venous drainage)
AF aneurysm MS (left atrial dilatation) |
|
|
name 3 prothrombotic molecules elaborated by endothelial cells
|
tissue factor
VWF plasminogen activator |
|
|
risk factors causing injury to endothelial cells
|
smoking
hyperlipidaemia toxins HTN vasculitis viruses immune reactions |
|
|
3 types of thrombi
|
arterial
mural (wall of endocardium) venous |
|
|
morphology of an arterial thrombus (appearance)
what are they associated with where are they commonly found |

lines of ZHAN, WHITE thrombus, mainly PLATELETS in a fibrin mesh.
- atherosclerosis - carotid, femoral, cerebral |
|
|
morphology (appearance) of a venous thrombus
|

RED - fibrin-rich, white head
|
|
|
4 fates of a thrombus
|
1) resolution (fibrinolysis)
2) organisation (granulation, recanalisation) 3) propagation/ embolism 4) DIC (clot) |
|
|
6 types of embolism
|
thromboembolism
fat air (can cause PE) tumour amniotic fluid septic |
|
|
80% systemic emboli originate from where
what 3 common reasons |
heart! ♥
- AF, post-MI, aneurysm |
|
|
what's Monvkeberg Medial Calcific Sclerosis
|
calcification of medium sized arteries in >50yrs
|
|
|
differentiate artherosclerosis and arteriosclerosis
|
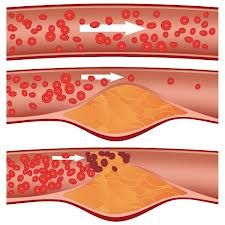
arthero: INTIMAL
arterio: small arteries/ arterioles, hyaline & hyperplastic (DM & HTN) |
|
|
3 main targets for atherosclerosis
|
cerebral arteries
coronary arteries aorta |
|
|
what happens to the walls and linings of arteries in atherosclerosis
|
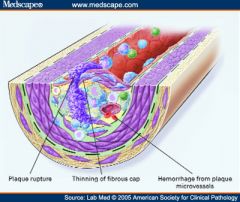
raised focal lesion of intima
media degraded / weakened (aneurysm) lipid core fibrous cap |
|
|
in atherosclerosis, what effecst does lipoprotein oxidation have
|
cytokine & GF release
direct damage endothelial & SM cells ab response trap MACs engulfed by MACs chemotactic |
|
|
what migrates and proliferates within an atheromatous plaque
|

smooth muscle cells
|
|
|
after smooth muscle proliferation and collagen deposition, what does a fatty streak become
|
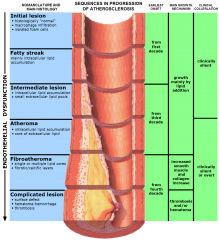
fibrofatty atheroma (plaque)
|
|
|
what 2 syndromes come under acute coronary syndrome (ACS)
|
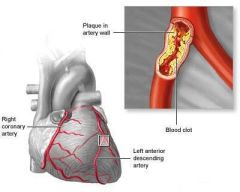
unstable angina
AMI |
|
|
characteristic pain of angina pectoris
|
visceral (myocardial hypoxia): dull, heavy, tight.
predictable retrosternal exertion, cold, heavy meals may radiate <30mins ease at rest / GTN (may be associated with: sweating, nausea, dyspnoea, faint) |
|
|
Ddx's chest pain
|
Gi (reflux, ulcer, biliary colic)
musculoskeletal pericarditis (posture related) Resp- PE, pneumothorax (pleuritic) tumour MI!! dissection |
|
|
3 Ix's for angina (type of CHD/ IHD)
NOT ACS |
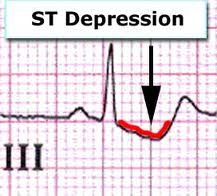
☆ exercise testing☆ (& baseline ECG)
perfusion scanning (thallium) CT coronary ANGIOGRAPHY (high risk) |
|
|
What's the difference betwees CCBs:
- dihydropyradines - rate-liminting eg for each (clinical use) |
Dihydro: amlodipine - act on systemic vascular smooth muscle (HTN)
Rate-limiting: verapamil - myocyte specific (angina) NB: diltiazem is an intermediate |
|
|
first line therapy for stable angina (e.g)
alternative if intolerant |
cardio-selective BBs (e.g. bisiprolol, atenolol)
GTN intolerant: rate-limiting CCB (verapamil), isosorbide mononitrate (long-acting), K-channel opener (nicorandil) |
|
|
2nd line addition to 1st line management (BBs / GTN) of stable angina
|
CCB (dihydropyradine- amlodipine)
NB: rate-limiting CCBs + BBs used with CAUTION! |
|
|
side effects of GTN
|
flushing
light headed headache |
|
|
If angina is due to atherosclerotic (CHD) disease, what 2/3 secondary preventative drugs do you add to:
1st line BB/ GTN 2nd line CCB (dihyd) |
★aspirin★
★statins★ ?ACEI (consider) |
|
|
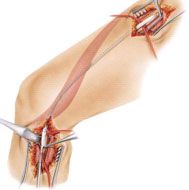
which 2 revascularisation procedures are appropriate for alleviating anginal symptoms
|
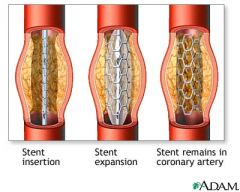
CABG
PCI (percutaneous coronary intervention) |
|
|
which 3 vessels can be used in CABG
|
internal thoracic artery (mammary artery)
radial artery long saphenous vein |
|
|
Indications for CTCA
why (with a veiw to what) |
severe stable angina
unstable angina ACS non-ST elevation ASC ST-elevation treated with throbolytic therapy view to REVASCULARISATION |
|
|
name some medical and haematological conditions that predispose to DVT/PE
|
medical: vasculitis, ca, AMI, CHF, sepsis, nephritis, IBS, ==.
haem: polycythaemia, thrombosytosis, coagulation, antithrombin def, protein C/S def, prothrombin mutation, factor V leiden |
|
|
some medications predisposing to DVT
|
oestrogen
oral contraceptives IVDUs chemo heparin-induces |
|
|
S&Ss of DVT
|

unilateral
calf: pain, red, inflamed, warm, pitting oedema, prominent superficial veins fever |
|
|
Ix's for DVT
|
FBC & U&Es (clotting)
★D dimer ★doppler USS |
|
|
management of DVT
|

anticoagulation: ★LMWH & warfarin★
mobilisation compression stockings |
|
|
management of phlegmasia dolens (severe DVT obstructing arterial flow in POAD) --> venous gangrene
|

EMERGENCY
★IVC filter ★ |
|
|
S&S's of PE
|
tachypnoea, breathless, hypoxia, cyanosis
chest pain haemoptysis collapse tachycardia hypotension ↑JVP, pleural rub |
|
|
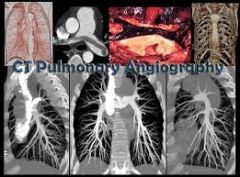
Ix's for PE
|

FBC & U&Es (clotting)
ABG, CXR (effusion, collapse, consolidation, oedema, WEDGE-shaped infarcts) ★CTPA★ ECG/ echo (R heart strain) ?V/Q scan |
|
|
management of PE
|
anti-coagulant: LMWH & warfain
thrombolysis: for major PE (RV dysfunction) IVC filter suspect DVT?- assess |
|
|
anticoagulant, warfarin, is an anti-thrombotic. How does it work?
how is it monitored |
vit K antagonist- blocks ability to activate ALL serine coagulation factors
INR |
|
|
anticoagulant, LMWH, is an anti-thrombotic. How does it work?
|
binds to natural antithrobotic- ATIII to increase affinity and rate of coagulation factor Xa inactivation
|
|
|
2 new direct oral inhibitors
|
direct thrombin (lla) inhib- dabigatran
Xa inhib- fondaparinux |
|
|
egs of some thrombolytic drugs and how they work
|
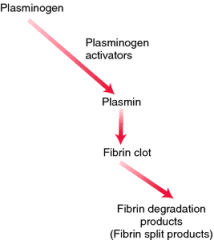
fibrinolytics: tPA, streptokinase.
activate plasminogen --> plasmin which degrades fibrin clots accelerates resolution |
|
|
when are thrombolytics used
|
when PCI for ST-elevation ACS can't be done within 90min
(not often used in VTE) |
|
|
Anticoagulants pose a risk of bleeding- in which pt's in particular
|
DM
renal failure >65 prev stroke GI bleed MI anaemia |
|
|
how do you reverse overdose of warfarin and LMWH
|
warfarin- Vik K/ fresh frozen plasma
LMWH- protamine sulphate |
|
|
2 types stroke & why
|
Haemorrhagic: ⇧BP, weak walls (structural, inflam)
Ischaemic: thrombosis, embolism, hypoperfusion |
|
|
gender and race risk factor for stroke
|
female♀
african-american |
|
|
what common heart abnormality is associated with ⇧ risk stroke
|
AF
|
|
|
Ix's stroke
- general - caused by cardioembolism |
CT +/- angiography
MRI ECG, ECHO |
|
|
medical treatment of stroke
|
ANTIPLATELETS(aspirin, clopidogrel [ADP rec antag], tirofiban [GP rec antag])
THROMBOLYSIS- in emergency statins- preventative anticoagulants- AF antihypertensives- HTN |
|
|
how do you differentiate between peripheral arterial disease and peripheral venous disease
|

arterial: INTERMITTENT CLAUDICATION , ulceration, gangrene
venous: DVT signs, VARICOSE veins |
|
|
2 types of PAD
|

atherosclerotic (obstructive)
aneurysmal |
|
|
major risk factors in PAD
|
male
DM SMOKING HTN age ... |
|
|
S&Ss PAD
|
INTERMITTENT CLAUDICATION, cramping
pain on movement ulceration, gangrene distally --> proximally pale, pulseless, cold, paralysis, paresthesia, loss hair, loss pigmentation, amputations, nail changes bruits |
|
|
Ix's for PAD (& critical limb ischaemia)
|
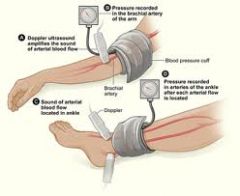
★ANKLE-BRACHIAL PRESSURE INDEX★ (leg BP)
<1 = PAD DUPLEX USS- artery flow (MRA or arteriography) |
|
|
management of claudication/ PAD
|
CONSERVATIVE:
- quit smoking - lose weight - exercise (collateral circulation) - treat underlying HTN, DM, hypercholesterolemia drugs when QOL poor (vasodilators) surgery (angioplasty) |
|
|
what can PAD develop into if untreated- how would you distinguish this clinically
|

CRITICAL limb ischaemia:
- REST pain (wakes at night) - Ulcers - Gangrene |
|
|
what's the GOLD standard treatment for critical limb ischaemia
|
SURGERY / ANGIOPLASTY
treat underlying risks (e.g. DM, HTN, smoking,..) |
|
|
what are varicose veins
|

VENOUS disease- incompetent VALVES
blood deep--> superficial veins (reverse) venous HTN |
|
|
S&Ss of varicose veins
|

dilated veins from venous HTN
pain, cramps, tingling, heaviness oedema, ulcers, tenderness gravitational |
|
|
what's chronic venous insufficiency
if untreated, what can it lead to |

irreversible skin damage from sustained venous HTN
relief on raising --> chronic venous ulceration |
|
|
what's chronic venous ulceration
|

break in skin >6/52 between MALLEOLUS & TIBIAL TUBEROSITY
develops from chronic venous insifficiency |
|
|
Ix's for varicose veins (venous disease)
|
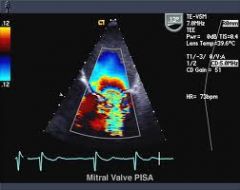
★DOPPLER USS★
|
|
|
management of venous diseases/ varicose veins
|
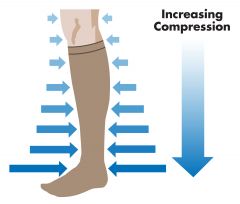
★COMPRESSion stockings★ + pt EDUCATION
ulcers- topical SURGICAL removal SCLEROSANT therapy |
|
|
ddx for ulceration
|

PAD - distally
CVI- malleolus---> tibial tuberosity VASCULITIS- proximal |

