![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
527 Cards in this Set
- Front
- Back
Acute scrotal pain
|
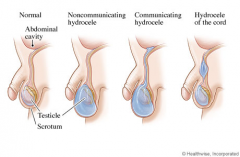
1. pain predominant
testicular torsion: medical emergency need surgical detorsion and orchiopexy(fixation of both testes) cremasteric reflex: positive if there is elevation of the testis in response to stroking the upper inner thigh It is negative in testicular torsion and boys < 6 months Negative cremasteric reflex and abnormal testicle lay are high suggestive of testicular torsion. Doppler U/S or nuclear scan of scrotum can help diagnosis of testicular torsion in the case of clinical uncertainity torsion of the appendix testis epididymitis: pain relief with scrotum elevation, not reliable for diagnosis, U/A is recommended for all suspected epididymitis, urethral swab is recommended for STD induced epididymitis 2. swelling predominant hydrocele: typically not painful positive translumination of scrotum, a cystic scrotal fluid collection between the parietal and visceral layers of the tunica vaginalis that can communicate, increased size during the day and with Valsalva maneuver |
|
|
Varicocele
|
Venous drainage of the testes involves a complex network of veins called the pampiniform plexus, which are responsible for keeping the temperature of the scrotal sacs below the normal body temperature. Seminiferous tubules make up most of the testicular mass, and are very sensitive to an ↑temperature .Dilation of the pampiniform plexus (varicocele) results in an ↑temperature of the scrotal sacs → testicular atrophy
Androgen-secreting Leydig cells are more resistant to an↑ in temperature caused by varicoceles therefore impotence is not common in varicocele. Varicoceles are more common on the left side because the left spermatic vein enters the left renal vein at a 90-degree angle. The right spermatic vein drains at a more obtuse angle directly into the inferior vena cava, thereby facilitating a more continuous flow. Processes that cause IVC obstruction(clot, tumor) should be ruled out in patients who have bilateral varicocele, right varicocles or varicocele that does not disappear in the supine postion (abdominal CT) |
|
|
Scrotal trauma
|
Surgical exploration should be performed immediately in scrotal trauma cases wherein there is evidence of significant trauma (hematoma)on PE.
|
|
|
Sphincter-sparing sugery for patients with rectal cancer
|
An important determining factor is the location of the tumor
Proximal non-metastatic rectal cancer --- lower anterior resection+radiation+chemo if node + Distal rectal cancer ---- local resection(spincter-sparing operation) if mobile, non-ulcerated and relatively small (<4cm) or abdomino-perineal resection (extensive radical operation) Patients with a big tumor are sometimes treated with preoperative irradiation and concurrent chemotherapy prior to a planned resection which may permit a spincter-preserving local resection |
|
|
Fat embolism
|
A clinical diagnosis, 24-72h after severe trauma
Triad: respiratory insufficiency + neurological impairment + petechial rash,(trunk) by occlusion of dermal capillaries by fat globules –extravasation of RBC, the rash is considered pathognomonic Can have fever, tachycardia and altered mental status. Ventilation/perfusion scans may demonstrate a mottled pattern of sub-segmental perfusion defects with a normal ventilatory pattern. Treatment: early immobilization + operative fixation of fractures |
|
|
Acute arterial occlusion
|
usually presents with five Ps: pain, pallor, pulselessness, paresthesias and paralysis. The sudden onset of symptoms in a previously asymptomatic patient is most likely due to an embolus while a history of gradually progressive symptoms in a previously symptomatic patient is consistent with thrombosis
Most of the emboli are from a cardiac source , with a few coming from the arterial aneurysms or atherosclerotic plaques. It is important to find the exact cause of cardiac emboli to prevent further recurrences. After an embolectomy, the surgical specimen should be sent for histological examination to ascertain the exact source of emboli. Atrial myxomas are the most common primary cardiac tumors (LA>RA>LV). The tumors are typically pedunculated with a stalk arising from the atrial septum. These can be extremely friable, resulting in embolization of the part of the myxoma to the systemic circulation. Some large tumors may initially present with signs and symptoms of mitral valve obstruction (diastolic murmur or tumor plop), rapidly worsening heart failure in otherwise young healthy individuals or new onset of AF. Once the diagnosis of atrial myxoma is made, it should be excised as soon as possible to reduce the risk of recurrent embolization |
|
|
Thyroglossal duct cyst
|
1/3 present after the age of 20
Midline neck mass that moves with protrusion of the tongue Have high chances of getting infected due to the connection with the oropharynx Ectopic thyroid tissue is present in a large number of patients within the thyroglossal duct cysts, but sometimes this is the only functional tissue present, so thyroid function assessment + imaging studies like a thyroid nuclear scan, U/S or CT is mandatory before subjecting of the patient to surgery, CT is more useful because it clarifies the anatomy of the thyroglossal duct cyst in relation to the surrounding structures |
|
|
Klinefelter’s syndrome
|
Related to gynecomastia (decreased testosterone-to-estrogen ratio, low testosterone levels→LH increase →increased estrogen)
The strongest known risk factor for male breast cancer, 50-fold increase |
|
|
Anal abscess
|
Glands that encircle the anus become blocked and the bacteria within grow unchecked.
Severe constant pain+/- fever/maaise PE: erythematous indurated skin or fluctuant mass over the peripheral or ischiorectal space Treatment: incision + drainage of the abscess + antibiotics (if DM, immunosuppressive, extensive cellulitis or valvular heart disease) Periana/small ischiorectal abscesses --- office Larger ischiorectal abscesses --- surgical intervention Complication: fistula from the involved anal gland to the overlying skin, require surgical repair (present with an anal abscess that persists after incision and drainage or pustule-like lesion in the perianal or ischiorectal area that conitually drains) |
|
|
Porcelain gallbladder
|
Calcium salt deposits in the wall of a chronically inflamed gallbladder + Thin/faintly visible /amorphous/patchy/thick calcification + Large gallbladder
Associated with gallstones Plain radiography can detect it (abdominal X-ray shows a curvilinear calcification in the right hypochondrium), CT can confirm the diagnosis (high sensitivity and specifity) Treatment: elective cholecystectomy due to high risk of gallbladder carcinoma |
|
|
Stress fracture
|
Common in athletes, ballet dancers, baketbal/soccer players, military recruits
Related to activity (excessive training and improper footwear), biomechanic (weak calf muscles and high arched feet) or metabolism (demineralized bone from hormonal or nutritional disease)Occur due to a sudden increase in repeated tension/compression without adequate rest that eventually breaks the bone Medial tibial stress syndrome (shine splints with no tibial tenderness on palpation) which can progress with further activity to a complete/incomplete fracture → pain to palpation of the tibia The clinical diagnosis of a stress fracture is made on examination with pain at a specific area that increases with jumping or running and is associated with local swelling and point tenderness to palpation. Plain X-ray is < 50% sensitive for stress fracture especially within the first 2-3 weeks after the onset of symptoms (MRI is preferred over bone scan or U/S and can show a fracture line that extends through the cortex into the medullary line and can distinguish ligament, muscle and cartilage injuries but can stay abnormal for up to 12months after the stress fracture) and can take 3-4 weeks or months to show changes of a stress fracture including periosteal elevation, bone sclerosis , true fracture line and cortical thickening. Treatment: conservative treatment(complete cessation of aggravating activities for >4-6w) + pain control + crutch/brace support, gradual return to activity |
|
|
Bile salt-induced diarrhea
|
Complication in 5-10% of cholecysterectomies, It is usually seen in short bowel syndrome as well.
Choleycysterectomy → increased bile acid flux to the colon → a shift to the secondary bile acids → diarrhea Treatment: cholestyramine (bile-acid binding resin, sequester the excess bile acids) |
|
Breast cysts
|
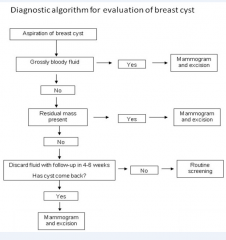
In patients > 30y, breast masses should first be evaluated by mammogram and/or U/S.
Simple cysts are well-circumscribed on U/S, thin→thick consistency with varying color, disapper with aspiration of the fluid. Unless blood is seen in the aspirate, no further intervention is required initially except for serial U/S. Complex cysts have thick walls on U/S and may contain both cystic and solid components. Require core needle biopsy. Solid, circumscribed masses usually represent fibroadenomas and can be followed with repeat U/S and mammogram in 6m but patients generally request biopsy for confirmation |
|
|
Indirect hernias
|
in the pediatric age group should be surgically repaired as early as possible. Will not resolve with age. It is related to the failure of the processus vaginalis to obliterate (A direct hernia related to muscular weakness of the abdominal wall is usually seen in the elderly age group)
The risk of potential complications including incarceration is particularly high if it remains unrepaired during the first months of life. |
|
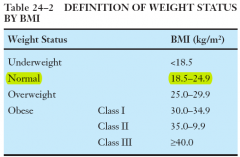
Significant obesity
|
(BMI>35kg/m2) with comorbid conditions (premature osteoarthritis, HTN, DM) should be managed aggressively for weight loss with dietary changes, behavioral therapy and medical therapy (orlistat) if conservative treatment fails. Patients who fail both conservative and medical therapies should be considered for bariatric surgery.
Indication for bariatric surgery (gastric bypass or vertical banded gastroplasty, gallbladder disease is a common complication of bariatric surgery and rapid weight loss) 1. BMI > 40 who have a low risk for surgery and failed previous weight loss treatments or 2. BMI >35 who have obesity-related comorbidities Referral to plastic surgery presumably for lipectomy, should take place only after bariatric surgery has been completed and long-term weight loss has been achieved. |
|
|
Scaphoid fracture
|
are the most common carpal bone fracture and occur while falling on an outstretched hand with a dorsiflexed wrist (The scaphoid spans both the proximal and distal carpal row. In this position it is quite vulnerable to high-impact injuries, such as a fall on an outstretched hand, and is the most commonly fractured carpal bone.).
↓Range of motion in the wrist + point tenderness over the radial aspect of the wrist/ the scaphoid within the anatomic snuffbox (snuffbox tenderness)+ ↓grip strength It can take up to 2weeks to show the fracture in X-ray. The current guidelines recommend MRI or CT of the wirst to distinguish between fracture and ligament injuries. Patients should be referred to an orthopedic surgeon if they have a scaphoid fracture displaced >1mm, association with tilf of the lunate, nonunion during follow-up, osteonecrosis or scapholunate dissociation. If not meet surgical indications and have a nondisplaced fracture should be placed in a short-arm thumb spica cast (with wrist deviated radially and neutrally flexed) and have follow-up X-rays every 2 weeks to monitor healing. Immobilization should be continued until there is radiographic union. Scaphoid fractures are most commonly complicated by nonunion骨折不愈合 and avascular necrosis (proximal fractures of the scaphoid has less blood supply and require longer immobilization, 12weeks for adequate healing,) Malunion骨连接不正is more commonly seen in physeal fractures of the distal forearm in children due to injury of the growth plate and growth arrest → a growth disparity between the radius and ulna wrist deformity DD 1. Colles fracture: occurs after a blow to the wrist while falling on an outstretched hand and has the appearance of a dinner fork on lateral view of the wrist due to the ulnar styloid separating from the rest of the bone (A Colles fracture is a fracture of the distal radius at the metaphysis, which is displaced dorsally and often angulated. It is the most common wrist fracture in adults. The ulnar styloid is often involved, and there may be intraarticular involvement as well.) 1. Hamate fracture: occur while falling on an outstretched hand, near the hook of the hamate containing the ulnar artery and nerve, pain/swelling in the hypothenar eminence and ulnar aspect of the wrist 2. Radial styloid fracture (Hutchingson /chauffeur fracture) occurs due to a direct blow to the styloid while falling on an outstretched hand with ulnar deviation and supination – a fracture dislocation of the radial styloid and either lunate or scaphoid 1. Wrist sprain of the ligaments: mild pain/stiffness with normal range of motion, resolve with conservative/supportive care. Worse pain with flexion and extension of the ligaments rather then severe point tenderness with palpation |
|
Stop the raloxifene
|
4 weeks prior to surgery and restart it postoperatively when the patient is stable with ↓risk for thromoboembolism (Raloxifene →↑thromoboembolism, but not ↑endometrial carcinoma , can prevent osteoporosis)
|
|
|
Desmoid tumor 纤维瘤
|
A locally aggressive benign tumor arising from fibroplastic elements within the muscle or fascial planes with very low potential for metastasis/differentiation due to abnormal wound healing or clonal chromosomal abnormalities causing a neoplastic behavior, has variable clinical course.
Rare but increased in familial adenomatosis polyposis (Gardner syndrome) Typically present as deeply seated painless/painful masses in the trunk/extremity, intraabdominal bowel and mesentery and abdominal wall. They can cause intestinal obstruction and bowel ischemia and have a high rate of recurrence even after aggressive surgery Treatment: surgery or radiation DD 1. Dermatofibroma A benign proliferation of fibroblasts that usually occurs after trauma or insect bite or idiopathic, a firm hyperpigmented nodule located on the lower extremities rather than the abdomen 2. Epidermoid像表皮的cyst A discrete nodule that is usually located on the skin and a result of the normal epidermal keratin becoming lodged in the dermis. It can be seen in Gardner syndrome but are usually located on the extremities, can resolve spontaneously without treatment 3. Lipoma An asymptomatic and benign subcutaneous collection of fat cells. Soft without rapid enlargement or recurrence after resection. 4 Pyogenic granuloma (granuloma telangiectaticum) Caused by capillary proliferation after trauma Dome-shaped papule with recurrent bleeding, more commonly seen in pregnant women In digital injuries, tendons are more likely to be injured than arteries, veins or nerves due to their relative, vulnerable anatomic location. Digital arteries, nerves and veins run on the sides while the flexor tendons run on the anterior surface of the phalanges. Attempting to grab a knife with a hand is likely to injure the tendons. |
|
Tetanus prophylaxis
|
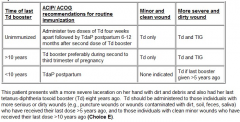
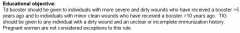
Only tetanus toxoid (booster every 10 years) is given when
1. clean wound +unknown immunization status/<3 does of tetanus antitoxin 2. clean wound+ >3 does of tetanus antitoxin but the last doe was >10y ago 3. contaminated wound + >3 does of tetanus antitoxin but the last doe was >5y ago Tetanus immune globulin should be given to any individual with a dirty wound + an unclear/insufficient immunization history. |
|
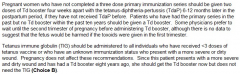
Tetanus prophylaxis
|
For pregnant women
Not indicated: 1. minor/clean wound, vaccine <10y 2. Dirty wound, wound vaccine <5y Td+TIG: dirty wound, immunization unknown or >10y |
|
|
Acute cholangitis 胆道炎
|
Charcot’s triad: right upper quadrant pain+ fever+jaundice (50-75%)
↑Direct bilirubin+↑ alkaline phosphatase without↑ in the ALT/AST →extrahepatic obstruction ERCP should be done in patients with suspected common bile duct stones Treatment: adequate hydration Strict vital signs monitoring Blood culture +immediate antibiotics (empiric: ampicillin+gentamicin or monotherapy with imipenem or levofloxacin) Adequate analgesia, NPO 80% cases get controlled within 24h, if the patient clinically improves, an elective ERCP can be scheduled. But when not improve, urgent biliary decompression through biliary drainage through ERCP with lower morbidity rate of 10% compared with 50% morbidity rate via surgical drainage Cholecystectomy is for treatment of gallstones or acute/chronic cholecystitis not acute cholangits. When hypotension and confusion develop: 50% mortality |
|
|
Acute cholecystitis胆囊炎
|
Right upper quadrant pain (radiate to back/right shoulder)+fever+leukocytosis
Murphy’s sign + Can due to gallstone or acalculus cholecystitis in elderly/critically ill patients U/S initial test for diagnosis (95% sensitivity): stones in the gall bladder/cystic duct, gallbladder wall thickening, pericholecystic fluid collection and + sonographic Murphy’s sign HIDA scan is useful in excluding cystic duct obstruction in patients with clinical features suggestive of acute cholecystitis In patients with uncomplicated acute cholecystitis , the symptoms subside in 7-10d, however if left untreated, there is high risk of complication Compication: gallbladder gangrene/perforation, cholecystoenteric fistula, emphysematous cholecystitis, therefore all patients with acute cholecystitis should be admitted to the hospital and managed with supportive care in the first 24-48 hours Treatment: Adequate analgesia, NPO adequate hydration correction of electrolyte abnormalities antibiotics(empiric: ampicillin-sulbactam or piperacillin-tazobactam or ceftriaxone+metronidazole) Emergent laparotomy/laparoscopic cholecysterectomy/T tube placement(percutaneous cholecystostomy) is only considered for patients with gallbladder gangrene or perforation or fail to respond |
|
|
Flail chest
|
Tachypnea, shallow breathing, tachycardia, anterior chest bruises and peripheral cyanosis
The result of double rib fractures in more than one site Increased work of breathing due to muscular spasm and pain. Hypoxia develops frequently due to associated pulmonary contusions |
|
|
Anterior cruciate ligament (ACL)
|
Athelete, occur after hyperextension of the knee, popping sensation, rapid onset of a knee effusion and an unstable knee
Lachman’s test is very sensitive 80-95% (knee flexed at 20 degrees, supine, one hand pulls the proxima tibia while the other hand stabilizes the femur) Pop or swelling 0-12h after the injury or hemarthrosis on aspiration suspect ACL |
|
|
Meniscal injury
|
After a twistering injury, medical meniscus injury more common
Locking of the knee joint on extensions, tenderness along medical side of the knee McMurray’s sign: snap felt with tibial torsion and the knee flexed at 90 degrees |
|
|
Dashboard injury
|
A posteriorly directed force is placed on the anterior aspect of the proximal tibia, with the knee in a flexed position—disruption of the posteror cruciate ligament.
A similar injury can be seen in an athlete who falls on a flexed knee with the foot in plantar flexion. |
|
|
Patellar tendon rupture
|
Excruciating pain + swelling in the anterior part of the knee + inability to maintain passive extension of the knee against gravity
Treatment: early surgical repair of the ruptured patellar tendon, delayed treatment can lead to quadriceps muscle atrophy, contracture formation and limited range of motion of the knee →significant disability DD 1. Anterior cruciate ligament tear (ACL) Popping sensation/sound at the time of injury Anterior drawer test +: A difference of 1cm compared with the opposite side suggests a complete tear of the ACL Lachman test is most sensitive for ACL insufficiency (80-95%) 2. Meniscal injury A twisting force with the foot fixed on the ground, commonly seen during football/basketball games, McMurray’s maneuver + with an audible /palpable click or popping sensation during extension of the involved knee 3. Medial collateral ligament injury Tenderness/pain along the medial joint line. \ It is most frequently caused by an injury involving valgus (abductor) stress to the partially flexed knee with the foot fixed. Such injury can occur while skiing or during contact sports when another person falls across the knee from the lateral to medial direction Did the patient or someone else hear a pop? If yes, suspect ACL tear (80%), meniscal injury (15%), and rarely a fracture. When did you notice swelling? If 0–12 hours after the injury, suspect ACL tear or patellar dislocation/subluxation; if 12–24 hours, suspect meniscal injury. If there is hemarthrosis on aspiration, suspect ACL injury (>75%), patellar subluxation, or intraarticular fracture |
|
|
Elevated intracranial pressure
|
Cushing’s triad: bradycardia, HTN, respiratory depression
Headache, vomiting, blurred vision, papilledema on funduscopic examination→ transtentorial herniation of brain tissue altered levels of consciousness (stupor progressing to coma), dilation of the ipsilateral pupil, CNIII palsy, hemiparesis, decerebrate posturing, respiratory arrest Most important next step: rapidly intubate the patient to protect /maintain airway in case of b respiratory arrest |
|
Diabetic antonomic neuropathy
|
Distal symmetric polyneuropathy (stocking-glovepattern), erectile dysfunction, diminished testicular sensation, bladder dysfunction, inability to masturbate
DD 1. cauda equine syndrome: severe lower back pain, urinary/bowel incontinence, motor weakness /sensory loss in the legs bilaterally, saddle anesthesia 2. Injury to the spinal cord at L1-L2: The cremateric reflex is regulated at the L1-L2 level of the spinal cord., The reflex can be diminished or lost secondary to diabetic antonomic neuropathy. L1-L2 also responsible for hip flexion and adduction. 3. Injury to the spinal cord at S2-S4: abnormal anal sphincter tone, responsible for erection and sensation of penile/anal zones (stroke on labia阴唇/clitoris阴蒂→ contraction of anal sphincter) 4. Injury to the spinal cord at L5-S2: abnormal dorsiflextion and plantar flextion |
|
|
Cryptorchidism (undescended testis)
|
4% newborn infants, majority cases resolve spontaneously during the first several months of life (rare after 6 months). Early orchiopexy (6m-2y) helps to prevent testicular torsion/infertility. Although the risk of malignant transformation may ↓ a little after the surgery, it remains higher than that of the general population.
|
|
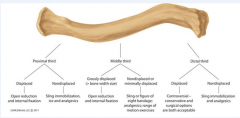
Clavicular fracture
|
Majority occur in the middle third of this S-shaped bone, its thinnest part. In a displaced fracture, the proximal (medial) segment may move superiorly and the distal(lateral) segment inferiorly past each other→ shortening of the bone. The skin over the clavicle may also be stretched → skin necrosis/hematoma/conversion to an open fracture
Surgical referral for open reduction with internal fixation (ORIF) is indicated for 1. open fractures with neurovascular injury or tenting隆起 of the skin 2. widely displaced fractures(> bone width size) 3. Significant shortening and comminution Nondisplaced/minimally displaced fractures of the middle third of the clavicle are usually managed conservatively with ice, analgesics (NASIDs should be avoided as they may delay bone healing, acetaminophen/opioids are perfereed), elbow range of motion exercises and either a sling or figure of eight bandage. The figure of eight bandage requires periodic adjustments to keep it tight and excess tightening risks complications. Most patients prefer a sling over a figure of eight bandage. However the sling does not allow the patient to have complete freedome of the elbow and hands for daily activities → elbow stiffness For the noncontact athlete with a clavicle fracture, a gradual return to usual activities may be allowed in 4-6 weeks after injury when the patient has 1) painless, full, active range of motion, 2) near-normal strength and 3) evidence of bridging callus |
|
|
Hip fracture
|
1. Intracapsular (femoral head and neck) hip fracture:
pain without significant ecchymoses, higher complication of avascular necrosis 2. Extracapsular (intertrochanteric/subtrochanteric) hip fracture: with ecchymoses+external rotation,higher risk for displacement , Both type should be evaluated by an orthopedic surgeon because most of them require surgical correction with either arthroplasty or open reduction with internal fixation. Nonoperative management is reserved for patients who are nonambulatory or demented with mild pain, at the end stage of a terminal illness, have an old nondisplaced /impacted嵌入的fracture or are unable with major comorbitities |
|
|
Prostate cancer
|
1. Transient ↑of PSA level can occur due to a variety of causes (such as urinary retention, BPH, prostate cancer, prostatic inflammation/infection, perineal trauma such as digital rectal examination or prostate massage or cystoscopy ) that usually ↓4-6w after recovery from the insult. Further investigation is needed if the PSA level remains↑or prostate examination shows abnormal finding
2. Transrectal biopsy of the prostate is invasive and indicated for patients with prostate nodules, induration or asymmetry on rectal examination +/- ↑PSA level |
|
|
Femoral nerve injury
|
Inability to extend the knee, sparing leg adduction(obturator nerve)
Loss of knee jerk reflex Sensory loss: the anterior/medial aspects of the thigh+medial aspect of the shin+ arch of the foot DD 1. Obturator nerve injury (pelvic trauma/injury) Pain, weakness in leg adduction Sensory loss over a small area in the medial thigh 2. Sciatic nerve injury (trauma, hip dislocation/fracture/replacement, wayward不规则的 buttock injections, prolonged bed rest, deep-seated mass in the pelvis due to hematoma) Weakness affecting most of the lower leg musculature including hamstrings腿筋, hip flexion/abduction/adduction Ankle jerk is unobtainable 3. Common peroneal nerve injury (injury at the knee/lateral aspect of the fibular head) Acute foot drop+weekness in foot dorsiflextion/eversion Paresthesia/sensory loss over the dorsum of the foot+laternal shin (superficial peroneal nerve territory) |
|
|
An upright chest X-ray
|
is the initial test of choice to confirm the diagnosis of penumothorax. The accumulation of air occurs primarily in the apical and lateral regions when the patient is upright and is usually seen as a convex white visceral pleural line on X-ray. As little as 50ml of pleural gas can be visible on upright X-ray.
|
|
|
Morphine
|
undergoes a 2-step metabolism process, beginning with hepatic conjugation with glucuronic acid to form active metabolites morphine-3-glucuronide and morphine-6-glucuronide which is more potent than morphine. The metabolites are then eliminated by the kidney. In the setting of renal injury, morphine-6-glucurnoide accumulates and potentiates the effects of morphine.
Morphine acts directly on brainstem respiratory centers to produce respiratory depression and also the sensitivity of medullary chemoreceptors to CO2 levels, leaving only the hypoxic drive functioning. Giving a patient O2 → apnea by removing both respiratory drives and further worsening the respiratory depression. Clinical triad of depressed respiratory function which is consistent with acute opioid toxicity: ↓respiratory function + small pupils + drowsiness/coma Maintenance of adequate hemodynamic stability is the most important step in the management of a patient with a penetrating injury. Always attempt to identify and correct any reversible cause of coagulopathy and anticipate the need for blood transfusions in such patients (knife penetrating injury to skull): blood typing + corssmatch +PT/PTT U/S is the initial test of choice to evaluate a testicular mass and to differentiate between solid and cystic masses. |
|
|
Retrograde ejaculation
|
is the most frequent complication of transurethral resection of the prostate (TURP), which is an invasive procedure used in the management of benign prostatic hyperplasia (BPH.).
|
|
|
Silicone breast implants
|
do not cause any major rheumatologic autoimmune or neurologic disorder. Most morbidity from silicone breast implants is associated with local complications such as capsular contracture, implant deflation and rupture. There is no evidence that having silicone breast implants causes any harmful effects, such as birth defects or any other neurological abnormalities on the developing fetus. There is no risk in breast-feeding with a silicone breast implant. Women with breast implants should continue to have screening mammograms at regular intervals. It is recommended MRI imagining every 2 or 3y over the lifetime of the implant to screen for asymptomatic implant rupture → scarring within the breast.
|
|
|
The Achilles (calcaneal) tendon rupture
|
Thrompson test with 96% sensitivity and 93% specifity: the patient lying in the prone position, feet hanging off the table, the clinician squeeze the patient’s calf muscles and observe for the presence of plantar flexion of the foot., The absence of plantar flexion signifies complete rupture and a positive test result.
Absence of active plantar flextion is not as reliable as the calf-squeeze test to rule out Achilles tendon rupture because patient can also use accessory muscles to actively plantar flex and falsely reassure the clinician. MRI is the diagnostic modality of choice for Achilles tendon rupture and useful in the setting of high clinical suspicion with (-) Thompson test or if the Achilles tendon tear is suspected. |
|
|
Peripheral vascular disease
|
Ankle-brachial pressure index (ABI) is the best initial screening test to detect peripheral vascular disease. It is calculated by measuring the systolic blood pressure using a Doppler probe at the brachial, posterior tibial and dorsalis pedis arteries and then dividing the lower extremity pressure by the brachial pressure.
Normal: 1-1.3 ABI < 0.9 --- peripheral vascular disease ABI < 0.4 –- severe ischemia Cliostrzol is currently the most effective conservative therapy available for peripheral vascular disease. Cilostazol is a phosphodiesterase inhibitor that inhibit platelet aggregation and acts as a direct arterial vasodilator. It can be taken in combination with aspirin and clopidogrel. |
|
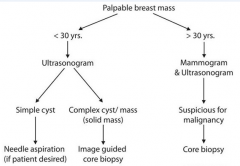
A mammogram
|
is not as sensitive or specific for initial evaluation for women <30y because the breast tissue is usually denser in this age group. A U/S has better sensitivity and specifity for initial evaluation.
Core needle biopsy is a larger sample of the breast and more deforming but can test for ER, PR AND HER2/neu ( Fine needle aspiration can not). |
|
|
Mesenteric ischemia
|
Acute onset of severe abdominal pain+ unmatched PE with the severity of pain + metabolic acidosis is generally mesenteric ischemia unless proven otherwise.
Leukocytes, Hb, serum amylase, LDH , creatine phosphokinase or alkaline phosphatase can be ↑ in mesenteric ischemia The most commone cause is superior mesenteric artery(SMA) occlusion secondary to an embolism. SMA runs off at a minimla angle from the aorta and has a wide diameter. Risk factors are cardiac arrhythmia, recent MI and abdominal malignance. 60% mortaility rate (untreated mesenteric ischemia → bowel infarction, sepsis and death) |
|
|
Cardiac arrest
|
due to lightening injuries usually present with asystole and should be treated with prompt and sometimes prolonged cardiopulmonary resuscitation.
Defibrillation is effective for ventricular fibrillation and pulseess ventricular tachycardia but not aystole. Epinephrine and then atropine should be given for asystole. The most common injuries from lightning include cardiac(sudden cardiac arrest), renal (rhabdomyolysis), nervous system (autonomic dysfunction → fixed/dilated pupils, ruptured eardrum and vitreous hemorrhage) and skin (thermal burn) |
|
|
iv nutrition
|
Numerous complications can occur from iv nutrition in critically ill patients. The most dangerous metabolic complication, hyperglycemia, is most commonly caused by too rapid initiation of the infusion. It is best prevented by initiation of the infusion at 40-60cc/hour, and slowly increasing the rate at 20 cc/hour every 24 hours, while monitoring the patient’s glucose level. Patients with normal glucose intolerance may manifest glycosuria for the first 48hours of parenteral nutrition. Before initiating insulin, one must verify that the glucose level is high and that glycosuria is not secondary to a reduced threshold for glucose.
The most common cause of sudden hyperglycemia is sepsis and hyperglycemia may antedate other signs of sepsis within 24 hours. The sudden appearance of hyperglycemia should initiate a thorough search for the source of infection. |
|
|
Dumping
|
Dumping is a common complication of gastrectomy: abdominal pain + diarrhear+ N/V+dizziness, generalized sweating, dyspnea
Treat: a high protein diet, low in carbohydrate Fractionated, smaller, more frequent foot portions |
|
|
pylephlebitis (infectious thrombosis of the portal veins) 门静脉炎.
|
14% of pregnant women in the 2nd trimester can have premature delivery when affected by appendicitis while around 33% of those in the 1st trimester may experience abortion. During the third trimester the main complication is appendix perforation with peritonitis and subsequent pylephlebitis (infectious thrombosis of the portal veins) 门静脉炎. These complications are rare but feasible, especially if therapy is not offered within the first 24 hours of the initiation of symptoms)
|
|
|
Endoscopic Ultrasound
|
(EUS, use endoscope to take U/S deep in the body) with aspiration is the best test to evaluate a pancreatic cyst to differentiate malignancy from nonmalignant causes.
EUS uses U/S guidance of the endoscope for needle biopsy or lesions too small to be identified by CT/MRI or that are encased by vascular structures(making percuteneous biopsy difficult) Pancreatic cystic neoplasm account for 50% of pancreatic cysts and can be asymptomatic. |
|
|
sudden death after a steering wheel
|
The most common cause of sudden death after a steering wheel injury from motor vehicle accident is aortic injury. Patients typically die at the scene before an ambulance service arrives. Rapid deceleration produces a shearing force along the aortic arch where the aorta is firmly attached. It is usually observed in the area of the ligamentum arteriosum, the aortic root and the diaphragmatic hiatus.
|
|
|
Renal/urethral stones
|
Sudden onset of pain (colicky, wax and wane)+ hematuria
Upper ureteral /renal stones→ pain in the flank Lower/distal ureteral stone→ pain radiating to the ipsilateral groin area Initial treatment: iv hydration, pain control < 5mm , stone pass spontaneously >8-10mm stone or persistent pain, acurte renal failure or signs of urosepsis require removal (1. extracorporeal shockwave lithotripsy-ESWL 2. flexible ureteroscopy 3. percutaneous ureterolithotomy) The choice of procedure depends on the location of the ureteral stone. Shockwave冲击波lithotripsy is the treatment of choice for small symptomatic proximal ureteral calculi(<10mm in size) Flexible ureteroscopy输尿管镜检查术+laser lithotripsy is preferred for large proximal ureteral stones A percutaneous ureterolithotomy输尿管石切除术is only used when shockwave lithotripsy and ureteroscopic removal fail to remove the ureteral stones. |
|
|
animal bites
|
All animal bites, regardless of the site, should be thoroughly cleaned and irrigated with normal saline, and all devitalized tissues should be debrided. A plain radiograph should be obtained if a patient is suspected of having a foreign body or has a bite occurring close to a bone. Most open lacerations can be closed primarily within a few hours of injury. This is especially true for injuries of the face where infections are less common due to a good vascular supply, however bites involving the hands should not be sutured or closed primarily due a high risk of subsequent wound infection. These should be left open to drain and examined frequently for signs of infection. Other situations where primary closure is not recommended include puncture wounds, cat and human bites (high risk of infection), and patients presenting late after the bite.
|
|
|
Human bite
|
Soft tissue or wound infections can occur after a human bite due to exposure to human mouth microbes. Human bites are more serious than animal bites and can be limb threatening. Most of the soft tissue infections caused by human bites are polymircrobial in nature. Infections with human bites are associated with alpha-hemolytic strep, staph aureus, Eikenella corrodens, Haemophilus species and anaerobic bacteria (bacteroides species, Peptostrptococcus, Aactinomyces species and fusobacterium.)
Tx: ampicillin-sulbactam is the drug of choice |
|
|
Complex regional pain syndrome (CRPS)
|
should be suspected in patients with recent joint injury who present with local burning pain (out of proportion to the injury), edema, skin changes and ↓range of motion., temperature change, edema and abnormal skin color. Type I CRPS (90% of CRPS cases) occurs without a definable nerve lesion while type II occurs with a definable nerve lesion. The pathogenesis is likely due to an injury causing ↑sensitivity to sympathetic nerves, an abnormal response to and sensation of pain, and ↑neuropeptide release causing burning pain to light touch (allodynia 异常性疼痛).
Typically, CRPS occurs in 3 stages, Stage 1 includes burning pain, edema and vasomotor changes in a limb after injury. Stage 2 includes progression of edema, skin thickening and muscle wasting. Stage 3 is the most severe and includes limited range of motion and bone demineralization on X-ray. Diagnosis can be confirmed by either autonomic testing that measures↑resting sweat output or MRI that looks for the above changes. Treatment: regional sympathetic nerve block/iv regional anesthesia. |
|
|
Varicose veins
|
visible, palpable and tortuous superficial veins of the legs. Most are asymptomatic. Some may complain of leg cramping, heaviness, fatigue and swelling. The symptoms are generally worse in the evening with prolonged standing and improve with leg elevation.
1. conservative measures: leg elevation, weight reduction and ↓venous pressure in the lower extremities by direct compression (compression stocking should not be used in arterial insufficiency) 2. Injection sclerotherapy (sclerotherapy → endothelial damage + sclerosis of the involved vein→ prevent further vein filling) for patients with symptomatic, small, varicose veins who have failed at least 3-6 months of conservative treatment. 3. surgical ligation + stripping : large symptomatic varicose veins + ulcers, bleeding, recurrent thrombophlebitis of the veins. external laser treatment: particular veins and/or telangiectasia , not for varicose |
|
blunt cardiac injury (BCI)
|
Patients with BCI can have varying degrees of severity including transient dysrhythmias, cardiac wall motion abnormalities, cardiogenic shock and free wall rupture. Cardiac contusion is the most common injury.
The first step after initial stabilization of the patient is to do a chest x-ray to evaluate for fractures, pneumothorax, hemothorax and widened mediastinum indicating possible aortic injury. A patient can either be asymptomatic or manifest various symptoms of cardiac injury ranging from mild chest pain (dull or pressure-like pain) to severe heart failure and cardiovascular collapse. If the chest x-ray is abnormal or the patient is hypotensive, further testing by focused assessment with sonography in trauma (FAST) examination or CT scan of the chest can be done to evaluate for aortic injuries or hemopericardium心包积血. All patients should have a 12-lead ECG especially if there is anterior chest trauma(bruise), are elderly or have a h/o coronary artery disease. 12-lead ECG is the single most important screening test for BCI. Patients with possible BCI and normal ECG require no further treatment or investigation. Abnormal ECG in CBI include a new bundle branch block, persistent sinus tachycardia, ST depression or elevations and other arrhythmias.An individual who suffers severe traumatic injury should be given narcotics for pain relief, regardless of addiction history |
|
Low-molecular-weight heparin or fondaparinux
|
(first-line) is considered the prophylactic therapy of choice for preventing deep vein thrombosis in patients with hip fracture and should be started on admission (DVP may begin at the time of fracture and subsequent bed rest ), even if the patient is scheduled for surgery. This can be stopped 12hours before surgery.
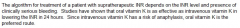
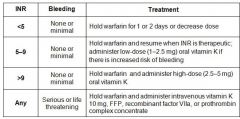
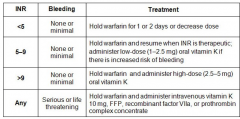
Both of these are short-acting agents and have been shown to have relatively low perioperative bleeding risk while significantly lowering the risk of DVT. Anticoagulation should be continued for >10days (up to 35 days) after surgery, depending the patient’s risks for thrombosis. Warfarin is considered a second-line prophylactic agent that can be started postoperatively since it is long-acting agent, with a target INR of 2.5 ****INR goals for mechanical prosthetic valves ***In contrast to pt with idiopathic DVTs, patients with DVTs secondary to reversible or time-limited risk factors (surgery, pregnancy, OCPs or trauma) should be treated for > 3m but not >6m, as the risk of a recurrent DVT after 6m of treatment is very low. In pt with idiopathic DVTs, >6m of warfarin therapy is also recommended, with re-evaluation at the end of treatment cycle for long-term anticoagulation. |
|
Supratherapeutic INR
|
|
|
|
Inadequate anticoagulation
|
The goal INR level for pt with DVT is 2-3. If INR is 1.4 (under-anticoagulation), it should not be considered a failure of anticoagulation, as the pt was never adequately anticoagulated in the first place. The pt should be admitted to begin iv heparin therapy and will need an increase in his warfarin dose to reach an appropriate INR level.
|
|
|
Pulmonary contusion
|
is the most common lung parenchymal实质 injury seen in patients with blunt chest trauma. Chest radiography generally reveals homogenous opacification of the lung fields that do not conform to a specific anatomic segment of the lung.
Dyspnea, tachypnea, hypoxemia and hemptysis. PE: ↓breath sounds over the affected area of the lungs. It may take several hours for clinical and radiographic abnormalities to develop after the initial trauma. Patients are at risk for late clinical deterioration. Treatment: mainly supportive (oxygen, pain control, careful fluid management to prevent worsening edema in the injured lung), resolution of symptoms generally occurs in 3-5 days. Admitted to the hospital after the initial injury and monitored for 24-48h for any signs of clinical deterioration. |
|
|
Epidural abscess
|
abscess is a possible complication of epidural injections that causes cauda equine syndrome, which is a medical emergency requiring prompt diagnosis with MRI.
The first priority is to establish the diagnosis and determine the extent of damage to the cauda equine because paralysis if present can become irreversible without rapid treatment. Treatment: antibiotics, neurosurgical evaluation for drainage and spine stabilization. If MRI confirms the diagnosis of an epidural abscess, then the next stop would be blood cultures, antibiotics and CT-guided drainage, Lumbar puncture is not recommended for diagnosis because diagnostic yield is low. Surgical decompression by orthopedics or neurosurgery and drainage of the abscess within the first 24h significantly improve the prognosis. High dose gluococorticord is not indicated for epidural abscess.(it is treatment of choice for metastatic malignancy or traumatic injury causing spinal cord compression or cauda equine syndrome ) |
|
|
The sesitiity of a melanoma
|
The sesitiity of a melanoma diagnosis by a dermatologist based on H&P is 85%, an excisional biopsy is essential for confirmation of the diagnosis and staging of the lesion. Complete excision is the treatment of choice.
Common techniques used to remove tattoo marks Dermabrasion (removal of the superficial layer of the epidermis, allowing the pigment to leach out of the skin) Cryosurgery Thermal cautery Surgical resection Laser removal (laser break up the pigments into smaller molecules, which are taken up and cleared by the macrophages in the skin, can leave scar marks→skin hypo/hyper-pigmentation) |
|
|
Rosacea
|
Rosacea is a chronic acneiform condition characterized by vascular dilation in the central face. 30-60y, occurs more often in individuals with light skin, hair and eye color. Periods of exacerbation and remission are expected. It is associated with Meibomian gland dysfunction and chalazion 睑板腺囊肿
Facial erythema, telangiectasia, papules and pustules Treatment: topical metronidazole +/- oral antibiotics (↓number/severity of the inflammatory lesions, but facial erythema may persist despite treatment.), applied daily on a long-term basis to maintain remission |
|
|
Lichen planus: 扁平苔癣
|
与真菌无关 immunologically mediated skin disorder, middle age adults, It typically involves the skin/nails/mucous membranes of the mouth/external genitalia.
Shiny, discrete, intensely prutitic, polygonal shaped violaceous plaques and papules that are usually present on the flexural surfaces of the extremities. Wrists are common site of skin involvement. A characteristic whitish lacy pattern- Wickham;s striae, often seen on the surfaces of the papules and plaques. (The typical rash of lichen planus is well-described by the "5 Ps": well-defined pruritic, planar平的, purple, polygonal papules.) Lichen planus is associated with hepatitis C virus infection Diagnosis is mainly clinical. A punch biopsy of the most prominent skin lesion can confirm diagnosis: hyperkeratotic epidermis + irregular acanthosis + focal thickening in the granular layer of epidermis + irregular acanthosis + liquefactive degenerating keratinocytes in the lower epidermis (colloid bodies or Civatte bodies) + linear fibrin deposition in the basal layer |
|
|
Porphyria cutanea tarda
|
is a condition characterized by painless blisters + hypertrichosis + hyperpigmentation.
It is often associated with HCV and iron overload and can be triggered by the ingestion of ethanol, estrogens, |
|
|
remove tattoo marks
|
Common techniques used to remove tattoo marks
Dermabrasion (removal of the superficial layer of the epidermis, allowing the pigment to leach out of the skin) Cryosurgery Thermal cautery Surgical resection Laser removal (laser break up the pigments into smaller molecules, which are taken up and cleared by the macrophages in the skin, can leave scar marks→skin hypo/hyper-pigmentation) |
|
|
Alopecia areata斑秃
|
is a type of non-scarring hair loss that can affect any hair-bearing area. It is an autoimmune process.
Well-demarcated, round, non-scarred patch of complete hair loss. “Exclamation point hairs”(hairs which are tapered near the insertion into the scalp, especially at the periphery of an alopecic plaque) is considered pathognomonic of but not necessary for the diagnosis. Areas of involvement may be single or multiple. Nail pitting is a common associated finding. Self-limited but may be relapsing and remitting or chronic and progressive. ↑risk for other autoimmune conditions including autoimmune thyroid disease, vitiligo白癜风and pernicious anemia DD 1. Medication-related hair loss Diffuse non-scarring thinning Telogen effluvium静止期脱发usually begins 3 months after some precipitating event such as an illness, stressor or new medication (beta-blocker, anti-coagulants, systemic retinoids, anti-convulsants and anti-thyoid medications are frequently implicated causes of telogen effluvium) Chemotherapeutics can cause anagen effluvium生长期脱发which usually begins within 1-2w of chemotherapy initiation. 2. scarring alopecia tinea capitis (erythema + scaling + “black dot” alopecia), folliculitis, + inflammation + hyperkeratosis 3. Androgenetic alopecia: treat with low-dose Finasteride indefinitely 4. Metabolic conditions: hypothyroidism, hyperthyroidism, iron deficiency 5. Trichotillomania: psychiatric impulse control disorder Treatment: Intralesional corticosteroids there is a high chance of recurrence of hair loss even after successful treatment. |
|
|
Oral terbinafine or itraconazole X 6w-12w
|
are superior methods of treatment for confirmed cases of onychomycosis 甲癣(The diagnosis is typically established with KOH examination of nail bed scrapings).
Unlike Trichophyton tonsurans infection, Microsporum canis infection is characterized by a bright green fluorescence when the lesion is observed under Wood’s ultraviolet lamp. Well demarcated scaling and slightly erythematous alopecia is suggestive of tinea capitis or ringworm of the scalp. The diagnosis is confirmed by KOH examination of epilated hair stubs. |
|
|
Tinea pedis
|
Tinea pedis is a common superficial fungal infection of the foot with pruritic, erythematous, well-demarcated lesions, usually between the toes and extending to the sole and side of the foot.
DD Scabies is due to skin infestation by a mite, intense pruritus worse at night. Multiple, small, erythematous papules and characteristic burrow. It involve the sides and webs of finger, flexor aspects of the wrists, extensor aspects of the elbow, axillary folds, periumbilical areas and waist, lower half of the buttocks and adjacent thighs. |
|
|
Tinea vesicolor花斑癣
|
is a fungal infection of the skin caused by the dimorphic yeast Pityrosporum orbiculare (Malassezia Furfur – “spaghetti and meatball “ appearance on KOH prep).
Multiple small circular maculae are observed that may vary in color (white, pink or brown). The rash is more prominent in the summer (more tanning skin) because the yeast inhibits pigment transfer to keratinocytes and makes the affected skin more demarcated from unaffected tanned skin. The lesions are usually asymptomatic although mild pruritus may be present. Treatment: topical ketoconazole |
|
|
Reactivation of the latent infection by herpes zoster
|
Oral acyclovir is the mainstay of therapy
Localized zoster in an immunocompetent patient is only transmitted via direct contact with the open lesions. Contact precautions are not necessary for patients with localized zoster in a community setting. Contact precautions are recommended for hospitalized patients who are at a higher risk of transmitting the infection to health care workers and other patients. Localized zoster in immunocompromised patients or patients with disseminated zoster has a significantly higher risk of disease transmission. These patients should be hospitalized and placed on strict isolation until all their lesions have crusted. Postherpetic neuralgia (PNH): pain/other sensory symptoms >1 month after the resolution of skin lesions of herpes zoster. A significant number of patients also experience the pain with non-painful stimuli such as a light touch, a condition known as allodynia. TCA (amitriptyline, desimipramine) are the mainstays of therapy for postherpetic neuralgia. TCA+opioid analgesic for early stages of treatment. Topical capsaicin↑the substance P release. Gabapentin can be used for patients who are unable to tolerate TCA. |
|
|
Doxycycline is a photosensitizing
|
agent and may cause exaggerated sunburn in some patients.
Treatment: replenishment of lost fluids and relief for pain/prutitus.(diphenhydramine hydroxyzine) NSAIDS (oral/topical indomethacin, ibuprofen) Isotretinoin → hypertriglyceridemia in 25% of individuals → pancretitis after treatment of acne Photoaging arises from the combination of intrinsic aging and damage caused by ultraviolet light. It results in coarse, deep wrinkles on a rough skin surface and may be accompanied by actinic keratoses, telangiectasias and brown spots. Cigarette smokers have been shown to have more and deeper wrinkles than do nonsmokers. Tretinoin is an emollient cream approved by the FDA for reduction of fine wrinkles, mottled hyperpigmentation and roughness of the facial skin. Tretinoin is also successful in reducing actinic keratoses and in improving the appearance of brown spots, regardless of etiology. |
|
Intralesional corticosteroids
|
are the preferred means of treating most keloids. The earlier the lesion is treated, the greater the chance of improvement. However, patients should be warned that recurrence after treatment is common.
|
|
Pressure ulcer
|
Stage 3/4 pressure ulcers heal best when all pressure is removed from the involved area and a moist wound environment is maintained (the wound should be covered with an occlusive dressing or loosely packed with saline-moistened gauze., difficult to treat), the fluids found within wounds are thought to contain tissue growth factors that promote reepithelialization, therefore, dry gauze is not an ideal treatment method. Viable surrounding skin should be kept dry.
|
|
|
Psoriasis
|
Asymptomatic or mild itching
Mild, asymptomatic psoriasis without any joint or nail involvement does not need aggressive treatment. Topical corticosteroid creams are the mainstay of therapy for localized skin lesions. High-potency agent (betamethasone) 0.05% should be initially used for thick plaques on extensor surfaces. The lesions should be covered with a plastic wrap or occlusion tape after steroid cream application to maximize its effects. Low-potency steroids (hydrocortisone 1%) should only be used on the face and intertriginous areas. Methotrexate is very effective in severe psoriasis, psoriatic arthritis and psoriasis involving the nails. The most common drugs that may exacerbate psoriatic lesions are beta-blocker, ACEI, antimalarial drugs, NSAIDS and lithium. It should be discontinued. |
|
|
Sporotrichosis
|
Sporothrix schenckii
Involved in outdoor activities/occupations A popular lesion over the site of inoculation, ulcerates over time with non-purulent discharge from the lesion. Similar lesions are seen along the lymphatic channels proximal to the original lesion. Treatment: itraconazole X 3-6 monthsi Diuretic-induced hypokalemia is a common complication of antihypertensive/congestive heart failure therapy especially when loop-diuretics are used. Paralytic ileus is one of the indications for prompt parenteral potassium replacement. EKG recording should also be taken. Intravenous potassium must be given immediately when hypokalemia is found in certain situations such as hepatic encephalopathy, ventilatory failure, Paralytic ileus and cardiace arrhythmia. In patients with symptomatic or severe hyponatremia (Na <115 mEq/L), an aggressive initial correction at the rate of 1.5-2 mEq/L/hour for the first 3-4 hours is indicated. Hypertonic saline should be used initially in the setting for rapid correction of hyponatremia. The plasma sodium levels should be monitored frequently to avoid raising sodium levels more than 12 mEq/L in the first 24 hours. Hyponatremia : cerebral edema --- nausea, malaise, headache, lethargy, obtundation, seizure, coma, respiratory arrest if Na < 115-120 mEq/L *** Water restriction is the mainstay of therapy for hyponatremia 115 mEq/L in pt with advanced CHF. The use of hypertonic saline to increase the plasma sodium concentration is usually indicated only for pt with symptomatic hyponatremia. |
|
|
Alcoholic ketoacidosis
|
Anion gap acidosis +↑osmolal gap + ketonemia/ketonuria + low or high or normal blood glucose levels (in diabetic ketoacidosis, blood glucose is generally higher than 250 mg/dL)
Treatment: dextrose normal saline + thiamine |
|
|
Hypophosphatemia
|
Hypophosphatemia is not very recognized in hospitalized patients. Continuous glucose infusions are the leading cause of hypophosphatemia in hospitalized patients. The patients are usually alcoholic or otherwise debilitated and the nadir in serum phosphate appears in the first few days after admission. Hypophosphatemia can impair ATP generation which is needed by the sketetal muscle to perform work, and muscle weakness can result. Respiratory muscle weakness has been reported, this is severe enough to prevent weaning from mechanical ventilation. In addition, phosphate deficiency reduces cardiac contractility and chronic phosphate deficiency has been implicated as a cause of cardiomyopathy. Phosphate depletion is associated with depletion of 2,3 diphosphoglycerate, and this causes a leftward shift of the oxyhemaglobin dissociation curve. As a result, the oxygen bound to hemoglobin is less readily released to the tissues
|
|
|
Alcoholism-hypophosphatemia-refeeding syndrome
|
Patients with severe alcoholism often have chronic depletion of phosphate secondary to ↓VitD and phosphate intake along with intestinal uptake in those with chronic diarrhea. Urinary phosphate excretion may also because of secondary hyperparathyroidism from ↓VitD intake as well as a proximal tubular reabsorption defect from alcohol abuse itself. Despite the depletion of phosphate, serum levels are often maintained (extracellular shift) until the patient is admitted to the hospital and fluids are initiated.
Once the patient is fed or receives iv fluids with glucose, ↑insulin secretion or respiratory alkalosis → shifting of phosphate intracellularly → weakness, rhabdomyolysis , ↑CPK (many alcoholism have myopathy) |
|
|
Exogenous hyperthyroidism
|
Non-enlarged thyroid gland
RAIU—low thyroglobulin – low Thyroglobulin is cosecreted with endogenous T3/T4 RAIU—low thyroglobulin – high: struma ovarii, postpartum thyroiditis, subactue granulomatouos (DeQuervain’s) thyroiditis Thyroglobulin level is useful in the follow-up management of pt with differentiated thyroid cancers and in the evauation of suspected factitious thyrotoxicosis. |
|
|
adrenal mass
|
In any patient with an adrenal mass, essential laboratory studies include serum electrolytes, dexamethasone suppression testing, and 24-hour urine catecholamine, metanephrine, vanillylmandelic acid and 17-ketosteroid messurement. Surgical excision is recommended for all functional tumors, all malignant tumors (which demonstrate a characteristic heterogenous appearance on imaging), and all tumors > 4cm. All other masses can be managed conservatively with serial abdominal imaging and removed if they increase in size.
|
|
|
Subclinical hypothyroidism (↑TSH 5-10, --T4)
|
Treatment is warranted in the presence of
1. antithyroid antibodies: anti-peroxidase-TPO-antibodies (high chance for a patient to become overtly hypothyroid: Harshimoto thyroiditis) 2. abnormal lipid profile 3. symptoms of hypothyroidism 4. ovulatory and menstrual dysfunction 5. TSH>10 uU/ml Downside of the treatment in asymptomatic patients is the risk of overtreatment → bone loss and atrial fibrillation. The American Thyroid Association recommends all individuals over the age of 40 to be screened for thyroid dysfunction. |
|
|
Alpha blockade (phenoxybenzamine)
|
is done for 10-14 days preoperatively to control HTN and restore intravascular volume in pheochromocytoma. Beta-blockers are only given to patients who are adequately alpha-blocked. The chances of intraoperative complications are much higher with inadequate preoperative alpha blockade.
CT/MRI is typically done while the patient is on alpha blockade. MIBG resembles norepinephrine and is taken up by pheochromocytomas. The sensitivity of MIBG scan is 70%. MIBG scan is performed in patients who have borderline biochemical values, but with CT showing an adrenal mass. Intraoperative hypotension in patients with pheochromocytoma responds to an iv bolus of normal saline. (NOT COLLOID, NOT VASOPRESSOR). |
|
|
Amiodarone
|
Amiodarone →↓conversion of T4→T3 →↓ T3 ,↑T4
Amiodarone → hypothyroidism or thyrotoxicosis due to high iodine content |
|
|
Sulfonylureas toxicity
|
Sulfonylureas toxicity (glyburide) →↑ insulin release → hypoglycemia
Treatment: 1. initial treatment is dextrose 2. Octreotide (somatostatin analogue) →↓ insulin release Patients with CAD are at risk of myocardial ischemia when levothyroxine is first started and the medication should be started very slowly in these patients. Hypothyroidim in the absence of myxedema coma or other severe symptoms usually only mildly increases the perioperative risk. |
|
|
Thyroid nodules
|
Thyroid nodules > 1cm: fine needle aspiration biopsy
Thyroid nodules < 1cm: followed with thyroid U/S on a yearly basis Radioiodine uptake and scan are useful for diagnosing toxic adenoma in thyrotoxic patients. |
|
|
Graves disease in pregnancy
|
Methimazole is a potential teratogen and PTU is associated with liver failure
PTU – first trimester Switch to MMI for the second/third trimester |
|
|
VitD deficiency
|
Patients following gastric bypass surgery develop some degree of malabsorption, and may require a higher dose of VitD supplementation to prevent osteomalacia. In patients with VitD deficiency, the serum phosphorus level decreased before the calcium level. The deficiency in vitD leads to a high PTH levels (secondary hyperparathyroidism) and causes urinary phosphate loss.
Plasma 25-hydroxyvitamin D level is a very sensitive indicator for VitD stores. |
|
|
diabetic gastroparesis.
|
A scintigraphic gastric emptying study is the test of choice for diagnosing diabetic gastroparesis. However gastric outlet obstruction (secondary to peptic ulcer disease/malignancy) can have a similar appearance on a gastric emptying study. The treatment of these two conditions differs drastically. Gastric outlet obstruction should therefore first be ruled out with either endoscopy or a barium upper GI exam. Gastroduodenal manometry can be considered in patients who have evidence of delayed gastric emptying on a scintigraphic study but who lack a clear underlying disorder such as diabetes.
Delayed gastric emptying → post-meal hypoglycemic episodes (peak-effect of insulin is not corresponding with the glucose peaks after meals, the rise in blood glucose levels is significantly delayed after the peak insulin levels → hypoglycemia) Treatment 1. The first step in managing diabetic gastroparesis is dietary modification consisting of small and more frequent meals which are low in fat and fiber. 2. when dietary modifications not effective: erythromycin/metoclopramide |
|
|
Medullary thyroid cancer
|
Elevated calcitonin levels in patients with medullary thyroid cancer (parafollicular C-cells) following total thyroidectomy indicate metastatic disease. CT scan of the neck and chest is recommended as the next step to look for metastatic disease.
Medullary thyroid cancer cells do not take-up iodine, therefore total body iodine scan is useless |
|
|
Hpyercalcemia
|
1. Hypervitaminosis D (secondary to granulomatous disease)
2. primary hyperparathyroidism hypercalcemia + urine calcium > 200mg/day + upper limits of normal PTH suggest hyperparathyroidism (↑Ca →↓PTH) 3. Familial hypocalciuric hypercalcemia Mutation in a calcium sensing receptor (CaSR) which is found in the parathyroid gland and kidneys urine calcium < 100mg/day generally asymptomatic from mild hypercalcemia, no surgical treatment is necessary 4. Malignancy – high PTHrp + low PTH (negative feedback), Ca is much higher in pt with malignant lung tumors than those with primary hyperparathyroidism 5. Excessive bone resorption after immobilization, usually in patients with a very high bone turnover (e.g. adolescent patients and older patients with Paget’s disease). It happens in days to weeks following immobilization. |
|
|
Primary hyperparathyroidism
|
Indications for parathyroidectomy in primary hyperparathyroidism
1. All symptomatic patients 2. Asymptomatic patients with Serum Ca > 1mg/dl above the upper limits of normal Creatinine clearance of < 60ml/min A T-score of < 205 on bone mineral densitometry or previous fragility fracture Age < 50y |
|
|
Nonfunctioning pituitary adenoma
|
Generally arise from gonadotropin-secreting cells of the pituitary glands
Suppressed LH/FSH, increased α-subunits (LH/FSH are composed of a common α-subunits and hormone-specific β-subunit) Hypogonadism (amenorrhea) First-line therapy is transphenoidal surgery. Patients might regain their normal gonadal functions after resection |
|
|
Hypoglycemia in type I diabetic patients
|
DD 1. exercise 2. wrong insulin dose in geriatric population/insulin pump dysfunction 3.renal failure
Decreased insulin dosage before/during increased physical activity is useful to prevent hypoglycemia in type I diabetic patients. When exercise is performed in the early afternoon, the morning dose of NPH should be reduced by 20-30%. Type I diabetic patients who are on insulin pumps have more flexibility for changing their insulin dose, and may participate in unplanned physical activities. Under certain circumstances, type I diabetic patients should avoid exercise or change the type of physical activity. For instance, Exercise should not be performed when blood sugar > 250mg/dl because it can precipitate ketoacidosis. Intense exercise programs have been known to cause progression of proliferative diabetic retinopathy, therefore avoid weightlifting which tends to increase intravascular pressure within the retinal vessels, and predispose them to hemorrhage. If the patient developes hypoglycemia during exercise, she should immediately consume mono or disaccharides such as candy or glucose tablets, Granola bars contain a complex carbohydrate and is not the preferred treatment of acute hypoglycemia. |
|
|
Iodine-induced thyrotoxicosis
|
occurs mainly in patients with nodular goiter, where excess iodine can serve as a substrate for excessive thyroid hormone formation. Symptoms occurred a few weeks after coronary angiography (extreme fatigue, shakiness, weight loss and palpitations, tachycardia despite beta-blocker use). Iodine-induced thyrotoxicosis is a self-limiting disorder if the source of excess iodine is discontinued. However it can persist for months and is usually refractory to antithyroid medications.
1. beta-blocker – mild symptoms 2. antithyroid drugs—moderate to severe symptoms 3. radioactive iodine ablation is ineffective because of low radioactive iodine uptake. 4. potassium perchlorate – refractory cases |
|
|
Apathic thyrotoxicosis
|
Elderly patients may not have classical manifestations of thyrotoxicosis and can present with apathy, depression , loss of appetite and severe weight loss. SOB and Af are also commonly seen in these patients.
The most common causes of mental status change in elderly are medications, infection (UTI and pneumonia) and metabolic abnormalities |
|
|
The use of glucocoricoids
|
The use of glucocoricoids for < 3w, even in higher doses (> 7.5mg prednisone daily), does not cause significant suppression of the HPA axis. When given for a short period, glucocorticoids can be stopped rapidly without causing significant adrenal insufficiency.
|
|
|
Papillary thyroid cancer
|
Papillary carcinoma-most common, excellent prognosis, "ground-glass" nuclei (Orphan Annie) psammoma bodies, nuclear grooves. ↑risk with childhood irradiation.
Nearly total thyroidectomy (NTT) is the preferred treatment for patients with papillary thyroid cancer. By taking out most of the thyroid tissue, it becomes easier to destroy the resideul thyroid tissue (small thyroid tissue left after surgery) by giving high-dose radioactive iodine. Throglobulin is used as a tumor marker for following patients after NTT and radioactive iodine treatment. Detectable serum thyroglobulin following NTT and radioactive iodine treatment suggests residual disease. Staging of papillary thyroid cancer is not performed preoperatively even when metastase. Most papillary thyroid cancers are slow growing and the prognosis is usually very good. In patients with thyroid cancer in remission, the dose of levothyroxine is adjusted to suppress the TSH below normal range, usually between 0.1 and 0.3uU/mL. For patients with distant metastasis, even lower levels of TSH are required. Patients being treated with suppressive doses of levothyroxine are at an increased risk for bone loss and atrial fibrillation. Levothyroxine suppression For high risk patients (Stage III and IV disease), we recommend full levothyroxine therapy (TSH <0.1 mU/L) . For low-risk patients (Stage I and II disease), we suggest levothyroxine suppression of TSH to slightly below the lower half of the reference range (0.1 to 2.0 mU/L) The presence of heart disease or low bone density may necessitate a lower level of TSH suppression with smaller doses of thyroxine. The dose also may be decreased to allow the TSH to rise into the normal range in low risk patients who remain disease-free for 5 to 10 years after primary therapy |
|
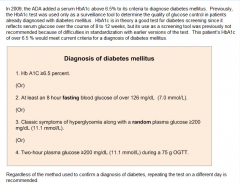
Diagnosis of diabetes mellitus
|
Fasting blood glucose < 100 mg/dl: normal
Fasting blood glucose 100-126 mg/dl : impaired fasting blood glucose --- increased risk for CAD even with a normal lipid profile and progression to overt DM |
|
|
Graves’ disease
|
In the United States, the majority of patients with Graves’ disease are treated with radioiodine ablation. Understand that radioactive iodine treatment for Graves’ disease is associated with worsening of ophthalmopathy, which can be prevented by concurrent administration of glucocorticoids.
Radioactive iodine ablation is contraindicated in large retrosternal goiters because post-radioiodine inflammatory swelling of the thyroid gland may compromise the airways. Antithyroid drugs should be discontinued a few days before radioiodine administration because these drugs cause a decrease in radioiodine uptake. |
|
|
Thyroid storm
|
1. Glucocorticoids inhibit T4→ T3
2. antithyroid drugs, PTU/Methimazole, higher dose/+ 3. Beta-blocker 4. Iodine: inhibit inhibit T4→ T3 and hormone release they should be given at least one hour after the thionamide to prevent the iodine from being used as substrate for new hormone synthesis |
|
|
Pseudohypoparathyroidism
|
(resistance of PTH on its target tissue)
↓Ca + ↑phosphorus +↑PTH Bilateral cataracts + calcification of basal ganglia 1. type 1A: has features of Albright hereditary osteodystrophy (AHO) in addition to hypoparathyrodism shore stature, round facies, short fourth/fifth meatcarpals, short neck 2. type 1B: no feature of AHO 3. pseudohypoparathyroidism (PPHP) no hypocalcemia and hyperphosphatemia because the resistance to PTH is mild + AHO features 4. Acute hyperphosphatemia can cause a decrease in calcium levels. Seen in patients with seizure, tumor lysis or acute renal failure. |
|
|
DVT
|
HRT should be avoided in patients with a history of previous thromboembolic disease. Warfarin should be continued for 3-6m after a first episode of DVT.
Tamoxifen is also associated with increased risk of DVT. |
|

Drugs for DM
|
Metformin is contraindicated in patients with alcoholism, congestive heart failure and renal failure.
Pioglitazone is an insulin sensitizer and should be carefully used in patients with congestive heart failure because it can cause salt and water retention, which can worsen the cardiac failure. Pioglitazone is contraindicated in patients with NYHA class III and class IV congestive heart failure. Glyburide increases insulin release and is useless in patients with beta cell loss secondary to chronic pancreatitis. When renal failure, stop metformin and sulfonylureas (glyburide) that are metabolized exclusively by the kidneys Insulin:Patients with type I diabetes are managed with a combination of basal insulin (Type I DM requires either 2 injections of NPH or one dose of a long-acting insulin like glargine to provide basal insulin delivery) and meantime boluses of regular or ultrarapid acting insulin (lispro or aspart) NPH has its peak actions after 4-6 hours of injection, and its effects can last up to 16-18 hours. Hypoglycemia episode (glucose < 60 mg/dL) during exercise in type I DM can be managed by lowering NPH in the morning, avoiding injections of insulin in the excercising limbs and eating before excercising. Regular (rapid onset of action, short duration of action) and NPH (slower onset of action, longer duration of action) human insulin are the most commonly-used preparations. Regular insulin has an onset of action (begins to reduce blood sugar) within 30 minutes of injection, reaches a peak effect at 1-3 hours, and has effects that last 6-8 hours. NPH insulin is an insulin with an intermediate duration of action. It has an onset of action starting about 2 hours following injection. It has a peak effect 4-12 hours after injection, and a duration of action of 18-26 hours. Chronic pancreatitis → islet damage → type I DM Patients with type 2 DM are likely to have higher plasma C-peptide and insulin levels compared to patients with islet damage Patients with DM secondary to chronic pancreatitis are more prone to develop hypoglycemic reactions with insulin use due to the associated loss of both alpha and beta cells (in type I DM, there is selective loss of beta-cells). Alpha cells in the islets secrete the counterregulatory hormone glucagon, which is important in increasing blood glucose levels during hypoglycemia, therefore, loss of alpha cells due to chronic pancreatitis will result in a poor glucagon response to hypoglycemic episodes |
|
|
Lactic acidosis
|
Metformin → lactic acidosis, especially in the elderly or pt wih renal/hepatic/heart failure
Hypoperfusion Tissure hypoxia (sepsis/hypovolemic shock/hypoxemia) The main causes of high anion gap metabolic acidosis are: renal failure, ketoacidosis, lactic acidosis or intoxication of ASA, ethylene glycol or methanol. Metformin induced lactic acidosis: Absence of a raised plasma ketone level excludes ketoacidosis as the cause of the metabolic acidosis. Treat with large amounts of sodium bicarbonate |
|
|
Diabetic ketoacidosis treatment
|
1. iv normal saline (0.90% w/v of NaCl, about 300 mOsm/L) with potassium added for patients with a serum potassium < 5.3mEq/L.
2. iv insulin should be continued until the anion gap has resolved 3. If serum glucose < 200 mg/dL but the paitient still has an elevated anion gap >12, the rate of insulin infusion should be halved and iv fluids should be converted to D5 1/2 NS (Half-normal saline (0.45% NaCl), often with "D5" (5% dextrose), contains 77 mEq/L of Na and Cl and 50 g/L glucose.) in order to prevent hypoglycemia 4. Most accurate measure of the severity of DKA is serum bicarbonate, if bicarbonate is very low, the patient is at risk of death. 5. Criteria for resolution of DKA include a serum glucose < 200mg/dL, an anion gap of < 12 meq/L, serum bicarbonate of > 18meq/L and ability to eat. The patient should be started on subcutaneous insulin after DKA has resolved, but the iv insulin should be continued for the first 2h giving time for the subcutaneous insulin to become absorbed and take effect. Subcutaneous insulin regimen consists of rapidly acting insulin to cover the meal and basal insulin (NPH or glargine) to prevent the rise of blood sugar levels between meals. Oral hypoglycemic agents are typically avoided in hospitalized patients. Normal anion gap: 7-13 Normal bicarbonate: 22-28 meq/L |
|
|
Nelson’s syndrome
|
Pituitary enlargement + hyperpigmentation + visual field defect following bilateral adrenalectomy
Usually these tumors are rapidly growing and can be treated with surgery/local radiation |
|
|
Insulin in pregnancy
|
During pregnancy, the requirement of insulin increases, particularly during the 2nd trimester due to the diabetogenic effects of the placental hormones.
Following a normal labor or cesarean section. There is a decrease in the level of these hormones, which drastically decreases the patient’s insulin requirement. The patient should take her normal dose of insulin on the night before surgery even if she is not eating. Insulin infusion is the best way to treat a patient perioperatively and the drip rate is adjusted to keep the blood glucose under 160 mg/dL. Insulin has a half-life of 5 minutes and its hypoglycemic effects lasts < 30min. |
|
|
Diabetic neuropathy
|
A severe burning sensation that can interfere with sleep, necessitating some form of pain control.
First-line: duloxetine (serotonin norepinephrine reuptake inhibitor-SNRI), pregabalin, TCA Others: gabapentin, lamotrigine, carbamazepine Topical capsaicin cream /lidocaine Strict blood glucose control decreases the risk of developing a new neuropathy in patients with DM, prevent microvascular complications, including diabetic neuropathy |
|
|
Euthyroid sick syndrome (ESS)
|
Common in hospitalized patients, acute severe illness, due to caloric deprivation and increae IL-1/6
↓total T3 (↓T4 →T3 conversion), --normal total T4, --TSH, ↑ reverse T3 (inactive) Low T4 indicate a bad prognosis TSH transiently ↑above normal limits when patients recover from their illness The treatment with thyroid hormone is not warranted in euthyroid sick syndrome. Thyroid function tests are also not performed in patients recovering from major systemic illness |
|
|
Central hypothyroidism
|
The majority of patients with central hypothyroidism have coexisting deficiencies in other pituitary hormones,
Pituitary-adrenal function should be assessed, usually by an ACTH stimulation test, before thyroxine (T4) therapy is begun in all patients with central hypothyroidism. If adrenal insufficiency is present, glucocorticoid therapy should be given concomitantly with T4. If you give levothyroxine to pt with adrenal insufficiency the pt wont be able to cope up with the stress which will occur with increased metabolism that will occur due to levothyroxine. ↑C-peptide +↑ serum insulin + hypoglycemia DD 1. oral hypoglycemic agents: sulfonylurea/meglitinide 2.insulinoma Exogenous insulin→(+) antibody against insulin |
|

Diabetic retinopathy
|
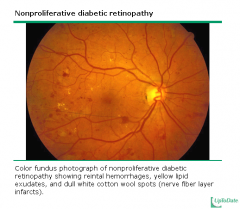
Vitreous hemorrhage, retinal detachment and macular edema
Macular edema occurs due to vascular permeability of the retinal blood vessels. Usually pt with macular edema have background diabetic retinopathy (microaneurysms, hard/soft exudates, dot/blot hemorrhages ) Diabetic retinopathy requires some years to develop, Poor glycemic control and blurry vision can be due to the swelling in the optial lens secondary to osmotic changes. Improving glycemic controls is likely to improve the patient’s symptoms. |
|
|
Diabetic retinopathy
|
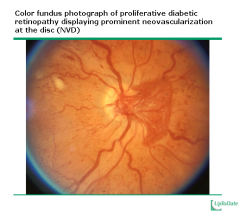
|
|
|
Polyglandular autoimmune failure type II (Schmidt’s syndrome)
|
Addison’s diseae
Type I DM Antoimmune thyroid disease The clinical features of glucocorticoid-induced DM resemble type 2 DM. |
|
|
Medications that impair the absorption of levothyroxine
|
Calcium
Iron (iron and food the absorption of levothyroxine by as much as 40%) Pt with hypothyroidism should be instructed to take levothyroxine on an empty stomatch, preferably in the morning, separately from other medications |
|
|
Postpartum thyroiditis
|
Hyperthyroidism then hypothyroidism
↓RAIU, painless, positive TPO antibodies, increased thyroglobulin, high T4 DD 1. subacute thyroiditis (Quervain thyroiditis): follow URI, pain over the thyroid and pain referred to the lower jaw, ears, neck or arms initial ↑T3/T4, ↓RAIU 2. Lymphoocytic thyroiditis, Low TSH, low T4 3. Graves’ disease Increased RAIU |
|
Paget’s disease
|
Pain not released by acetaminophen
X-ray: thickening of outer cortex of femur + sclerotic lesions Technetium bone scan: ↑uptake in the bone Indications for treatment of Paget’s disease include bone pain, involvement of weightbearing bones, neurological compromise, hypercalcemia, hypercalciruia and congestive heart failure. Treatment: Bisphosphonates (alendronate X6m, risedronate X2m and pamidronate) |
|
|
Glucagonoma
|
“Necrolytic migratory erythema” rash: red, raised, scaly rash on the face, abdomen. Perineum and distal extremities
Most are malignant and have metastasis, mainly in the liver at the time of diagnosis. Some of its clinical manifestations are due to the secretion of other peptides, such as VIP (facial flushing),, calcitonin and GLP1 The diagnosis is suspected clinically (mild diabetes mellitus, glossitis, necrolytic migratory erythema) and then confirmed by messuring glucagon levels Treat: surgical |
|
|
obstructive sleep apnea (OSA)
|
There is no indication for special tests in snoring patient without associated symptoms and clinical findings of obstructive sleep apnea (OSA). Advise to lose weight, stop smoking and avoid alohol near bedtime.
The predisposing factors include obesity, genetic or acquired upper airway structural abnormalities, HTN, smoking and alcohol and sedative-hypnotic use. |
|
|
Epistaxis
|
The majority of epistaxis in children/young adults is anterior and generally originates from Kiesselbach’s plexus.
Kiesselbach plexus is a venous collection system in the anterior nose that contains blood from the ethmoid and sphenopalatine arteries. It is the most common site of bleeding. The ethmoid and sphenopalatine arteries supply the posterior area of the nose, and bleeding from these sites is more difficult to control. Anterior bleeding that is not controlled by nostril pinching is next treated by an attempt to localize and cauterized the site of bleeding. Bleeding is first controlled temporarily by applying pressure with a cotton pledget impregnated with a vasoconstrictor such as phenylephrine 0.25% and a topical anesthetic such as lidocaine 2% until the site is anesthetized. Siver nitrate chemical cautery or needlepoint electrocautery can then be attempted through a nasal speculum. |
|
|
T1a N0 M0 SCC 声门癌
|
The initial treatment of a squamous cell carcinoma of the glottis which is confined to one vocal cord and which has not metastasized is a radiation therapy, laser excision or partial vocal cordectomy
T4 (tumors invading thtough the thyroid cartilage or with direct extralaryngeal spread): total laryngectomy T3 (tumors confined to the larynx with vocal cord fixation): induction chemotherapy followed by radiation |
|
|
PCP intoxication
|
A low-stimulation environment is ideal for pt with PCP intoxication (belligerence, impulsiveness, vertical and horizontal nystagmus in awake or agitated pt is characteristic for PCP intoxication, nystagmus is typically associated with prominent sedation)
|
|
|
Scuba diving
|
Scuba diving is associated with a range of pressure-related injuries. It is important to inform the patient about the possibility of such injuries and to educate him about the basic measures that help prevent them discourage flying in a plane within 24h. The most common condition associated with scuba diving is ear barotraumas 气压伤. The pt with h/o allergic rhinitis has increased susceptibility to ear and sinus barotraumas.
Avoid diving if he has any symptoms of allergy. The use of non-sedating decongestants ( specially pseudoephedrine) before diving reduces the incidence of ear and sinus barotraumas by 75%. |
|
|
Rhinitis
|
The diagnosis of rhinitis is not always clear and laboratory evaluation may be necessary. Nasal cytology is the most appropriate next step in the management of the patient. Demonstration of neutrophils in nasal secretions suggests infectious cause of the disease while predominance of eosinophils indicates that allergic rhinitis is the most likely diagnosis. However nasal cytology has low specifity.
Other causes of nasal eosinophilia include nasal polyposis (including aspirin sensitivity ) and non-allergic rhinitis with eosinophilia. A common cause of perennial non-allergic rhinitis, vasomotor rhinitis, is characterized by the absence of nasal eosinophilia. Vasomotor rhinitis is caused by increased sensitivity of the vidian nerve and is a common cause of clear rhinorrhea in the elderly. Often patients will report that they have troubling rhinorrhea in response to numerous nasal stimuli, including warm or cold air, odors or scents, light, or particulate matter. |
|
|
Presbycusis
|
A sensorineural hearing impairment, initially affects the high-frequency range of hearing.
Can participate in a phone conversation and talk to wife but has difficulties in understanding spoken language during business meetings and while watching TV shows The decreased ability to discriminate speech in pt with presbycusis is especially obvious in a nosiy, distracting environment. |
|
|
External otitis
|
External otitis is associated with swimming, excessive cleaning or itching of the ear or usage of occlusive devices. Treatment must first begin with cleaning of the ear canal with a cerumen wire loop or cotton swab. Irrigation of hydrogen peroxide is an acceptable alternative cleaning method if the tympanic membrane is visualized and intact.
|
|
|
Nitroprusside
|
Dilate both arterioles and veins. It has a very rapid onset of action. Its effects disappear within minutes, thereby allowing for rapid titration of its infusion according to the blood pressure response. It is metabolized to cyanide ions in the blood where the RBC take up these cyanide ions and these new complexes are converted into cyanocobalamin. This is then metabolized to thiocyanate by the hepatic and renal enzymes.
According to the current FDA dose recommendation, the maximum doses of 10ug/kg per minute should never be given for > 10min. Rapid, prolonged and excessive use of nitroprusside infusions can lead to the development of cyanide toxicity (tachycardia, clinical deterioration, lactic acidosis, change in mental status, coma and seizures). It is especially important to recognize this early in the presence of renal failure |
|
|
Salicylate overdose – aspirin overdose
|
Initial : tinnitus, restlessness, N/V, mild GI discomfort, after a few hours, a depressed level of consciousness
High anion gap metabolic acidosis + respiratory alkalosis + transient hepatotoxicity + acute renal failure + depressed mental status Hyperventilation (breath heavily) associated with metabolic acidosis is hardly ever acoompanied by dyspnea. Hyperventilation without dyspnea is suggestive of respiratory alkalosis. It is important to determine salicylate serum levels, > 35mg/dl indicate significant acidosis Treat: alkalinization of the urine |
|
|
Ethylene glycol intoxication
|
Fomepizole is competitive inhibitor of ADH and is the antidote of choice in cases of ethylene glycol intoxication. It also prolongs the half life of ethanol, therefore, simultaneous use with ethanol is not recommended.
|
|
|
sharp object ingestion
|
In all symptomatic patients or patients with a history of sharp object ingestion (fish or chicken bone, toothpicks, needle or pins), an urgent endoscopy should be performed to remove the foreign body and to prevent esophageal perforation.
Foreign bodies should not be allowed to remain in the esophagus for >24hours. |
|
|
Co-oximetry --- CO poisoning
|
Co-oximetry is used to measure carboxyhemoglobin levels. This spectrophotometric laboratory method can distinguish normal hemoglobin from carboxyhemoglobin
|
|
|
brushed off unknown dry chemicals,
|
When an incident involving exposure to hazardous materials occurs, it is important to brushed off unknown dry chemicals, then irrigate the area with copious amounts of low-pressure water (unknown liquid chemicals, in contrast, are simply immediately washed off with water.)
|
|
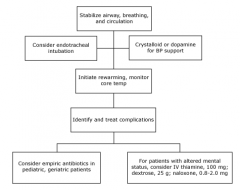
Hypothermia
|
Risk factor: older age, homelessness, alcohol abuse, hypothyroidism, adrenal insufficiency, sepsis, malnutrition
p/w confustion, ataxia, slurred speech, tachycardia, tachypnea (Temp: 32-35C) marked CNS depression, hypoventilation, hypotension, bradycardia, hyporeflexia and cardiaccondution abnormalities (Temp:28-32C) severe hypothermia(core temperature <28C) can cause marked hypotension, areflexia, coma, malignant ventricular arrhythmias (VF) and asystole. The first step in the resuscitation of such patients is to protect and secure the airway with immediate or early endotracheal intubation Aggressive iv hydration should be used to support low BP in pts with hypothermia and hypotension |
|
|
Diphenhydramine
|
is highly sedating and has anti-cholingergic properties. Because of the effect of diphenhydramine on the level of alertness and coordination, use of the drug must be discontinued before performing coordinated tasks such as driving, working on machinery, flying planes or diving.
|
|
|
HCV infection
|
In pt with (+) ELISA-anti-HCV antibodies, there are several potential explanations: persistent hepatitis C infection, cleared infection (+ anti-HCV antibodies + normal liver function tests + negative HCV RNA)or false positive ELISA result. The diagnosis should be confirmed by high-specificity testing (usually HCV RNA). The positive predictive value of ELISA-anti HCV in a pt with a low risk profile (no previous transfusions, no IV drug use or sexual promiscuity) and normal ASL/ALT is low.
|
|
|
Scleroderma
|
A ‘sticking sensation’ in the throat (dysphagia) accompanied by heartburn
The absence of peristaltic waves in the lower two-thirds of the esophagus + a significant decrase in lower esophageal sphincter (LES )tone. |
|
|
Prophylaxis for stress ulcers
|
ICU pt with coagulopathy, a h/o GI bleeding in the last year, mechanical ventilation >48h, or 2 of the following
Sepsis ICU admission > 1w Occult GI bleeding > 6d Glucocorticoid therapy A proton pump inhibitor is DOC if the pt is able to take medications via an enteral tube H2 receptor antagonists are DOC for pt requiring iv medications |
|
|
Enteral feeding
|
feeding is preferred to parenteral feedings for pt who have a functioning GI system. The standard composition of 30kcal/kg/day and 1g/kg/day of protein is satisfactory for most pt with adequate baseline nutrition.
|
|
|
Spontaneous bacterial infection
|
infection can develop in up to 50% of pt who are hospitalized for acute variceal bleeding, therefore these pt should be treated prophylactic with antibiotics (Fluoroquinolone such as ofloxacin, norfloxacin or ciprofloxacin for 7-10d)
The most common complication is the development of infection (UTI, SBP, respiratory infection, aspiration pneumonia or primary bacteremia) |
|
|
Toxic megacolon due to UC
|
Abdominal X-ray is for diagnosis. CT is best for detecting early complication.
Findings of peritonitis may be absent in toxic megacolon, so the lack of rebound tenderness or guarding on the pt’s exam does not exclude the diagnosis. The transverse colon: most prominent dilation, > 6cm in diameter, multiple air-fluid levels Nonsurgical treatment is attempted in the absence of perforation. Any medications that could decrease peristalsis (anticholinergics ,5-ASA, opiates) should be held. 5-ASA should not be used acutely in pt with inflammatory bowel disease complicated by toxic megacolon. Start the pt on glucocorticoids to decrase the severity of underlying inflammatory bowel disease. Note that management depends on the underlying cause of toxic megacolone and that glucocorticoids should be avoided in pt with toxic megacolone secondary to C. difficile or other infections. The pt should also receive aggressive fluid resuscitation |
|
|
ALS
|
that progresses to severe muscular weakness, dysarthria, dysphagia and dyspnea, The dysphagia is irreversible and must be treated through percutaneous gastrostomy(PEG) tube placement. NGT (nasogastric tube) produces discomfort, can affect the pt’s breathing or speech, can aggravate the pt’s dyspnea and leads to sinusitis.
|
|
|
Pt with peritonitis
|
Pt with peritonitis tend to lie flat and motionless to limit irritation of the peritoneum, in contrast to pt with renal colic who tend to writhe in pain.
|
|
|
The APACHE II score
|
is the scoring system of choice to predict the severity of acute pancreatitis given its good predictive values and ability to be calculated at admission.
The Apache II score accounts for blood pressure, oxygenation, temperature, respiratory rate, creatinine, GCS, etc, and is a better predictor of survival. A HCT of 44% or greater at admission and failure to decrease at 24 hours is also an excellent predictor of necrotizing pancreatitis and multi-organ failure. Ranson’s criteria are the oldest scoring system, the predictive value is lower and score can only be calculated after the pt has been hospitalized for 48h. CT scan is usually NOT necessary to make a diagnosis of pancreatitis, but it can be helpful in assessing it severity and complications. A contrat-enhanced CT is indicated to assess for pancreatic necrosis or other complications (Intravenous contrast-enhanced CT distinguishes between edematous and necrotizing pancreatitis, since areas of necrosis and exudates do not enhance). Pt in whom >30% of the pancreas is necrotic may benefit from prophylactic antibiotics, with imipenem and meropenem x 7-10d being the most commonly used agents. Isolated gastric variecs (without evidence of esophageal varices) due to splenic vein thrombosis can be seen as a complication of chronic recurrent pancreatitis. The splenic vein runs along the posterior surface of the pancreas, and can get directly inflamed and thrombosed due to recurrent pancreatic inflammation. |
|
|
Drug induced pancreatitis
|
Furosemide and thiazide diuretics can cause acute pancreatitis.
AIDS pt – didanosine, pentamidine Pt with h/o seizures/bipolar disorder – valproic acid Pt on antibiotics – metronidazole, tetracycline Pt with inflammatory bowel disease --- sulfasalazine, 5-ASA Pt on immunosuppressive agents – azathioprine, L-asparaginase |
|
|
Acute variceal bleeding
|
Endotracheal intubation is indicated in unresponsive pt with a large amount of hematemesis due to aspiration risk, followed by assessment of breathing and circulation. Upper endoscopy should be performed early on since it may be both diagnostic and therapeutic.
In acute variceal bleeding an endoscopic intervention is the most effective therapy and should be reattempted in the event of recurrent bleeding. If a second attempt at banding fails, surgical shunting or transjugular intrahepatic portosystemic shunt (TIPS) procedure should be considered. Nonselective beta-blockers such as nadolol and propranolol (↓pressure in the portal venous system)can be used in primary and secondary prevention of esophageal variceal hemorrhage, Oral nitrate medications may also be used as a part of the medication regimen for variceal bleeding prevention. |
|
|
rebleeding after gastric surgery for peptic ulcer treatment
|
There is a significant rate of rebleeding after gastric surgery for peptic ulcer treatment. Truncal vagotomy with partial antrectomy has a recurrence rate of 5-10% after a mean follow-up of 3.5y. The preferred methold to confirm the source of bleeding is upper GI endoscopy because it also has therapeutic applications such as photocoagulation or local injection of vasoconstrictor agents.
|
|
|
Side effects of herbal remedies
|
Kava(for anxiety) --- liver injury, hepatitis, cirrhosis, liver failure 卡瓦根(旧时用作利尿药)
Gingko --- bleeding, Stevens-Johnson syndrome – psychosis Aconite --- cardiotoxic: arrhythmia, hypotension 乌头毒草;从乌头草的根中所提炼的强心止痛剂 |
|
|
hepatitis B virus infection
|
Stable and otherwise healthy adults who present with jaundice + ↑ALS + ↑AST can be evaluated on an outpatient basis. Admission to the hospital for observation is appropriate only if there is concern that the pt’s condition will worsen rapidly in the near future.
Acute hepatitis B virus infection is a subclinical or anicteric syndrome in 70% of pt, with the remaining 30% complaining of symptoms such as anorexia, nausea, jaundice, and RUQ discomfort. Treatment of acute hepatitis B consists of supportive measures. Fewer than 5% of adults stricken with acute hepatitis B infection will go on to develop chronic hepatitis B whereas 90% of infants that acquire acute hepatitis B perinatally will go on to develop chronic hepatitis B. |
|
|
Triple drug therapy with a PPI,
|
Triple drug therapy with a PPI, clarithromycin and amoxicillin/metronidazole (metronidazole in case of penicillin allergy) X 2w is the regimen of choice for the eradication of H. pylori infection. There is a high prevalence of H. pylori resistance to clarithromycin and metronidazole in the US.
1. use different combination of drugs/antibiotics for another 2w 2. Quadruple therapy: PPI+bismuth+tetracycline+metronidazole, take with meals for 2w Confirmation of H. pylori eradication is recommended for pt with ulcers or ongoing dyspepsia. Either urea breath or fecal antigen testing can be used after 4w to confirm H. pylori eradication (urea breath test is more accurate than fecal antigen testing). 1w is too soon for urea breath test and may result in a false positive test. H. pylori serology should not be used since it may remain positive a year or more after eradication. |
|
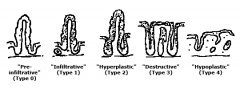
Celiac disease
|
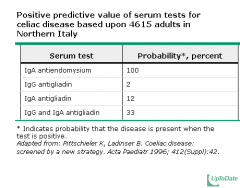
Diarrhea with bulky, foul-smelling, floating stools due to steatorrhea and flatulence.
Growth failure in children, weight loss, severe anemia, neurologic disorders from deficiencies of B vitamins and osteopenia from VitD/Ca deficiency Schematic representation of the five main lesions associated with gluten sensitivity. The lesions range in histologic severity from a mild alteration characterized by increased intraepithelial lymphocytes (type 0 lesion) to a flat mucosa with total mucosal atrophy, complete loss of villi, enhanced epithelial apoptosis and crypt hyperplasia (type 3 lesion). The type 4 lesion is seen in T cell lymphoma. |
|
|
Rapid stool tests to dectect C. difficile toxins
|
have very high specificity (close to 100%); however their sensitivity is about 70-80%. Repeating the test may be necessary in pt in whom the pretest probability of C. difficile infection is high and an initial test result is negative
Tx: iv/po metronidazole po vancomycin Recurrent CDI often results from reinfection with the same or a different strain of C. difficile. Studies using molecular methods have shown that up to one-half of recurrent episodes are reinfections rather than relapses of infection with the original strain. Resistence is very rare. For first replapse: metronidazole. |
|
|
GERD
|
Heartburn, regurgitation and dysphagia (It is important to identify the non-classical presentation of GERD, including periodic retrosternal chest pain that can mimic angina )
Chest pain of hearburn: uncomfortable squeezing/burning sensation in the retrosternal chest that radiates toward the back, neck, jaw or arms. The pain may resolve spontaneously or after consumption of antacids and usually occurs postprandially, can awaken pt from sleep and worsens with emotional stress. The resulting erosive esophagitis may cause transitory dysphagia, which may result in a peptic stricture if left untreated. Peptic stricture formation is a well-known complication of GERD that can cause obstructive dysphagia. A trial of proton pump inhibitors >8w should be used in pt who have failed other conservative therapies (lifestyle/dietary modifications, antacids, non-prescription H2 blockers). Endoscopy should be done early if the pt complains of dysphagia, odynophagia, significant weight loss and GI bleeding. If fails a trial of proton pump inhibitors → refer to a gastroenterologist for an upper endoscopy |
|
Colonic Adenocarcinoma
|
Management of adenocarcinoma arising in a polyp is usually different from other forms of colonic adenocarcinoma. If the invasive adenocarcinoma is in the head of the polyp, the margins are uninvolved, the lesion is well-differentiated, and there is no lymphovascular invasion then the pt can undergo nonoperative management, however consultation is typically required with the pt on a case by case basis. In pt who are managed nonoperatively, follow up colonoscopy should be performed in 3 months to exclude residual/recurrent disease. Subsequent follow ups should be obtained at 1, 4, and 9 years following the initial polyp resection as these pt are at an ↑risk of having colonic adenocarcinoma in the future.
Colonic polyps: Masses protruding into gut lumen →sawtooth锯齿appearance. 90% are non-neoplastic. Often rectosigmoid. can be tubular or villous. Adenomatous polyps are precancerous. Malignant risk is associated with ↑size, villous histology, ↑epithelial dysplasia. Precursor to colorectal cancer (CRC). The more villous the polyp, the more likely it is to be malignant (VILLous = VILLainOUS) . Polyp symptoms- often asymptomatic, lower G I bleed, partial obstruction, secretory diarrhea. Studies have shown that 30-50% of pt with one adenoma will have at least one another adenoma at a different site (synchronous adenoma). All pt with adenomatous polyps found on screening sigmoidoscopy should have a complete colonoscopy for detection of synchronous adenomas. Examination of the complete large bowel and removal of all the adenomas is an important step in reducing the risk of subsequent cancer, therefore the pt should be screened with a complete colonoscopy to detect and resect all synchronous adenomas. No further treatment is necessary if all the following criteria are fulfilled: 1. The polyp is considered to completely excised 2. There is accurate determination of the depth of invasion, grade of differentiation and completeness of excision of the carcinoma 3. The cancer is not poorly differentiated 4. There is no vascular or lymphatic involvement 5. The margins of the excision and the stalk of a pedunculated adenoma are not involved. Invasion of the stalk of a pedunculated polyp is not an unfavorable prognostic finding, as long as the cancer do not extend to the margin of the stalk resection. A three-year interval for surveillance colonoscopy is safe and cost-effective for the majority of pt with adenomatous polyps (> 2 adenomas, > 1cm adenoma, a villous adenoma or and adenoma with high-grade dysplasia). The surveillance intervals can be extended to 5 years if no adenomas are detected at the three-year follow-up colonoscopy. Number/Size/Histopathology Surveillance colonoscopy Hyperplastic polyps 10 years 1 or 2 small (< 1cm) tubular adenomas with no high-grade dysplasia 5 years ➢ > 2 adenomas ➢ High-grade dysplasia ➢ Villous features ➢ Any adenoma > 1cm in size 3 years Adenomatous colon polyps are neoplastic lesions which have the potential to develop into colonic adenocarcinomas, make up 2/3 of polypoid lesions in the colon Hyperplastic polyps rarely if ever develop into malignancy and should NOT affect recommendations for future colonoscopic surveillance. Colonoscopy is the initial test of choice in pt with iron-deficiency anemia and + fecal occult blood test. Barium enema has lower sensitivity and do not offer the option of simultaneous diagnostic and therapeutic intervention (biopsy or polyectomy). In pt with no obvious pathological findings on colonoscopy, upper GI endoscopy should be performed. |
|
|
Familial adenomatous polyposis (FAP)
|
Autosomal dominant
H/o a first degree relative with early onset colon cancer, however up to 1/3 of pt with FAP have no such family history due to a new mutation Polyposis typically begins in the 2nd/3rd decade of life, > 100 adenomatous polys on colonoscopy, symptoms are vague and nonspecific Genetic testing for mutations in the APC gene is to confirm the diagnosis The vast majority of these pt → colorectal carcinoma by age 50 if colectomy is not performed. Tx: proctocolectomy or total colectomy with ileorectal anastomosi before age 20. At risk of developing extracolonic neoplasms. Both gastric and duodenal adenomas/carcinomas are more prevalent among pt with FAP so upper GI endoscopy at this time would be warranted. Nearly all pt with FAP develop colon cancer by the age of 45, so colectomy is generally made at the time of diagnosis (prophylactic colectomy). |
|
|
Wireless video endoscopy
|
Wireless video endoscopy is an effective tool to diagnose some small bowel disease because visualization of the majority of the small bowel mucosa is not possible with push endoscopy. Endoscopy is preferred for the dx of esophageal and stomach disease.
A video capsule is taken by the pt and video recording is traced by the outside sensors. It can be helpful to identify the source of small bowel hemorrhage, tumors, ulceration and inflammatory conditions. The images acquired are of excellent resolution and have an 8:1 magnification, which is higher than that of conventional endoscopes. Limited views of the esophagus, stomach and cecum are obtained by this technique, therefore, in no way can it currently replace endoscopy for the dx of esophageal and stomach disease. Complications of wireless video endoscopy are rare. |
|
|
Celiac disease
|
Celiac disease is related to an increased risk of developing intestinal lymphoma. This diagnosis must be suspected in any pt with celiac disease who p/w GI symptoms (abdominal pain, weight loss and diarrhea) despite adherence to a gluten-free diet. The jejunum is most commonly affected and the tumors are usually nodular or ulcerative. Some pt may p/w perforative peritonitis.
Tx: surgery + chemotherapy, high relapse + poor prognosis |
|
|
Cholecystectomy
|
Pt who have undergone cholecystectomy do not need to change their dietary habits, Half of them may have transient and mild episodes of diarrhea, flatulence or bloating that will be self-limited.
Biliary injuries from laparoscopic cholecystectomy can present with either biliary leak or obstruction → ascending cholangitis (Charcot’s triad: fever + jaundice + right upper quadrant pain) Suppurative cholangitis: Reynold’s pentad: fever + jaundice + right upper quadrant pain + hypotension + confusion (Tx: fluid resuscitation + antibiotic + biliary drainage) |
|
|
Angiodysplasia (vascular ectasia膨胀)
|
The most common cause of massive lower GI bleeding in elderly pt is angiodysplasia or diverticulosis (the two entities frequently coexist). Angiodysplasia is associated with aortic stenosis, Von Willebrand disease and ESRD. The cause of angiodysplasia may be related to degenerative changes associated with aging and to intramuscular hypertrophy that obstructs submucosal veins.
Angiodysplasias are composed of ecstatic 扩张的, dilated, thin-walled vessels that are lined by endothelium alone or endothelium along with small amounts of smooth muscle. Angiodysplasia is usually diagnosed by endoscopy being done to evaluate GI bleeding, but in some cases, radiographic imaging or surgery may be required for detection. DD Diverticulosis 憩室病is also a common cause of massive colonic bleeding (erosion of artery) and this has been attributed to ruptured vasa recta wither at the apex or neck of a diverticulum. The bleeding is generally painless and can be massive. Diagnosis can be made by colonoscopy. Diverticulitis can also cause bleeding as a result of superficial mucosal ulcerations but usually the bleeding is mild, fever + abdominal pain + mild bleeding. It was diagnosed with a CT scan (colonic wall thickening and stranding of mesenteric fat, complications of diverticulitis such as perforation, fistulas and abscesses, determine the need for surgery or percutaneous CT-guided drainage). A change to a diet rich in fiber is recommended to prevent recurrences. A colonoscopy is contraindicated in the acute condition. Colon cancer: occult GI bleeding + anemia Ulcerative colitis: bloody diarrhea + mucus + mild abdominal cramping, dx is made by endoscopy and barium enema |
|
|
Mallory-Weiss tear
|
Hematemesis preceded by a bout of retching/vomiting
Risk factor: Hiatal hernia食管裂孔疝(40-100% of pt with Mallory-Weiss syndrome), retching/vomiting, straining, hiccupping, coughing, primal scream therapy, blunt abdominal trauma, cardiopulmonary resuscitation and endoscopy Dx: Endoscopy is the gold standard : a single longitudinal tear at the gastro-esophageal junction Endoscopy also allows for therapeutic interventions (i.e. thermal coagulation, sclerotherapy and band ligation) to stop active bleeding In pt with Mallory-Weiss tear who are not actively bleeding, observation and supportive care are typically necessary. |
|
|
Acute ischemic colitis
|
H/o HTN, hypercholesterolemia, CAD
Abdo pain followed by bloody diarrhea Most vulnerable areas are watershed areas which include the splenic flexure and rectrosigmoid junction. Elevated WBC, X-rays and sigmoidoscopies: mucosal edema + mucosal ulcerations (edematous/dilated transverse colon) |
|
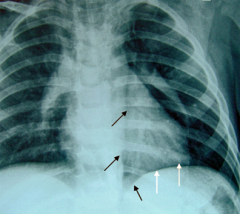
Esophageal perforation (Boerhaave’s syndrome)
|
Acute chest pain following episodes of repeated vomiting
Most tears occur in the distal third of the esophagus → pleural effusion Pneumomediastinum (the radiologic finding of a radiolucent band adjacent to the cardiac border) and pneumothorax can be part of the presentation. The best diagnostic text for esophageal perforation is an esophagogram with water-soluble contrast (90% of the cases).If the test is negative but the clinical suspicion is high, barium contrast can be used. Water-soluble contrast is preferred to barium because the latter can produce further mediastinal irritation and injury. CT scan of the chest is helpful but may not detect small tears or ruptures. Urgent management is needed because of the risk of mediastinitis, which carries a mortality rate of > 40% if not properly diagnosed within the first 24h. In this radiograph of a child with pneumomediastinum, the following characteristic signs are seen: 1) The "continuous diaphragm sign", in which the mediastinal gas is seen as a thin lucent line outlining the superior surface of the diaphragm and separating it from the heart (white arrows). 2) "Naclerio's V sign", in which the gas outlines the lateral margin of the descending aorta and extends laterally over left hemidiaphragm (black arrows) |
|
|
Dysphagia
|
1. oropharyngeal dysphagia: cough with swallowing, referred pain (ear pain), drooling, difficulty initiating a swallow, a cervical location of symptoms
2. esophageal dysphagia: symptoms several sec after a swallow with complaints often referable to the parasternal region. |
|
|
Lactose intolerance
|
It can be diagnosed with the lactose breath hydrogen test because free lactose is fermented by colonic bacteria to form fatty acids and hydrogen gas. The test involves measuring the amount of hydrogen gas exhaled in the few hours after consuming a lactose-containing beverage. In preparation for the test, pt should fast for 8h.
The test is begun by giving oral lactose in the fasting state, at a usual dose of 2 g/kg (maximum dose, 25 g). Breath hydrogen is sampled at baseline and at 30-minute intervals after the ingestion of lactose for three hours. The post-lactose and baseline values are compared. We generally consider a breath hydrogen value of 10 ppm (parts per million) as normal. Values between 10 and 20 ppm may be indeterminate unless accompanied by symptoms, while values over 20 ppm are considered diagnostic of lactose malabsorption. |
|
|
Fecal incontinence
|
Fecal impaction (a solid, immobile bulk of human feces that can develop in the rectum as a result of chronic constipation.) is the most common cause of fecal incontinence in elderly pt. The most appropriate initial treatment is to disimpact the stool and empty the colon until there is no return of stool by using enemas and suppositories栓剂.Suppositories are frequently used to ensure complete emptying. Colonoscopic decompression is performed in pt who have failed conservative management.
|
|
|
Evaluating persistent/nonresolving pneumonia/pulmonary infiltrates
|
The best diagnostic test for endobronchial obstructive lesion is flexible bronchoscopy. HRCT scan is an alternative, but it does not provide confirmatory information.
|
|
|
ARDS --- non-cardiogenic pulmonary edema
|
Criteria for diagnosis
1. A pulmonary capillary wedge pressure < 18 mmHg 2. PaO2/FiO2 < 200 mmHg regardless of the PEEP level 3. Diffuse bilateral infiltrates on chest X-ray It can occur secondary to sepsis, pneumonia, severe trauma, burns, drowning or pancreatitis. The presentation is sudden. Oxygen requirements increase very rapidly. In contrast to heart failure, pt with ARDS will typically have clear lungs on exam but will show diffuse, bilateral infiltrates on the chest X-ray. |
|
|
ARDS
|
The goals of mechanical ventilation in ARDS include
Low tidal volumes (8 ml/kg of ideal body weight or less) to achieve low plateau pressure Optimize PEEP to achieve acceptable oxygenation (PaO2 >55 mmHg, O2 saturation > 90%,) A normal or slightly acidic pH (permissive hypercapnia) One this is achieved, the pt should be weaned as soon as possible in order to avoid complications such as barotraumas, ventilator-associated pneumonia, prolonged sedation and hypotension. ARDS: 35-40% mortality rate Mechanical ventilation that delivers lower tidal volumes (<6 ml/kg) and limits plateau pressure (< 30 cm H2O) has been shown to be relatively more effective to ↓mortaility |
|
|
Pulmonary embolism
|
Fever can be present in up to 14% of pt with pulmonary embolism and is usually low-grade. The clinical picture can be confusing for the possible presence of pneumonia given that pt may also have pulmonary opacities from infarction or atelectasis as well as an elevated WBC count secondary to the pulmonary embolism itself. Obtaining blood cultures at this time is reasonable but initiation of antibiotic therapy is unnecessary unless the patient’s condition worsens.
A lower extremity venous U/S is performed in pt for whom there is concern foe PE but in whom CT angiography.is contraindicated. ↑troponin levels --- 30-50% of pt with large PE, secondary to acute right heart overload, related to a higher risk of death. Generally resolve within 2 days, in contrast to the more prolonged elevations seen in MI. The most important prognostic factor in PE is hypotension, which is seen in pt with massive emboli. |
|
|
Septic pulmonary embolism
|
Complication of IV drug abuse, result from septic throbophlebitis (a painful subcutaneous mass in the right cubital area) and/or tricuspid endocarditis.
|
|
|
Airway hyperreactivity
|
Cough induced by forced expiration is characteristic of airway hyperreactivity and is usually suggestive of asthma. However this presentation has also been described in some pt with COPD who can occasionally have an overlapping condition with asthma.
|
|
|
Clues to a pt’s clinical deterioration
|
H/o prior intubation
Exhaustion or extreme fatique Diaphoresis Change in consciousness: confusion and drowsiness Use of accessory muscle Presence of suprasternal retractions Depressed respiratory drive Marked tachycardia Pulsus paradoxus PaCO2 > 40 mmHg Peak expiratory flow rate < 25% of the normal predicted All pt with the above signs and symptoms of impending respiratory failure should be immediately intubated to secure and protect the airways. |
|
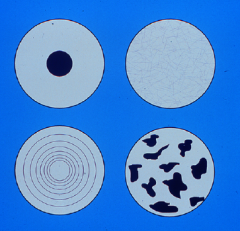
Benign nodule on chest X-ray/CT
|
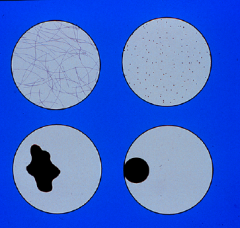
Popcorn/concentric/laminated/central/diffuse homogenous calcification
Popcorn calcifications are characteristically seen on radiographic imaging in pt with pulmonary hamartoma Schematic representation of different patterns of benign calcification. In clockwise orientation from top left: target, diffuse, popcorn, and lamellated calcification. Schematic representation of different patterns of malignant calcification. In clockwise orientation from top left: reticular, psammomatous (punctate), eccentric, and amorphous calcification. Schematic representation of different patterns of the margin of pulmonary nodules. In clockwise orientation from top left: smooth, scalloped圆齿状的, corona radiata辐射冠, and spiculated. Benign pattern of calcification in a solitary pulmonary nodule with characteristic popcorn configuration suggestive of a hamartoma. Spiculated border in a malignant solitary pulmonary nodule located in the right middle lobe. Smoker with obvious centrilobular emphysema. A review of all available old chest X-ray is an important initial part of the diagnostic workup of pt with a solitary pulmonary nodule. A high-resolution CT scan is extremely useful in defining the morphology, margin and border of the lesion. It demonstrates the pattern of calcification within the nodule and identified any mediastinal lymph node involvement and small pleural effusions. An irregular/speculated border and the presence of eccentric, reticular or punctuate calcifications within the lesion. Video-assisted thoracoscopic surgery (VATS) with excisional biopsy should be performed for the removal and definite diagnosis of a peripheral located pulmonary nodule suspicious for malignancy. |
|
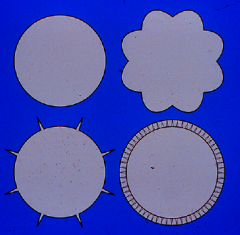
Benign nodule on chest X-ray/CT
|
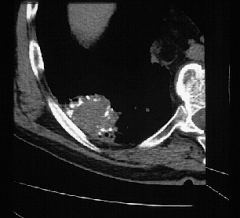
|
|
|
Benign nodule on chest X-ray/CT
|
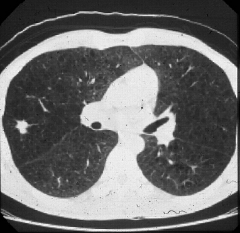
|
|
|
Hemoptysis
|
Chest X-ray abnormalities may suggest a variety of specific causes in pt with hemoptysis, ranging from malignancy to focal infection (e.g. pulmonary tuberculosis) to heart disease (e.g. mitral disease). Acute bronchitis is the most common cause of hemoptysis. A trail of antibiotic therapy is warranted while the pt is being evaluated for endobronchial lesions with bronchoscopy and CT scan.
|
|
|
Pulmonary artery hypertension
|
Pulmonary artery hypertension is often difficult to distinguish from congestive heart failure or coronary artery disease based on history alone as pt typically have dyspnea or chest pain on exertion due an inability to increase cardiac output with exercise.
Passive hepatic congestion leading to abdominal pain or anorexia can help to suggest right-sided heart dysfunction. The loud S2 and prominent pulmonary arteries on chest radiography are suggestive of PAH. The best test is an echocardiogram through which an estimate of pulmonary artery pressure can be made. Echo is also able to evaluate for right ventricular hypertrophy, right atrial size, finding of right ventricular failure and valvular incompetence. A high resolution CT of the chest is indicated to evaluate for secondary causes of pulmonary hypertension (mitral stenosis, COPD, polycythemia vera, chronic pulmonary emboli, interstitial lung disease). Echo should be obtained first. Most accurate test: right heart catheterization with↑pulmonary artery pressure. |
|
|
Asthma exacerbation
|
Early administration of systemic steroids is essential in managing moderate to severe asthma exacerbation.
The decision to admit a pt may be considered based on the individual clinical evaluation and the peak flow reading, if the value is at least 40-50% lower than the pt’s baseline. |
|
|
Paradoxical emboli
|
are those that originate in the venous system and enter the arterial system via an intracardiac shunt. They are a more common cause of stroke in the young than in the elderly. They can be diagnosed with an Echo and bubble study.
|
|
|
Hepatic hydrothorax
|
Usually presents as a right-sided transudative pleural effusion (pleural fluid protein/serum protein <0.5 and pleural fluid LDH/serum LDH < 0.6 and pleural fluid LDH < 2/3 of upper limit of the normal serum LDH) in pt with cirrohosis and ascites. It is thought to be caused by the passage of ascetic fluid through small diaphragmatic defects, although the exact mechanism is not known.
Tx: similar to the treatment of ascites: sodium restriction and diuretics |
|

Preoperative pulmonary risk assessment
|
It is important to perform preoperative pulmonary risk assessment in all pt who will be undergoing major surgical procedures (reduce postoperative pulmonary complications and length of stay in the hospital). A detailed history and PE is the first step (most important tools) in the evaluation of these pt. Significant risk factors (Age, Chronic lung disease, Asthma, Smoking General health status, Obesity, Obstructive sleep apnea, Pulmonary hypertension, Heart failure, Upper-respiratory infection, Metabolic factors) should be identified. Any history suggesting unrecognized chronic lung disease or heart failure, such as exercise intolerance, unexplained dyspnea, or cough, requires further consideration. In a pt with a known , stable, COPD and no evidence of exercise intolerance, routine testing with arterial blood gas analysis, pulmonary function testing, or spirometry is not indicated.
All candidates for lung resection should have preoperative pulmonary function tests performed. A careful history and physical examination are the most important tools for preoperative risk assessment in evaluating patients for potential postoperative pulmonary complications. Attention should be paid to symptoms that suggest the possibility of occult underlying lung disease, including exercise intolerance, cough, and unexplained dyspnea. In addition, the clinician should seek a history of the risk factors summarized above. The Canet risk index is also a promising tool for risk assessment. A high risk patient will benefit from aggressive strategies to reduce pulmonary complications (algorithm 1). (See "Strategies to reduce postoperative pulmonary complications".) In addition to the history and physical examination, a chest x-ray should be obtained in patients undergoing high risk surgery who are over age 50 years, or if cardiac or pulmonary disease is suggested by the clinical evaluation, unless one has been obtained in the past six months. Pulmonary function tests should be reserved for patients with uncharacterized dyspnea or exercise intolerance and for those with COPD or asthma where clinical evaluation cannot determine if airflow obstruction has been optimally reduced. The benefit of PFTs in other situations is unproved. There is no role for preoperative arterial blood gas analyses to identify high risk patients or to deny surgery. |
|
|
Allergic bronchopulmonary aspergillosis (ABPA)
|
No single diagnostic test to confirm ABPA
The diagnosis is usually made by clinical, radiographic and immunologic criteria 1. A h/o asthma 2. Immediate skin prick test reactivity to Aspergillus antigen A skin prick test for Aspergillus should be performed initially in all pt suspected of having ABPA. (+)→serum total IgE levels + precipitating serum Ab to Aspergillus fumigatus be measured (-): exclude ABPA 3. Precipitating serum antibodies to Aspergillus fumigatus 4. Serum total IgE concentration > 1000 ng/mL 5. Peripheral blood eosinophilia > 500 /cubic millimeter 6. Lung infiltrates, usually involving the upper lobes 7. Central bronchiectasis When airway of pt become colonized with Aspergillus, the intense IgE and IgG mediated immune response leads to the characteristic recurrent episodes of fever, malaise, cough with brownish mucoid expectoration, wheezing and symptoms of bronchial obstruction. Oral corticosteroids are the mainstay of therapy for pt with ABPA. |
|
|
Diaphragmatic paralysis
|
can lead to orthopnen, which can be easily confused with congestive heart failure. The most common cause of bilateral diaphragmatic paralysis are neurologic diseases such as ALS (presence of neurological signs and symptoms should be sought elsewhere in the body such as lower extremity muscle atrophy and tongue fasciculation)
|
|
|
Etomidate
|
Etomidate rapidly inhibits the γ-aminobutyric acid receptor to block neurologic excitation. It is the preferred agent in pt with cardiovascular compromise because it provides the most hemodynamic stability compared to other agents (e.g. benzodiazepine, barbiturate, ketamine and propofol).
|
|
|
Hypocalcemia after blood transfusion
|
Pt with renal failure, hepatic failure, hypothermia or shock who receives blood transfusion have a high risk of hypocalcemia due to their inability to metabolize citrate, which is concomitantly transfused with every blood transfusion. The measured serum calcium levels may remain normal despite this occurrence because the deficit of ionized calcium is not reflected in the total calcium levels. Prophylactic administration of at leat 10 cc of 10% calcium gluconate is therefore recommended for every 500 ml of packed red blood cells transfused.
|
|
|
Swallow evaluation in stroke pt
|
Stroke pt are often at risk for oropharyngeal dysphagia,and possibly aspiration, particularly those with symptoms of dysarthria. In the setting of acute stroke, such pt should not be given anything by mouth until a swallow evaluation can be performed.
Dysphagia is very common after stroke and is a major risk factor for developing aspiration pneumonia. Bedside swallowing evaluation with speech therapy followed by barium swallow study if needed. The upright supine position is thought to be the most protective and is used most frequently to prevent the risk of aspiration in pt with impaired consciousness or dysphagia due to neurological disorders. The recumbent position平卧的 predisposes the pt to a high risk of aspiration and should be avoided if possible. DVT and subsequent PE is a common cause of morbidity and mortality in pt with acute stroke, particularly in pt with dense hemiparesis. Subcutaneous low-dose heparin or LMWH for >2w should be used for prophylaxis in most pt with acute stroke. HTN up to a blood pressure of 220/120 should generally be permitted in pt with acute ischemic stroke. After the dx of an acute stroke is make and appropriate treatment is started, further evaluation is necessary to determine the cause of the cerebral infarct 1. MRA, CTA: evaluate the carotids and intracranial vasculature , duplex U/S: evaluate the carotids alone 2. ECG: Dx MI → intracardiac thrombus → embolus 3. TTE/TEE/cardiac MR: detect intracardiac thrombus Medical management of TIA consists of aggressive treatment of atherosclerotic risk factors as well as antithrombotic medication. Treatment with either aspirain or clopidogrel is comparable. Warfarin or an aspirin/clopidogrel combination have not been proven to be more efficacious than aspirin or clopidogrel alone but have a much higher bleeding risk. There is evidence to suggest that clopidogrel may be superior to aspirin in the secondary prevention of stroke. |
|
|
Depression in PD
|
Depression affects up to 50% of pt with Parkinson’s disease. It can be easily overlooked because some features may be attributed to the progression of PD. It has a significant impact on disability and should be highly suspected in pt who p/w any of the signs of depression(early morning awakening, poor eye contact). Uncertain cases are usually managed with a trial administration of SSRI antidepressants before changes in the medications for PD are considered.
Treatment of PD There are several problems with prolonged use of Levodopa. There is a theoretical concern that free radicals may be produced from levodopa which may hasten destruction of substantia nigra cells and worsen PD in the long term. There is also an unproven concept that there is a finite period of response to levodopa. Starting a pt on a dopamine agonist such as pramipexole is a strategy since it may help to save levodopa for a later time when the pt’s symptoms are more severe. There may also be a higher incidence of levodopa-related dyskinesia in pt with early onset of PD, therefore dopamine agonist should particularly be considered as the initial treatment in pt 60 years of age or younger. |
|
|
Seizure
|
The first step in the management of a pt with seizures is stabilization with assurance of adequate ventilation and circulation.
Iv lines should be placed Rapid glucose, CBC, electrolytes Urine toxicology screen Presence of slight twitching of mouth and arms suggests that she may be in status epilepticus(a single, unremitting seizure lasting > 5-10min or multiple seizures without an interictal return to baseline). Discountinuation of chronic seizure medicine is a frequent cause of status epilepticus. The metabolic stresses and neuronal damage associated with prolonged status epilepticus cause significant morbidity and mortality, and thus prompt treatment is crucial. Benzodiazepine (lorazepam or less commonly diazepam) are the initial treatment of choice for adult and pediatric pt in status epilepticus. If not effective, phenytoin or fosphenytoin are other possible second line alternatives. |
|
|
Tick paralysis
|
The first symptom of tick paralysis is unsteady gait that progresses to ascending paralysis. The typical presentation is a progressive ascending paralysis that occurs over a matter of hours to days. Fever is not present. Pupillary abnormalities are uncommon. If the pt has a h/o fever or prodromal illness, the dx is unlikely. Finding the attached tick on the skin is the most important diagnostic measure.
Removal of the ticks will cause a substantial improvement of the paresis within several hours. Caused by an attachment of a neurotoxin-secreting tick(Dermacentor andersoni, the Rocky Mountain wood tick and D variabilis-the American dog tick). Symptoms develop 5-6d after a female tick attaches to the pt. DD 1. Guillain-Barre syndrome (GBS), ascending progressive paralysis Occurs in a matter of days to weeks, CSF: increased protein with a normal cell count Tx: The first step is to triage the severity and provide appropriate respiratory support for pt with signs of respiratory failure intravenous immunoglobulin (IVIG) or plasmapheresis Indications for plasmapheresis are: severe flaccid paralysis, bulbar pasly, progressive respiratory failure, and pt on mechanical ventilation. 2. Botulism: descending paralysis, cranial nerves are affected early in the course, papillary abnormalities are common |
|
|
Multiple sclerosis
|
The initial presentation of MS with multiple sclerosis with cranial nerve involvement especially optic neuritis or sensory symptoms , onset at an early age, female sex and a relapsing form of disease carries a good prognosis.
An initial presentation due to involvement of cerebellum, brainstem or pyramidal system signifies a poor prognosis. Internuclear ophthalmoplegia, nystagmus and hemiparesis represent involvement of the brainstem, cerebellum and pyramidal system respectively and are bad prognostic features. Acute exacerbations of MS are treated with iv corticosteroids, Treatment is indicated when there are disabling symptoms. Mild sensory symptoms generally do not require steroids. High dose iv methylprednisolone is used for this purpose, Long-term treatment with steroids provides no benefit and does not prevent future relapses. Oral steroids should NOT be offered to pt who have evidence of optic neuritis. Pt with relapsing MS should be treated with either beta-interferon or glatriamer acetate, The best way of monitoring the disease activity is with a repeat MRI scan 3m after the initial scan. Relapses are decreased during pregnancy and increased in postpartum. Contraception is important if pt are taking disease-modifying agents (both beta-interferon and glatriamer acetate are teratogenic, pt should be advised to stop these medications several months before attempting to conceive, if pt becomes pregnant by chance, the medication should be stopped immediately), however therapeutic abortion is not indicated if they become pregnant with early exposure. |
|
|
Acoustic neuromas
|
Acoustic neuromas result from the proliferation of Schwann cells (schwanomas).
|
|
|
ALS
|
Riluzole is a glutamate inhibitor that is currently approved for the management of amyotrophic lateral sclerosis.
|
|
|
Hypokalemia following VitB12 treatment
|
Treatment with VitB12 in pt with moderate to severe megaloblastic anemia can cause hypokalemia, which can sometimes be very severe and life threatening. Hypokalemia results following uptake of potassium by newly forming RBC. The pt’s serum potassium levels should therefore be monitored during the first 48h. Some physicians transfused packed RBC in pt with severe megalobalstic anemia before VitB12 supplementation to prevent hypokalemia.
|
|
|
Falls in elderly
|
All elderly pts must be asked annually about any episode of falls. If a pt reports a single episode of fall, he should be evaluated with at least one postural stability test. Assessment of gait and balance is important because this determines the need for further evaluation.
The “Get up and go” test is most commonly used to assess postural stability. In this test, the physician instructs the pt to stand up from a chair without assistance, walk a short distance, turn round, return, and sit down again. If the pt is unsteady or has difficulties during the test, further evaluation is necessary. |
|
|
Pseudotumore cerebri (idiopathic intracranial HTN)
|
Women of childbearing age who are overweight, associated with venous sinus thrombosis, OCP and VitA toxicity.Headache is the primary symptom in most pt although the character of the headache is variable and not distinct from other etiologies of headache such as tension headache or migraines.
• Headache (92 percent) • Transient visual obscurations (72 percent) • Intracranial noises (pulsatile tinnitus) (60 percent) • Photopsia (54 percent) 闪光幻觉 • Retrobulbar pain (44 percent) • Diplopia (38 percent) • Sustained visual loss (26 percent) These symptoms, even as a cluster, are not specific for IIH. The primary PE finding in pt with idiopathic intracranial HTN is papilledema, so an ophthalmoscopic examination is the most appropriate next step. The most common signs in IIH are Papilledema, Visual field loss and Sixth nerve palsy Tx: weight loss, acetazolamide, steroids, repeated lumbar puncture rapidly lowers ICP. Ventriculoperitoneal shunt |
|
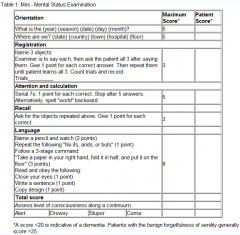
MMSE (mini-mental state exam)
|
A total maximal score on the MMSE is 30 points. A score of less than 24 points is suggestive of dementia or delirium. The test is not sensitive for mild dementia, and scores may be influenced by age and education, as well as language, motor, and visual impairments. In one study, for example, the median MMSE score was 29 for individuals with at least nine years of schooling, 26 for those with five to eight years of schooling, and 22 for those with four years of schooling or less.
Superior sagittal sinus thrombosis is a rare condition that can be associated with trauma, infection, hypercoagulation, vasculitis, nephritic syndrome, severe dehydration and pregnancy. Headache + hemiparesis, papilledema, seizure MRI and MR venography are very useful in establishing the dx. Tx: adequate anticoagulation with heparin even if an area of hemorrhagic infarction is demonstrated on CT (secondary to venous HTN). |
|
|
Clonidine--- HTN in pt with opioid withdrawal
|
The DSM-IV criteria for the dx of opioid withdrawal: > 3 of the following symptoms following reduction in or cessation of a prolonged and excessive opioid use
1. GI symptoms: N/V, diarrhea, abdominal cramps 2. Myalgias 3. Lacrimation or rhinorrrhea 4. Piloerection, sweating or papillary dilation 5. Insomnia 6. Autonomic symptoms: hypotension and tachycardia Clonidine is a centrally acting antihypertensive that is frequently used for the Tx of opioid withdrawal (Clonidine treats high blood pressure by stimulating α2 receptors in the brain, which decreases cardiac output and peripheral vascular resistance, lowering blood pressure.) Pain management: Epidural infusion: Clonidine is reserved for cancer patients with severe intractable pain, unresponsive to other opioid analgesics: Starting dose: 30 mcg/hour; titrate as required for relief of pain or presence of side effects; experience with doses >40 mcg/hour is limited; should be considered an adjunct to opioid therapy |
|
|
Construction apraxia
|
An acquired inability to draw 2-D objects or forms or copy 3-D arrangements of forms or shapes, in absence of motor defects, due to a defect in the non-dominant parietal lobe (right parietal lobe).
Can not copy a picture of a matchstick. Pt have marked difficulty in copying simple line drawings, wearing clothes and appear to struggle while attempting to get into a coat or pants known as dressing apraxia which is seen with bilateral or right-sided parietal lobe lesions. Almost 90% of right-handed pt and 60% of left-handed pt have a left hemispheric dominance for speech and language functions. Damage to the dominant parietal lobe, especially the inferior parietal lobe, p/w Gerstmann syndrome. The pt has difficult in performing simple arithmetic tasks (acalculia), inability to name individual fingers (finger agnosia)., impaired writing (agraphia), alexia and right/left confusion. Aphasia is seen in dominant temporal lobes lesions |
|
|
Trauatic lumbar puncture
|
CSF: RBC > 6000/MM3
↑WBC (RBC:WBC = 750-1000) ↑ Protein, ↑glucose DD 1. SAH: xanthochromia, discoloration of centrifuged CSF due to hemoglobin breakdown, appear 2-4h after RBCs enter the subarachnoid space, present in > 90% of pt within 12h of SAH |
|
|
Life-threatening hemorrhage --- fresh frozen transfusion
|
Life-threatening hemorrhage like traumatic SAH in pt on warfarin therapy should be treated with fresh frozen plasma transfusion
|
|
|
Cluster headache
|
Preventative treatment is important in pt with cluster headaches since by definition the pt can have a large number of headaches over a short period of time. Continually using abortive agents (sumatriptan) may inadvertently lead to rebound headaches or toxicity. Prventative treatment may be tapered after the expected duration of the clusters expires.
Verapamil is the drug of choice for prevention of cluster headaches with a duration of > 2m. Given the cardiac effects of verapamil a screening EKG should be done at higher level doses to assess for heart block or bradycardia. Acute management: 100% oxygen inhalation + sumatriptan, subcutaneous or intranasal Propranolol can be used as prophylaxis for migraine headaches. |
|
|
VitB12 deficiency
|
Intense erythroid hyperplasia occurs in the BM of pt with VitB12 deficiency, but their erythroid precursors do not mature normally and these subsequenctly die in the bone marrow, causing anemia and indirect hyperbilirubinmia.
|
|
|
Bell’s palsy
|
HSV is often implicated as the cause of the disease
Bilateral Bell’s palsy seen with sarcoidosis Tx: corticosteroid + acyclovir (HSV is often implicated as the cause of the disease) Artificial tears, eye patch |
|
Clock drawing test
|
This is a simple test that can be used as a part of a neurological test or as a screening tool for Alzheimer's and other types of dementia.
The person undergoing testing is asked to; Draw a clock Put in all the numbers Set the hands at ten past eleven. Clock drawing is difficult for many dementia pt and serves as a useful test when a full mini mental status exam can not be performed. |
|
|
Lewy body dementia
|
Second most common cause of dementia after AD, Pt must have dementia as well as > 2/3 core clinical features: cognitive fluctuations, visual hallucinations and parkinsonism. Visual hallucinations occurs in 2/3 pt with Lewy body dementia and help to distinguish the condition from AD, which rarely p/w visual hallucinations. Parkinsonism in Lewy body dementia most commonly manifest as bradykinesia, rigidity and gait abnormalities. Tremore is a more rare manifestation.
Physical and chemical restraints should be used judiciously in a combative and disruptive pt. These help prevent injuries and falls and allow for the continuation of medical therapy. Always give haloperidol before you apply restraints. Benzodiazepines have a more rapid onset of action but these can worsen confusion and sedation. They can be used as an adjunct to antipsychotics to reduce extrapyramidal side effects. |
|
|
Phenytoin toxicity
|
The earliest sign is the presence of nystagmus on far lateral gaze. Some other effects include blurred vision, diplopia, ataxia, slurred speech, dizziness, drowsiness. Lethargy and decreased mentation, which progresses to coma. Systemic side effects and neurotoxicity is one of the major limitations to the use of pheytoin..
The serum levels associated with neurotoxicity vary from pt to pt. Some pt can experience side effects even when the measured levels are within the normal therapeutic range. |
|
|
Cerebral palsy (CP)
|
Classified by the pt’s tone – spastic, dyskinetic, mixed or hypotonic
Classified by which limbs are affected – hemiplegic, diplegic or quadriplegic Spastic CP, characterized by spasticity, an upgoing Babinski reflex, and hyperreflexia is most common. Typical history includes premature birth, gross motor delay within the first year of life, and early hand preference. PE in infancy reveals hypotonia but later progresses to spasticity. Hyperreflexia and persistence of primitive reflexes may also be seen. Spastic diplegia is also characterized by a “scissoring gait” and toe walking. Mental retardation and seizures may be associated with CP. |
|
|
Meralgia 股痛paresthetica
|
Entrapment of the lateral femoral cutaneous nerve, which is a small, purely sensory nerve that is a direct branch of the lumbar plexus. It can be compressed as it courses from the lumbar plexus, through the abdominal cavity, under the inguinal ligament and into the subcutaneous tissue of the thigh,
PE: decreased sensation over the anterolateral thigh without any muscle weakness or deep tendon reflex abnormaities. Meralgia paresthetica is a clinical diagnosis. Common causes are obesity and the use of tight garments around the waist. Management: reassurance of the pt and conservative measures such as weight loss and avoidance of tight-fitting garments DD 1. Femoral nerve lesion – anterior and anteromedial thigh paresthesia + quadriceps muscle weakness + decreased knee jerk refex 2. Obturator nerve lesion – sensory loss over the medial thigh + weakness in leg adduction |
|

Caloric reflex test
|

Cold or warm water or air is irrigated into the external auditory canal, usually using a syringe. The temperature difference between the body and the injected water creates a convective current对流气流 in the endolymph of the nearby horizontal semicircular canal. Hot and cold water produce currents in opposite directions and therefore a horizontal nystagmus in opposite directions.[4] In patients with an intact brainstem:
• If the water is warm (44°C or above) endolymph in the ipsilateral horizontal canal rises, causing an increased rate of firing in the vestibular afferent nerve. This situation mimics a head turn to the ipsilateral side. Both eyes will turn toward the contralateral ear, with horizontal nystagmus to the ipsilateral ear. • If the water is cold, relative to body temperature (30°C or below), the endolymph falls within the semicircular canal, decreasing the rate of vestibular afferent firing. The eyes then turn toward the ipsilateral ear, with horizontal nystagmus (quick horizontal eye movements) to the contralateral ear.[5][6] • Absent reactive eye movement suggests vestibular weakness of the horizontal semicircular canal of the side being stimulated. In comatose patients with cerebral damage, the fast phase of nystagmus will be absent as this is controlled by the cerebrum. As a result, using cold water irrigation will result in deviation of the eyes toward the ear being irrigated. If both phases are absent, this suggests the patient's brainstem reflexes are also damaged and carries a very poor prognosis A normal response to caloric stimulation is characterized by a transient, conjugate, slow deviation of gaze to the side of the stimulus (brainstem-mediated), followed by saccadic correction to the midline (cortical correction). A caloric response can not be voluntarily suppressed, therefore the normal oculovestibular reaction strongly suggests psychogenic coma. |
|
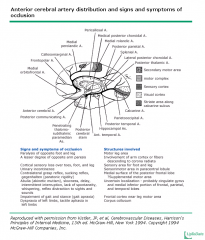
Caloric reflex test
|

|
|
|
Renal cell carcinoma
|
Stage I: confined within the renal capsule --- partial nephrectomy
Stage II: extends through the renal capsule but not beyond Gerota’s fascia --- radical nephrectomy |
|
|
Metformin
|
Metformin should be held temporarily in pt who will undergo radiologic procedures using radio-contrast agents. High-risk pt should be treated with sodium bicarbonate or normal saline infusion and N-Acetylcysteine (Mucomyst) to prevent contrast-induced acute renal failure. Metformin should also be discontinued in sick, admitted pt. NSAIDs should not be used prior to iv contrast administration.
Contraindication of metformin (↑lactic acidosis) 1. creatinine > 1.4 in femae and > 1.5 in male 2. decreased creatinine clearance < 50 ml/min 3. congestive heart failure 4. significant liver disease and alcohol abuse |
|
|
Nephrolithiasis
|
Diagnosis: non-contrast helical CT scan (gold standard)
IVP (more time-consuming, allergic reactions) In pregnant pt or in individuals where you want to avoid the radiation exposure, choose USG A non-contrast helical CT can detect both stones and urinary tract obstruction (Ureteral dilatation), and has become the gold standard for the radiologic diagnosis of stone disease since stones not visualized on KUB or IVP will usually be detected by CT scan . |
|
|
Scleroderma (systemic scerosis)
|
Abnormal deposition of collagen in multiple organ systems.
Raynaud phenomenon + GERD + thickening of the vessel wall and narrowing o vascular lumen in the rena arterioles --- ischemia --- activate the rennin-angiotensin system ---malignant HTN (headache + papilledema) It is important to monitor the BP in scleroderma pt and the presence o HTN should alert the physician to the possibility of scleroderma renal crisis, acute renal failure ACEi is the agent of choice in the treatment of scleroderma renal crisis since it reverse the angiotensin-induced vasoconstriction. Goal should be to reduce BP to baseline over 72h |
|
|
Hepatorenal syndrome
|
DIAGNOSTIC CRITERIA ( diagnosis of exclusion)
Chronic or acute hepatic disease with advanced hepatic failure and portal hypertension • A plasma creatinine concentration above 1.5 mg/dL (133 micromol/L) that progresses over days to weeks. As noted above, the rise in plasma creatinine with reductions in glomerular filtration rate may be minimized by the marked reduction in creatinine production. • The absence of any other apparent cause for the renal disease, including shock, ongoing bacterial infection, current or recent treatment with nephrotoxic drugs, and the absence of ultrasonographic evidence of obstruction or parenchymal renal disease. It is particularly important to exclude spontaneous bacterial peritonitis, which is complicated by acute renal failure that may be reversible in 30 to 40 percent of patients. Urine red cell excretion of less than 50 cells per high power field (when no urinary catheter is in place) and protein excretion less than 500 mg/day. • Lack of improvement in renal function after volume expansion with intravenous albumin (1 g/kg of body weight per day up to 100 g/day) for at least two days and withdrawal of diuretics. Treat: albumin, midodrine, octreotide |
|
|
Polycystic kidney disease
|
Extra-renal maniestations
Hepatic, pancreatic, splenic and pulmonary cysts Cerebral aneurysms, aortic aneurysm Colonic diverticula Mitral valve prolapse Inguinal and abdominal hernia Before considering peritoneal dialysis as a treatment option in pt with adult PKD, it is important to r/o diverticulosis, which can potentially complicated peritoneal dialysis. This can be done by performing a total colonoscopy. |
|
|
ADPKD (autosomal dominant polycystic kidney disease)
|
1:500, accounts for 10% o ESRD pt in the USA.
A progressive decline in renal unction commonly occurs with this disease. Poor prognostic factors for a rapid decline in renal function include severe HTN, male sex, early age of dx and early development of renal dysfunction. ACEi are considered as the drugs of choice for controlling HTN and preventing progression of renal failure in these pt. The ideal goal for BP control in any pt with chronic kidney disease, including ADPKD, is < 130/80mmHg. Routine screening of these berry aneurysms in ADPKD is restricted to pt with a positive family h/o subarachnoid hemorrhage. The most common extrarenal manifestation of ADPKD is hepatic cysts. A higher incidence of colonic diverticula is seen in ESRD pt who are on dialysis. Ultrasonography is the procedure of choice for screening the asymptomatic family members of a pt with ADPKD. The presence of > 3-5 cysts in each kidney is required to make a dx o ADPKD. |
|
|
Percutaneous nephrostomy
|
is the best treatment option for a pt with an obstructing proximal ureteral stone that is complicated by infection and hemodynamic instability.
|
|
|
acute tubular necrosis
|
Suspect acute tubular necrosis in a pt with oliguria following a hypotensive episode. Muddy brown casts and high fractional excretion differentiates acute tubular necrosis from prerenal azotemia.
Always watch out for fluid overload in pt who are oliguric or anuric. D5%W with bicarbonate is generally the fluid of choice in pt who are oliguric, hyperkalemic and acidotic. The indications for dialysis include intractable hyperkalemia, hypervolemia and acidosis. |
|
|
Urethral diverticula
|
diverticula are often secondary to maternal birth trauma or instrumentation of the urethral tract. The condition may present first with postvoid dribbling, followed by dysuria and dyspareunia (three Ds).
Dx: transvaginal U//S and MR |
|
|
HTN and chronic kidney disease
|
Treatment with an ACE inhibitor or ARB is beneficial for pt with HTN and chronic kidney disease who have proteinuria in excess of 500-1000mg/day. The presence o proteinuria affects prognosis and treatment in pt with chronic kidney disease and is considered significant beginning at levels of 500-1000mg.
Secondary treatment with a diuretic in addition to the ACE inhibitor or ARB may be necessary for some pt to meet these goal levels. A non-dihydropyridine calcium channel blocker is the typical choice if a third drug is required because of its anti-proteinuric properties. |
|
|
Renal transplantation
|
The great advances in immunosuppressive therapy have made it possible for any blood relative to be a suitable kidney donor, even in the event of a significant HLA mismatch.
For renal transplantation purposes, the best donor is sibling with no HLA mismatches. Blood relatives with up to 3 HLA mismatches, or non-relatives with a median of four HLA mismatches are also adequate candidates, even though the average possibility of survival (after 10 years) of the renal graft is 20% lower than that obtained from relatives with absolute compatibility. Candidates who are < 14y or > 65y are considered suboptimal or marginal kidney donors. Furthermore, it is not ethical to allow organ donation by children because they are not capable of giving the appropriate consent required. Only in some special situations in which HLA compatibility is critical can the possibility o organ donation by a child be discussed. Cadaveric尸体 donors must have no mismatches in order to be better alternatives than a living donor. A kidney from a cadaveric donor will only be considered to be better than a kidney from a living donor with up to 4 HLA mismatches if the following are both true: 1. The cadaver’s kidney does not have any HLA incompatibility 2. The cadaver did not have any suboptimal or marginal characteristics (no extremes of age, prolonged ischemia or hypotension, vascular injury, chronic diseases, h/o tumors, or significant physiologic derangements) |
|
|
Renal cell carcinoma
|
A renal mass + polycythemia + flank pain + h/o chronic smoking
|
|
|
Isolated elevation in serum creatinine
|
creatinine can be caused by the decreased tubular secretion of creatinine, which is induced by certain drugs (cimetidine, probenecid and trimethoprim).
|
|
|
Retrograde ejaculation
|
Retrograde ejaculation (dry orgasm) occurs in 70% of the pt after TURP (transurethral resection procedure). The bladder neck fails to close after the procedure and enables the sperm to flow backward to the bladder.
Elevation o PSA is seen after an invasive manipulation of prostate, such as prostate biopsy or TURP. The PSA levels usually returns to its normal value within 3-4w after TURP |
|
|
Mixed cryoglobulinemia
|
Nonspecific systemic symptoms: arthralgia, palpable purpura, lymphadenopathy, hepatosplenomegaly and peripheral neuropathy (classical Meltzer’s triad of purpura,, arthralgia and weakness). Most forms of generalized vasculitis cryoglobulinemia commonly involves the kidney due to Cryoglobulin-containing immune complexes.. Initial manifestations of renal disease usually include asymptomatic hematuria, proteinuria and mild elevation of serum creatinine levels. ↓Serum C3, CH50 and C4. Once cryoglobulinemia is suspected, circulating cryoglobuins should be measured to establish the dx.
Chronic hepatitis C infection is the most common cause of acquired essential mixed cryoglobulinemia. All pt p/w vasculitis and elevated cryoglobulin levels should be screened for hepatitis C. Anti-viral therapy is the mainstay of treatment for pt with mixed cryoglobulinemia associated with hepatitis C infection. In pt without renal dysfunction, alpha-intereron and ribavirin are emplyed while in pt with impaired renal function, only alpha-interferon is typically used. |
|
|
Alpha-1 blocker
|
is indicated for pt with HTN and BPH unless the pt has congestive heart failure or develops persistent dizziness (1st-dose orthostatic hypotension). Alpha-1 is also beneficial in pt with type-2 DM because it ↑insulin sensitivity, ↓ LDL and ↑ HDL.
When combined with sildenafil, be given > 4h intervalk |
|
|
Hematuria
|
The first step in the management of all pt with hematuria is to obtain a urinalysis. U/A confirms the presence of hematuria, and differentiates extraglomerular hematuria from glomerular hematuria. Red cell casts, dysmorphic red cells and associated proteinuria are features of glomerular bleeding. Centriugation of urine allows distinction between hematuria, hemoglobinuria and myoglobinuria.
|
|
|
Erectile dysfunction
|
Nocturnal erections (+): pschosocial or hormonal
Nocturnal erections (-): vascular or neurogenic cause Leriche syndrome: impotence, muscular atrophy, buttock claudication Erectile dysfunction may serve as a marker for occult peripheral vascular disease (screen test – ankle brachial index< 0.9 , confirm test – Doppler U/S, CTA or MRA, pt with atherosclearotic disease in one location often have similar disease elsewhere). All three PDE-5 inhibitors: sildenafil, vardenafil and tadalafil work to sustain levels of cyclic GMP within the penile corpora cavernosae to allow men with erectile dysfunction to achieve erections in response to appropriate sexual stimuli.扩管 Six hours from Viagra to throttle time One o the side effects associated with Viagra (sildenifil) is its effect on blue-green color vision.. 3% -- blue haze. Taking higher doses can lead to difficulty in blue-green differentiation. FAA has recommended all pilots to wait or > 6h after taking Viagra before flying a plan |
|
|
Priapism
|
Undesired, painful erection that begins as a nonischemic state and progresses to veno-occlusion, acidosis, anoxia and finally ischemia.
Etiolgoy: thromboembolism (sickle cell anemia, neurogenic dysfunction, neoplasia, trauma, trazodone due to alpha-adrengergic blockade or serotonergic receptor stimulation) An erection > 3h is considered an emergency and requires urologic consultation because permanent damage to the corpora and impotence can ensure. Tx: conservative treatment: ice pack application or medication (↓arterial inflow and ↑venous outflow) First line drug: alpha-adrengeric agonist such as phenylephrine or epinephrine every 5min until detumescence is achieved. |
|
|
Prostatitis
|
Pt presumptively diagnosed with prostatitis should first be evaluated with a urinalysis and urine culture
Dysuria, dull, aching pain in the perineal region and testicles, blood in semen, PE: Edematous /boggy, tender prostate, pyuria and (+) urine culture Nonbacterial prostatitis is more common than acute or chronic bacterial prostatitis. Nonbacterial prostatitis is a noninfectious inflammatory discorder. The clinical presentation is identical to that of bacterial prostitis and the prostatic secretions contain > 20 leukocytes/hpf. Cultures of these secretions are negative. No h/o UTI. Tx: sitz baths and anti-inflammatory medications provide pain relief. Transurethral microwave thermotherapy may also improve symptoms. Acute prostitis: same organisms responsible for UTIs and urethritis. High fever, chills, dysuria, pelvic or perineal pain, clondy urine and urinary frequency, urgency or dribbling. Tender prostate on PE confirms the dx. |
|
|
Analgesic nephropathy
|
Chronic necrosis of the renal papilla with calcification
Acute papillary necrosis → acute renal colic Hematuria, proteinuria and pyuria. Sterile urine culture. A unilateral ureteric calculus will NOT lead to an increase in the BUN and creatinine levels. |
|
|
Pneumonia in children
|
Community-acquired bacterial pneumonia in otherwise healthy children < 5y is most likely caused by S. pneumoniae and can be treated with amoxicillin on an outpatient basis.
Bacterial pneumonia Viral pneumonia onset sudden Gradual apperance High fever, look very ill Mildly ill auscultation Focal , distinctive More diffuse and bilateral X-ray Lobar consolidation Diffuse, bilateral infiltrate Tobramycin and ticarcillin-clavulanate is the preferred empiric antibiotic regiment in cystic fibrosis children experiencing severe pulmonary exacerbations (Pseudomonas aeruginosa, Staph aureus and Haemophillus influenza). For adult community-acquired pneumonia Outpatient: arithromycin/doxycycline/clarithromycin Or respirtory levofloxacin/gatiloxacin/moxiloxacin (comorbidities or antibiotics in the past 3m) Inpatient: cetriaxone + azithromycin Or respirtory levofloxacin/gatiloxacin/moxiloxacin (comorbidities or antibiotics in the past 3m) Ventilator-associated pneumonia: Gram-negative bacilli (Pseudomonas, Klebsiella, E. coli, etc.) or gram-positive bacilli such as methicillin-resistant Staphylococcus aureus (MRSA) Imipenem/meropenem, piperacillin/tazobactam , cefepime Gentamicin and Vancomycin/linezolid |
|
|
Giardia lamblia
|
Asymptomatic carriers o Giardia lamblia are not usually treated, except in specific instances such as in outbreak control for prevention of household transmission by toddlers to pregnant women and pt with hypogammaglobulinemia or cystic fibrosis.
Asymptomatic infection occurs in approximately 60% of people exposed to Giardia. Asymptomatic cyst carriage can last >6m. No need to isolate asymptomatic carriers once appropriate hygine measures are undertaken. |
|
|
In a child with diarrhea
|
In a child with diarrhea and no clinical signs of dehydration, preferred intake includes fluids low in sugar and the resumption of a normal, age-appropriate diet with minimal sugar and fat. Foods containing excessive sugar can increase the osmolarity of the stool in the intestinal lumen and fatty foods are known to delay gastric emptying, Both can worsen diarrhea
|
|
|
Posterior urethral valves (PUV)
|
Only in males, posterior urethra valves consist of posteriorly situated leaflets within the prostatic urethra, which result in partial bladder outlet obstruction. The increased pressure upstream causes urethra dilation, bladder neck hypertrophy, mucosal trabeculation and vesicoureteral reflux and renal dysgenesis. Hallmarks Of PUV include a distended bladder and a weak urine stream.
Dx: voiding cystourethrogam (VCUG) |
|
|
Infant botulism
|
Supportive care is the mainstay of therapy or infant botulism.
Human-derived botulinum antitoxin should be administered as early as possible Equine-derived botulinum antitoxin to infants is no longer recommended given the self-limiting course of infant botulism. (can cause anaphylaxis and serum sickness) A complete recovery is expected when the diagnosis is made shortly after symptoms first appear and when hospitalization and respiratory support are promptly provided. Most such infants will require hospitalization for 1-3m before they recover enough to be discharged home. Infants that p/w severe disease (e.g. significant cranial nerve palsies) may have a protracted course and some lingering neurologic deficits. Current research suggests that pregnant women are not at risk when household members are vaccinated against disease. The only potential exception to this rule is when a close contact is vaccinated against. |
|
|
Smoking cessation
|
is difficult to accomplish if the smoker remains subject to environmental triggers, including freiends and family who continue to smoke, Parents who want their children to stop smoking should quilt themselves.
|
|
|
Transient synovitis
|
(toxic synovitis) is a common condition that causes pain in the hip, thigh or knee in boys aged 3-10y old. The disorder may be preceded by a respiratory infection, although ESR and WBC are typically normal. If the clinical presentation suggests transient synovitis and plain radiographys are unremarkable, an ultrasound should be performed
|
|
|
Tuberculosis
|
Isoniazid X 9m is the first-line treatment for latent TB in both children and adults. In cases of isoniazid resistance, rifampin becomes the drug of choice and is typically given for 6m in children and 4m in adults.
***All new employees are required to undergo PPD testing prior to the commencement of their work, If PPD is negative, screening should be repeated annually to detect any tuberculin skin test conversions. If it is positive, the workers should be evaluated for the presence of active TB with a detailed history, PE and CXR. Once active TB is ruled out, the pt should be treated with isoniazide for 6-12m. All heathcare workers with latent TB infection should be counseled about the risk of developing active TB and offered preventive therapy with isoniazid for 6-12m. They should not be excluded from the workplace if they refused to accept the recommended therapy. They should continue to have regular follow-up visits for symptom screening and offered treatment or LTBI at very follow-up visit. Sptum AFB smears are not necessary in the absence of cinical or radiographic features of active TB. In contract to active TB, latent TB is not reportable to public health department or CDC. Asymptomatic pt who have received treatment for latent or active TB should not be given isoniazid prophylaxis, even if the repeat tuberculin skin test is positive. |
|
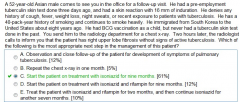
Latent TB
|
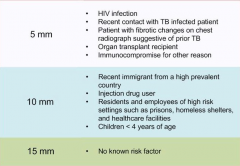
|
|
|
Methylphenidate toxicity
|
Aggressiveness, nervousness, dizziness, agitation,
tachycardia, ↑BP mydriasis,, dry mouth N/V, anorexia, euphoria , Weight and height or age may be ↓with chronic use Management include a toxicologic evaluation, since it may be difficult to distinguish clinically from an emphetamine overdose. It is very important to remember that methylphenidate can not be stopped abruptly because of the high prevalence of psychological dependence to the drug, its dosage must therefore be slowly tapered. |
|
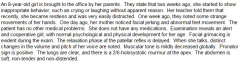
Chlamydia pneumonia in children
|
Absence of fever, staccato不连贯地cough, h/o or concurrent conjunctivitis and ausculatory/radiologic finding out of proportion to the healthy appearance of the child, although transmission takes place at birth, symptoms appear between 2 and 19w. Conjunctivitis is present in half of cases and may present either in the neonatal period or be concurrent with the pulmonary infection.
CXR: hyperinflation, peribronchial thickening and bilateral, symmetrical, intestinal infiltrates. WBC normal but the eosinophil count is elevated. |
|
|
Sydenham’s chorea
|
Usually occur in girls 5-13y
SC is usually preceded by a period of emotional lability, manifested by a tendency to cry or laugh, as well as deterioration of school performance. SC starts with distal hand movements, later progressing to facial jerking and grimacing as well as abnormal feet movement. It usually develops several months after the onset of acute rheumatic fever whereas carditis and arthritis typically develop within 21d. Jerking movements of the face, hands and feet Hypotonic state, (+) pronator sign (when the pt is examined with the arms stretched out, the arms move from the prone手心想上 to the supine position), sudden changes in the pitch and volume of the voice SC should be treated immediately with oral penicillin X 10d or a single dose of im Benzathine penicillin. In pt who are allergic to penicillin, weight based erythromycin, divided in 2-4 doses, should be given. SC usually resolves within 12-15w, however, prophylaxis should be continued into adulthood. If the motor function is severely compromised, valproic acid, Phenobarbital or haloperidol can be started and the pt must be referred to a neurologist. |
|
|
Lead poisoning
|
A blood lead leval > 70 mg/dl (medical emergency) is an indication for immediate hospitalization and parenteral chelation therapy with dimercaprol and EDTA..
A blood lead leval > 44 mg/dl requires chelation therapy (EDTA iv or oral DMSA, DMSA is a derivative of dimercaprol). A blood lead leval > 10 mg/dl requires comprehensive evaluation by CBC, serum electrolyte levels and UA, DMSA or d-penicillamine |
|
|
Candidal diaper rash
|
Tomato-red plaques and satellite papules are characteristic of candidal intertrigo and perineal infection. It is common in infants who have recently received antibiotic therapy. Treat with tropical clotrimazole or nystatin
DD: diaper dermatitis, usually spare the crural脚部的;小腿的folds, treat with zinc oxide and petrolatum ointment. |
|
|
Botulism
|
Gag reflex is frequently impaired in pt with infant botulism. Constipation is typically the first manifestation of the disease and is followed by lethargy, poor sucking and weak crying.
|
|
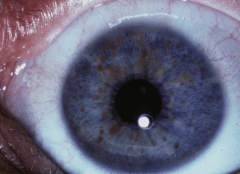
NF1
|
Dx: >=2 of the following
1. a first degree relative with NF1 2. The development of >6 CALS (café-au-lait spots) of >5mm if children or >15mm if adults 3. > 2 neurofibromas, Lisch nodules, optic glioma, bone dysplasia or axillary freckling Genetic testing can be negative in 30% of the cases, it is not needed for the dx. There is 15% possibility of development of optic nerve gliomas. Tx: have a detailed ophthalmologic evaluation for early detection of optic nerve glioma and for search of Lisch nodules (iris hamartoma, pigmented hamartomatous nodular aggregate of dendritic melanocytes affecting the iris) Lisch nodules |
|
|
Enterovirus and Arbovirus infections
|
(a group of viruses that are transmitted by arthropod vectors) are the most common cause of viral meningitis or encephalitis in the pediatric population. Most arbovirus infections are zoonosis (transmitted through animal vectors), for this reason, these infections are more common in the rural areas.
Herpes simplex virus is the most common cause of viral meningitis in the adult population. |
|
|
Cellulitis
|
Cellulitis is characterized by its irregular and elevated borders as well as increased local temperature, tenderness and erythema. Local anesthetics (lidocaine are basic compounds) are not effective for managing cellulites pain because the acidic environment of the infection neutralizes the medication rendering it ineffective.
|
|
|
Neonatal polycythemia
|
is diagnosed when the peripheral venous hct > 65%. High hct levels that are obtained from capillary samples (usually from the heel) are only screening values that need to be confirmed through venous blood sampling. Peripheral venous hct is usually 5-15% lower than hct taken from a capillary sample. The hct reaches its maximum values when the infant is approximately 2h of age, so it is important to recheck hct 12-24h after delivery if the hct is borderline high. The sample must be venous blood.
Neonatal polycythemia can be lift-threatening and can causes apnea, irritability, drowsiness, poor feeding, abdominal distension, hypotonia and hypoglycemia, hyperbilirrubinemia, cardiac and respiratory compromise. These signs and symptoms are due to blood hyperviscosity, which decreases blood flow to different tissues, including the brain and gut. Tx: Adequate hydration and partial exchange transfusion. |
|
|
Cryptorchid testicles
|
usually do not descend spontaneously after 6 months and spermatogonia degeneration begins in the undescended testicles at this age as well. An early surgical referral is recommended at 6m of age.
|
|
|
daily dietary allowance
|
The recommended daily dietary allowance for calcium is 1300mg for children aged 9-18y, 1000mg for adults aged 19-50y and 1200 mg for adults aged > 51y.
|
|
|
Cleft lip
|
Cleft lip +/- cleft palate is typically a multifactorial disorder It is associated with the use of teratogenic agents during pregnancy and the modes of inheritance can be autosomal dominant, autosomal recessive and X-linked.
Reconstruction of the cleft lip is performed 3m of age, according to the rule o “10”: 10 lbs of weight, 10 w of age and 10g of hemoglobin. The recurrence risk in the following pregnancies is close to 50%. Associated cardiac and renal abnormalities are not common. |
|
|
childhood absence epilepsy
|
The prognosis in pt with childhood absence epilepsy, especially if generalized tonic-clonic seizures are absent, is good. Although high doses may be required to control it effectively, the condition is usually responsive to ethosuximide or valproate.
Staring spells will disappear in the teenage years. Unlike CAE, juvenile myoclonic epilepsy (JME) is characterized by a late onset of absence seizures with myoclonic activity and is associated with life-long seizures. |
|
|
Diaphragmatic paralysis
|
of the newborn usually result from a phrenic nerve injury. The two most common causes of phrenic nerve injury are birth injury and cardiothoracic injury. It is typically acoompanied by the signs of brachial plexus injury, such as Erb’s palsy.
The prognosis o obstetrical Erb’s palsy is typically good, with an 80% chance of full or near-full recovery. Erb’s pasly involves the upper roots (C5, C6 and sometimes C7) of the plexus. A serioius complication is diaphragmatic paralysis due to phrenic nerve involvement. |
|

Meconium ileus
|

(Obstruction of the small bowel in the terminal ileus from impacted meconium) is the earliest manifestation of cystic fibrosis (CF) and is almost pathognomonic for the CF. Uncomplicated meconium ileus is characterized by distal intestinal obstruction, wherein the terminal ileum is dilated and filled with thick, tar-like, inspissated meconium.
Plain ABX: dilated, gas-filled loops of small bowel, (-) air-fluid levels and a meconium mass within the right side of the abdomen Meconium ileus. At left, a conventional radiograph of a newborn abdomen shows a "mass" in the right lower quadrant (white arrow) made up of loops of ileum with inspissated meconium, markedly dilated loops of bowel (black arrow) and a "soap-bubbly appearance to the meconium (white oval). In the contrast enema on the right, a small, unused microcolon (white arrows) is seen and there are filling defects representing meconium pellets in the terminal ileum and colon (black arrow). reasonable. |
|
|
Meconium ileus
|
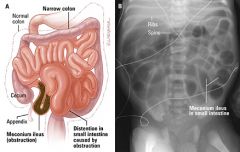
|
|
|
Severe malnutrition
|
Tx: address temperature control (warming), possible infection, dehydration and malnutrition (feeding).
Dehydration should be treated with oral rehydration whenever possible in malnourished pt because they have increased risk of developing heart failure compared to healthy children (iv hydration is used only if there is severe dehydration resulting in shock). Insertion of a Dobhoff tube for rehydration and feeding may be needed in pt with impaired consciousness, vomiting or painul oral ulcers. Placement of the enteric tube beyond the pylorus reduces the risk of aspiration. Feeding should be started cautiously to prevent refeeding syndrome. Systemic infection is commonly present in these pt, blood culture and staring empiric antibiotics is. Early iron supplementation is not recommended because it can lead to GI ulceration. Iron supplementation should begin later in the rehabilitation phase. Feeding solutions should not initially contain excess calories or protein because the pt’s GI reserves have decreased in response to malnutrition. |
|
|
nocturnal enuresis
|
First line management for primary nocturnal enuresis for children < 7y is reassurance the pt’s parents. Alarms are more effective in inducing remission and preventing relapses. The success rate is higher if this method is combined with complex behavioral intervention. Although desmopressin has a fast induction, it is less effective in preventing relapses.
|
|
|
Ticks
|
1. The only complication in most cases is local inflammation/infection although ticks can transmit Lyme disease (1.5%), RMS and ehrlichiosis.
2. brow tick – Lyme disease 3. black tick- RMSF 4. In order to be infected with Lyme disease, the pt must have been exposed to the tick for > 36h, because the transmission of the infection agent – Borrelia burgdorferi --- takes place only after the tick is firmly attached to the skin and has suctioned a certain amount of blood which gives it an engorged appearance. |
|
|
Lyme arthritis
|
Dx: can not be confirmed with serology tests. Serology identiies those with the disease and those with a previous exposure, therefore a positive results is non-discriminatory. Moreover, serology can be negative in pt who were partially treated or in those who received antibiotics for another reason.
Synovial fluid analysis with measurement of antibody titers through ELISA or Western blotting is needed to confirm the dx. Most pt (approximately 90%) are disease-free one year after the start of therapy. If the clinical suspicion of Lyme arthritis is high, antibiotic therapy may be started even when results are pending because synovial fluid serology usually takes time. Majority o pt will respond immediately. Recurrence of the disease is possible, but this is not the norm. Tx: 30d course of amoxicillin or parenteral ceftriaxone. Doxycycline and ceftriaxone are the drug of choice for adults. Those allergic to penicillin can be managed with erythromycin. Oral therapy is preferred unless there is a suspicion of neurologic compromise. The prognosis is good. If arthritis recurs despite antibiotics, parenteral therapy is indicated. Those who are not treated can have recurrent episodes of arthritis even 8y after the onset of disease. |
|
|
Lyme disease - pregnancy
|
There is little to no risk to the etus if the mother contracts Lyme disease during pregnancy if it is appropriately treated. Lyme disease can only be spread by a tick vector, There is no possibility for spread between humans.
|
|
|
GBS colonization
|
Chemoprophylaxis with penicillin G/ampicillin > 4h before delivery is considered adequate. Infants born to mothers with GBS colonization but inadequate treatment need to be examined for signs of sepsis, and CBC with differential and blood culture need to be drawn, Even if there is no sign of sepsis, those infants should be observed for > 48h prior to discharge from the hospital.
Broad spectrum antibiotics (ampicillin and gentamicin) are only indicated if the infant has GBS bateremia or confirmed GBS infection. LP is necessary if the mother has chorioamnionitis or if the infant develops signs of sepsis (temperature instability, irritability, lethargy. Apnea and bradycardia).Infants with meningitis often will appear septic instead of having typical meningeal signs (photophobia, neck stilfness) |
|
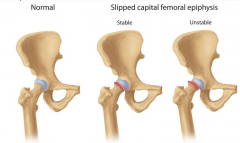
Slipped capital femoral epiphysis (SCFE)
|
Common in African American children, boys, 10-16y/o, related with obesity
For children < 10y, it is associated with metabolic endocrine disorders (hypothyroidism, panhypopituitarism, hypognadism, renal osteodystrophy, growth hormone abnormalities) 20% bilateral involvement It is called stable if the pt can bear weight and unstable if the pt can not ambulate, unstable SCFE is associated with more complications, including avascular necrosis of the femoral head (AVN). The underlying cause is a widened epiphyseal growth plate, due to abnormal cartilage maturation and endochondral ossification. Tx: surgical , immediate internal fixation with a single screw. Delay in treatment >24h leads to increased AVN, SCFE progression from stable to unstable, and high risk of future degenerative arthritis. Prophylactic contralateral fixation of the unaffected hip is not routinely done in the US except in pt with endocrine abnormalities. |
|
|
acute pharyngitis
|
The benefits of antibiotic therapy in child with acute pharyngitis: prevention of rheumatic fever, but NOT decrease the risk of acute glomerulonephritis because cutaneous infection is typically implicated in acute glomerulonephritis.
Impertigo ---- acute glomerulonephritis Pharyngitis ---- rhrumatic fever and acute glomerulonephritis |
|
|
of cat-scratch disease
|
The most common complication of cat-scratch disease is suppuration of the lymph nodes.
The incidence of infection complicating a cat bite is close to 50%, antibiotic prophylaxis covering a broad spectrum of cat mouth flora, including Pasteurella multocida is recommended, especially in high-risk situations (a hand bite) wherein the potential infection could extendto the bone and joint. The first dose of ampicillin/sulbactam is usually given parenterally, an oral ampicillin/sulbactam is administered subsequently for 3-5d. |
|
|
Varicella vaccination
|
It is advisable for all pt to receive pre-transplantation varicella immunization.
Varicella vaccination of household contacts of transplant recipients is relatively safe and is currently recommended by the American association of pediatrics. Transmission of vaccine-associated VZV is not typical, except for some cases when post-vaccination rash appears, therefore, this child should be monitored or the appearance of a rash and isolated if a rash appears. |
|
|
Contraindications for DTaP vaccinations
|
1) anaphylaxis within 7 days of administration of a previous DTP or DTaP vaccine, and
2) Encephalopathy within 7 days of administration of a prevoious DTP or DTaP vaccine. If high ever ( >104.8F), shock, inconsolable crying for 3-4h or seizure occur within 24h of receiving a dose of DTaP vaccine, then subsequent doses should be given with caution. Temporary contraindications: moderate or severe illness There are no significant contraindications to receipt of vaccinations against Hib, poliovirus and pneumococcus. |
|
|
Contraindication for MMR vaccination
|
1. Current moderate/severe febrile illness
2. Anaphylaxis to neomycin or gelatin 3. Severe immunodeficiency (CD4<200/mm3) 4. Thrombocytopenia after the first dose of MMR 5. Recent administration of immunoglobulins – diminish the efficacy of MMR 6. Pregnancy The following are NOT contraindications for MMR 1. TB or +PPD 2. Breastfeeding 3. Immunodeficient family member or household contact 4. Asymptomatic HIV-infected pt without severe immunosuppresion 5. Anaphylaxis to eggs |
|
|
Dx for febrile seizures
|
1. Age < 6y
2. No past h/o afebrile seizures 3. T> 38 4. No evidence of CNS infection 5. No metabolic disturbances present which may produces seizures Febrile seizures may be subdivided into 2 forms: simple and complex. Simple febrile seizures Generalized, brief (<15min, for seizures occurring in series, a cumulative duration < 30min) and occur in children aged 6m-5y. It is associated with T> 38C in children that are otherwise neurologically normal and display no evidence of meningitis or encephaliti. Febrile seizures often occur on the first day of a mild illness as the child’s temperature is rising and may be the first manifestation of illness. Generally studies are not necessary for the evaluation of the simple febrile seizure. The parents o this child should be reassured that simple febrile seizures are a common occurrence and that while they should continue to monitor their child for any new developments, there is no cause for alarm at this time. There is slightly increased risk of epilepsy (prognosis) and significantly elevated risk of recurrence compared to the general population. Complex febrile seizures, on the other hand, are characterized by focal features (postictal paresis), > 15min and if occurring in series, a cumulative duration of > 30min. Children with pre-existing neurologic conditions (arteriovenous malformation) or bleeding disorder should always undergo CT scan of the head without contrast after mild head trauma. Some clinicians recommend ordering a head CT without contrast in all children who report a brief loss of consciousness after head injury. |
|
|
Precocious puberty
|
: premature activation of the hypothalamus-pituitary-gonad axis
Can result from hypothalamic dysfunction: testicular enlargement, penis enlargement, pubic hair growth and a growth spurt Can result from severe hypothyroidism, slow growth |
|
|
Precocious pseudo-puberty
|
: gonadotropin-independent process, typically an excess of sex steroids, p/w signs of severe androgen excess (severe cystic acne, significant growth acceleration, enlarged penis), small testicles, can be casued by late-onset congenital adrenal hyperplasia, 21-hydroxygenase deficiency
|
|
|
Gynecomastia
|
Gynecomastia is very common (up to 70%) in pubertal males. Its occurrence during puberty is associated with the relative excess production of estrogen from the testes. In majority of subjects, gynecomastia regresses in about 18-24m, however this may persist in some pt and although rare, it could be cosmetically disfiguring.
Tx: reassurance and follow-up in 6m |
|

Benign premature thelarche
|
18-24 months
Bilateral breast enlargement not accompanied by other signs of isosexual precocious puberty (rapid increase in height, increase in bone maturity, appearance of axillary and public hair and menstrual bleeding) Tx: expectant, majority of the pt remain stable or have reversal of the breast enlargement in a few months. Stages of pubic hair development in boys. Stage 1: Prepubertal, with no pubic hair. Stage 2: Sparse, straight pubic hair along the base of the penis. Stage 3: Hair is darker, coarser, and curlier, extending over the mid-pubis. Stage 4: Hair is adult-like in appearance, but does not extend to thighs. Stage 5: Hair is adult in appearance, extending from thigh to thigh |
|
|
Complete airway obstruction
|
unable to cough or pass any air through the airway, although they may make gagging or choking noises --- respiratory failure rapidly
Helmlich maneuver: Give a series of 5 abdominal thrusts with the child standing or sitting, do it while the pt is lying down if the child is unconscious. |
|
|
Partial airway obstruction
|
the ability to talk, cough or breath.
The Heimlich maneuver is recommended in children with complete airway obstruction, who are > 1y. Below this age, give blows on the back with the heel of the hand alternating with chest thrusts. |
|
|
severe iron deficiency anemia
|
Children suffering from severe iron deficiency anemia should respond to iron supplementation with an increased reticulocyte count within 72h.
|
|
Rabies
|
The rabies usually starts with non-specific prodromal symptoms, including fever and pharyngitis. Neurological symptoms (conusion, lethargy, paralysis and aphasia) develop later in the course of the disease.
Unlike developing countries, domestic animals are not the common sources of infection in the US. Wild animals such as skunks臭鼬, foxes and bats are typically implicated as the vectors of the infection. The acquistition of rabies from bats does NOT require a traumatic event such as a bite or a scratch, but may involve aerolization of the viral particles and infection by respiratory exposure. Bat can transmit rabies even though there is no evidence of a bite. For this reason, if a bat is found in the room of a person and details of the exposure are unknown (person is small child or is sleeping, intoxicated, demented or with serious psychiatric problems), the CDC recommends postexposure prophylaxis Rabies is an almost universally fatal disease once pt are symptomatic. Tx: one dose anti-rabies immunoglobulin and 5 doses of the vaccine immediately unless the animal has been captured for observation (if it is a cat, a dog or a ferret) or for sacrifice and autopsy (if it is a wild animal such as a bat). Effectiveness will be the same if treatment is postponed for < 5 days although there have been reports of rabies in persons not vaccinated in the first 72h when the bite was in the head or the neck. |
|
|
Rabies prophylaxis
|
Previously vaccinated persons who are potentially re-exposed to rabies should receive only active immunization with a rabies vaccine.
Previously unvaccinated individuals who are exposed to a potential source of rabies should receive both active and passive immunization |
|
|
Anorexia nervosa
|
Indication for admission:
1. physiologic instability 2. Electrolyte abnormalities (hypokalemia, hyponatremia) 3. Severe malnutrition (< 75% of ideal weight) 4. Acute medical/psychiatric emergencies (pancreatitis, seizures, syncope, suicidal ideation, psychosis) 5. bradycardia (HR < 50/min), hypotenstion (BP < 80/50), hypothermia (T< 96F), orthostatism 6. Acute food refusal 7. Failure of outpatient therapy |
|
|
Refeeding syndrome
|
: 2-3w after refeeding is started in pt with anorexia nervosa. It is due to severe hypophosphatemia which can lead to tissue hypoxia and depletion of energy stores. The pt develops heart failure and edema
|
|
|
Voiding cystourethrogram
|
is recommended in the following pt to demonstrate vesico-ureteral reflux.
1. Children < 5y with a febrile UTI 2. Males of any age with a first UTI 3. Females < 3y with a first UTI 4. Children with UTI who do not promptly respond to antibiotic therapy 5. Children with recurrent UTI |
|
|
HPV vaccine
|
There are currently 2 HPV vaccines available: a bivalent HPV vaccine (HPV2) and a quadrivalent HPV (HPV4). The HPV2 is directed against HPV strains 16 and 18, which causes 70% of cervical cancer, while the HPV4 is directed against HPV strain 6 and 11, which cause 90% of genital warts, in addition to HPV strains 16 and 18.
Both HPV vaccination series should be started at 11-12 years of age and completed prior to the child becoming sexually active. They are administered in 3 doses, given at time point 0, then at 1-2m and finally at 6m. The vaccination series can be started as early as age 9 and as late as age 26. An interruption in the vaccination schedule does not require the entire series to be restarted. Even if the type of shot given initially (bivalent or quadrivalent) is not known, there is no need to repeat the entire seires, the remaining two shots of the HPV vaccine can be either one (the 3 shots in the series do not necessarily need to be of the same type). The HPV vaccines are not live vaccines and can be co-administered with other vaccines, live or inactivated. The HPV vaccines can also be given to those who are immunosuppressed. Women with abnormal pap smear or genital warts should still receive the HPV vaccine. It can still offer protection against future infections caused by other HPV strains. Not be given to pregnant women but can be given to lactating women. No pregnancy test is needed before administering the vaccine and no intervention is needed if the vaccine is accidentally administered to a pregnant woman. |
|
|
Gastroesophageal reflux (GER)
|
It is a clinical dx. Reassurance should be offered to the mother that the “spitting up” is a normal occurrence in infants up to 24m old.
No intervention if the child is otherwise healthy and developing appropriately (the happy spitter). In children with mild GER, the mainstay of conservative treatment is thickening of fomula with cereal, which usually results in decreased emesis, cry and better weight gain. If it fails, try H2 receptor antagonist like ranitidine. |
|
|
Neonatal sepsis
|
Group B strep, Klebsiella, Enterobacter, E. coli
Tx: cefotaxime/ceftriaxone + ampicillin (ceftriaxone ---- acute bilirubin encephalopathy) The type of bilirubinemia involved also affects the approach in management of septic infants. Indirect hyperbiliruinemia is usually physiologic in nature and persists while direct hyperbilirubinemia is probably induced by sepsis-related cholestasis. Ceftriaxone can not be used in this case since it may displace albumin-bound bilirubin and aggravate cholestasis (sulamethoxazole can worsen indirect hyperbilirubinemia by increasing the amount of free bilirubin, which may increase the risk of kernicterus). |
|
|
Flexible kyphosis
|
A common finding in adolescents.
On lateral X-ray, the angle of thoracic kyphosis is normal or slightly increased (20-40 degrees.) Flexible kyphosis驼背 is easily correctable by voluntary efforts and on prone-extension test. There is no evidence that flexible kyphosis leads to adverse physician effects. There is no evidence that flexible kyphosis leads to adverse physical effects or permanent deformity |
|
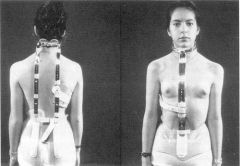
Scheuermann disease
|
Not corrected with voluntary efforts, a sharp angulation is commonly seen on forward bending.
Tx: Milwaukee brace (< 70-80 degrees angulation) and exercises to strengthen spinal muscles Surgical correction (significant angulation, intractable pain, neurological abnormalities) Milwaukee brace |
|
|
Otitis media
|
The most common pathogens responsible for acute otitis media include Streptococcus pneumoniae (35%), Haemophilus influenza (25%) and Moraxella catarrhalis (15%). Over 90% of infections with H. influenzae are caused by the nontypable strains. Most early recurrences of acute otitis media are not true relapses but rather are caused by a different “top three” pathogen or different strains of the same pathogen.
Fluid may persist in the middle ear for up to 3m after antimicrobial treatment of an acute episode of otitis media. Therapy is not usually required unless there are persistent symptoms of infection, the effusion is bilateral, or > 3m have elapsed since the acute episode. |
|
|
Tuberculous meningitis
|
All infants and children with tuberculous meningitis, military TB and tuberculous osteomyelitis should receive >12m of antituberculous therapy. In a pt with drug-resistant infection, therapy > 18-24m, depending on the clinical response and severity of the illness.
Isoniazid + rifampin + pyrazinamide X 2m, then INH + rifampin Intrathecal therapy is not recommended since all the agents (Isoniazid + rifampin + pyrazinamide) have good CSF penetration. Pt with pulmonary TB can be considered non-infectious if she has had 3 negative sputum acid-fast smears on 3 different occasions. |
|
|
Keratitis
|
Foreign body sensation, photophobia, corneal opacity/ulceration
Urgent ophthalmologic referral Can occur with conjunctivitis The presence of purulent eye discharge (viral/allergic conjunctivitis: simple morning crusting followed by watery discharge) generally warrants antibiotic treatment for bacterial conjunctivitis: erythromycin ointment, sulfa drops and polymyxin/trimethoprim drops. Fluroquinolones should be reserved for contact wearers because of their increased activity against Pseudomonas, which is a common pathogen in these pts. Bacterial conjunctivitis is very contagious. A minimum of 24h of antibiotic therapy is generally required by most institutions before the individual returns to work or school. |
|
|
RSV bronchiolitis.
|
A secondary bacterial infection of the middle ear and future risk of bronchial hyperreactivity (asthma) are the most common complications of RSV bronchiolitis.
|
|
|
Myelomeningocele
|
Bladder dysfunction is a universal complication of lumbosacral myelomeningocele (excluding neurological deficits), followed by lower GI tract dysfunction and fractures of the lower extremities.
|
|
|
Gender separatism
|
Discomfort at being seen naked by a member of the opposite sex is common in children starting by the age of 4 and tends to taper off gradually during adolescence, peak at 9
|
|
|
Sickle cell disease
|
In children, the most common initial symptoms of sickle cell disease is dactylitis, which develops in 40% of pt.. Splenic sequestration is the second most common and occurs in 20% o pt. Other complications such as ischemic events are not as frequent and are seen mainly in the adult population.
|
|
|
Turner syndrome
|
No increase recurrence risk is present after having an infant with Turner syndrome. The risk of 45, X does NOT increase with increased maternal age.
* Pregnancy is almost impossible, but there still remains a very small chance, in pt with Turner syndrome. |
|
|
infantile hypertrophic pyloric stenosis
|
The usage of erythromycin (postexposure prophylaxis for pertussis) is associated with the development of infantile hypertrophic pyloric stenosis.
|
|
|
Constipation in children
|
Tx: 1. dietary modification
2. mild laxatives such as magnesium hydroxide 3. Enemas and suppositories are reserved for severe constipation/fecal impaction |
|
|
an intussusception
|
The complication of greatest concern when reducing an intussusception with a hydrostatic or air contrast study is perforation of the bowel, which occurs in <1% of pt.
|
|
|
Evaluation of language delay or mental retardation
|
1. H&P (microcephaly, dysmorphic features, high-risk behavior for lead poisoning, family history of neurolingual abnormalities)
2. Sensory screening: complete ophthalmologic examination and audiometry, preferably using brainstem auditory evoked response |
|
|
Antenatal corticosteroid therapy
|
(decrease the risk of infant respiratory distress syndrome and intraventricular hemorrhage)
Betamethasone or dexamethasone im provideds stable and predictable concentration of the drug in the blood that is required to achieve the desired fetal effects. |
|
|
Postpartum endometritis
|
Fever, uterine tenderness, foul-smelling vaginal discharge, leukocytosis, caused by a polymicrobial infection of the deciduas (the pregnancy endometrium)
The most important risk factor in the development of endometritis is the route of delivery. Endometritis occurs after 3% of vaginal births but after 15-30% of cesarean deliveries. Gold standard of treatment: Clindamycin and gentamicin (metronidazole is contraindicated in breastfeeding mothers) |
|
|
Condyloma acuminate
|
is a manifestation of infection with HPV (subtype 6, 11) and is not considered a contraindication to the vaginal delivery in the pregnant women since HPV is thought to be contracted by the infant in < 1% of all childbirths to women who have condylomas.
Condyloma acuminate is STD. Flesh-colored, hyperkeratotic papules on posterior introitus, labia major and labia minora. The papules have a smooth surface and are sessile. Pruritus, bleeding, burning, tenderness, vaginal discharge and pain, depending on the location. Large lesions can interfere with defecation, vaginal intercourse and delivery. Visula inspection with application of acetic acid (lesions should turn white) is usually sufficient for making the correct diagnosis. Tx: Chemical destruction is preferred as the initial approach by many physicians Trichloroacetic acid application destroys the lesion by protein coagulation, the clearance rate is not very high, therefore repeated applications are usually necessary. Podophyllin has a similar effect as trichloroacetic acid but is not indicated for internal use with condylomata acuminata (should not be applied to the mucosal surface). Podophyllin is contraindicated during pregnancy. |
|
|
OCPs-pregnancy
|
All women who wish to get pregnant should take 400 ug folic acid daily >1m before the projected date of conception, OCPs can be stopped at any time, however conception may be delayed because the pt may continue to have anovulatory cycles immediately after discontinuation.
OCPs have 99.9% efficacy whn taken by the perfect users who never misses taking a pill, takes the pill at the sam time each day, and never vomits or has diarrhea. 1 pregancy for every 1000 women, 95% efficacy for every 1000 women. Fortunately, the risk of fetal anomalies secondary to accidental use of OCPs during pregnancy is negligible. |
|
|
Maternal hyperglycemi
|
Maternal hyperglycemia may result in excessive glycogen deposition in the fetal myocardium. This causes fetal hypertrophic cardiomyopathy and possible CHF.
Tx: observation and conservative medical therapy , the defect will often correct spontaneously in the infant following birth as it will no longer be exposed to the maternal hyperglycemia and the excessive glycogen within the myocardium will be depleted by normal metabolic processes during fasting periods. |
|
|
Gestational DM
|
A 50g oral glucose challenge (fasting is NOT required) with blood glucose values of >130-140 mg/dl is generally followed by a 100g oral glucose tolerance test with hourly blood glucose measurement for 3h on a fasting state.
HBA1C can be used to diagnose overt diabetes in pregnancy but a normal HBA1C does NOT eliminate the need for further screening in pregnant pt. The recommended fasting blood glucose values in pregnant diabetic pt should be < 95mg/dl and 2h postprandial blood glucose should be < 120mg/dl. Insulin is the treatment of choice for gestational DM that is nonresponsive to dietary restriction, with intermediate acting NPH insulin the most commonly used agent in combination with regular or lispro insulin. The use of long-acting glargine insulin is generally avoided due to its teratogenic effects. Regular (rapid onset of action, short duration of action) NPH (slower onset of action, longer duration of action. |
|
|
Retroverted uterus
|
A Retroverted uterus is a common condition found in 11% of the female population. If it is secondary to chronic PID or endometriosis, it can be associated with infertility. It is also related to dyspareunia, low back pain and dysmenorrheal,
Repositioning of the Retroverted uterus into an anterior position between 12w and 16w of pregnancy. Repositioning does not happen in 1.4% of the pt -----uterine incarceration in the sacral region, need manul reposition by physician. Surgery is recommended only for pt with dyspareunia related to a retroverted uterus |
|
女Has breast but no pubic/axiillary hair or uterus = androgen insensitivity
|
female phenotype, amenorrhea, testes (testes should be removed before age 20 because of increased risk of testicular cancer)
女Has breast with public/axillary hair, no uterus/fallopian tubes/cervix/upper vagina, normal ovary |
|
|
Infants born to mothers with a positive HBsAg
|
should be given hepatitis B vaccine and hepatitis B immune globulin within 12h of delievery. There is no indication that cesarean section reduces the rate of maternal-infant transmission of HBV.
|
|
|
Pap smear
|
A Pap smear sample is considered unsatisfactory if it is unlabelled, contains < 5000 well-visuaized squamous cells or has obscuring inflammation or blood. A Pap smear containing metaplastic and endocervical cells (EC) is considered to be a good sample of the trannformation zone of the cervix—junction of squamous and glandular cells at the external cervical os that is at greatest risk for neoplasia. The EC/TZ component is more likely to be absent in adolescents and women >30 years, particularly postmenopausal women. Pap smear can still be considered satisfactory without the EC/TZ component.
Current recommendations suggest repeat Pap smear in 12m for women who have a satisfactory Pap smear and negative cytology result without the EC/TZ component. Cervical cancer screening should be started at the age of 21, regardless of age of onset of sexual activity (and then every 2 years until the age of 30, the interval can be 2-3 years after 3 consecutive negative pap smear). This is because high-grade cervical cytological abnormalities due to HPV usually do not occur until 3-5 years after HPV exposure, also cervical cancer is rare in women < 21y.Routine testing or HPV is not indicated for women under the age of 30. |
|
|
Severe PID
|
Obtain high blood concentration of the antibiotics as soon as possible. All therapy should be intravenous.
Abdo pain and tenderness on palpation of the adnexae and lateralization of the cervix, fever, chills, bandemia, leukocytosis, N+V Cefoxitin+doxycycline Ceftriaxone + doxycycline If a tubo-ovarian abscess is diagnosed, surgical evaluation is immediately needed. |
|
|
Myelomeningocele
|
Pt with spina bifida must be referred immediately to the neurosurgeon. Majority of pt with myelomeningocele also have hydrocephalus and Chiari II malformations. An urgent neurosurgical evaluation is needed because the lesion must be closed in the first 24-48h after birth to prevent infections in the CNS.
|
|
|
Preeclampsia
|
1. hydralazine or labetalol to lower BP (2 drugs for acute management o HTN during pregnancy, methyldopa is the preferred for oral therapy in mild to moderate HTN)
2. MgSO4 to prevent progression to eclampsia (best medication to prevent further seizure, diazepam or phenytoin can be added to the therapy if seizures persist although the use o diazepam should be limited due to its depressant effects on the fetus, phenobarbital is reserved only or those cases in which seizure persist, despite the use of magnesium sulfate, diazepam or phenytoin) 3. Induce labor if >=36w 4. For mild preeclampsia (>140/90, proteinuria 1-2+ or > 0.3g), vaginal delivery is the preferred mode of delievery For severe preeclampsia (>160/110, proteinuria 3-4+ or >5g, headache, epigastric pain, change in vision), the preferred mode of delivery has not been evaluated. Hyperreflexia is an ominous sign in preeclampsia pt and usually heralds eclampsia, Retinal hemorrhage is an extremely ominous sign of preeclampsia. A h/o preeclampsia in the past increases the risk of developing this complication during a subsequent pregnancy, This risk is higher if the preeclampsia presented earlier (age of delivery was < 32-33w) or if the pt has renal disease or chronic HTN. |
|
|
Gestatopma thrombocytopenia
|
A benign condition defined by the presence of 5 distinct criteria
Mild and asymptomatic thrombocytopenia Late in pregnancy No h/o thrombocytopenia outside of pregnancy No evidence of fetal thrombocytopenia Spontaneous resolution once the child is delivered Tx: conservative, follow up DD: HELLP syndrome, HIV, ITP (usually plat <50 000/ul , develop earlier in the pregnancy), TTP |
|
|
Bacterial vaginosis (BV)
|
Current studies suggest that adverse outcomes such as preterm labor are not improved when BV is screened for or treated in average-risk asymptomatic women.
A short course of antibiotic therapy will alter the microlora imbalance, but recurrences are common. Screening for BV may be indicated if the pt is at high risk for preterm labor, and treatment with oral metronidazole or clindamycin is appropriate if a pt is either at high risk or preterm labor or is symptomatic. |
|
|
Chlamydia trachomatis in pregnancy
|
Genitourinary infection by Chlamydia trachomatis is sexually transmitted. Pregnant women <25y and those at increased risk for Chlamydia should have repeat testing in the third trimester.
Reactivation of Chlamydia does NOT occur. A positive culture in a pt who has previously negative implies recent sexual transmission. It is STD and can not spread directly from a water souce. Chlamydia endometritis during pregnancy can lead to chorioamnioitis and premature delivery of the fetus., conjunctivitis and pneumonia. Tx: erythromycin for pt and sexual partner |
|
|
Rectocele
|
Women with symptomatic rectoceles who are poor surgical candidates may be treated with pessaries in conjunction with estrogen cream. Without it, these can cause chronic discharge and bleeding secondary to injury of the vaginal tissues.
|
|
|
Polycystic ovarian syndrome
|
Weigh reduction should be tried first in the attempt to restore fertility. If weight reduction fails, clomiphene citrate can be tired. Even a moderate reduction in weight may restore fertility.
|
|
|
Epilepsy and pregnancy
|
Although anti-epileptic drug use during pregnancy is associated with an increased risk of congenital abnormalities, over 90% of women with epilepsy have normal pregnancy. There is no agreement about which anti-epileptic drug is most or least teratogenic, therefore the drug that works best or the pt should be used. Switching to another drug is NOT usually recommended for pt taking anit-epileptic drugs during pregnancy.
There is no direct evidence that supplementing folic acid may decrease the risk of neural tube defects in pt taking anti-epileptic drugs. High dose folic acid 4mg/day is recommended prior to conception (1-3m) and during the first trimester of pregnancy. Once the organogenesis period is over, the role of folic acid prevention is very limited. Early detection of neural tube defects by serum AFP screening, amniocentesis or U/S is important. If major abnormalities are present, the pregnancy can be terminated. Taking anti-epileptic medications is not a contraindication to breastfeeding. |
|
|
Hyperthyroidism in pregnancy
|
Due to an incrase in serum concentrations of thyroxine-binding globulin (TBG), pregnant women have high levels of T3 and T4. In order to determine if a pt has true hyperthyroidism, free T4, total T4 and TSH levels need to be determined.
Dx: 1. high serum free T4 2. serum TSH < 0.01mU/L DD: gestational transient thyrotoxicosis (mild increased free T4, slightly decreased TSH at the first trimester, GTT occurs in 10% of women, 8-11 weeks of gestation , does not occur after 14w, it is due to the elevated levels of hCG, which has thyroid-stimulating properties) * As soon as pregnancy is confirmed in hypothyroid pt who are receiving hormone replacement therapy, the dose of L-thyroxine should be increased due to increases in thyroxine-binding globulin (TBG) and th volume of distribution of T4 and an increase in body mass. * The estrogen can increase TBG level, which may result in an increase in the total T4 levels and decrease in free T4 levels, therefore, TSH levels should be checked 12w after pt with primary hypothyroidism are started on OCPs, and the dosage o levothyroxine should be increased. |
|
|
TB-pregancy
|
Pregnant women stricken with TB not likely to be drug-resistant should be treated with isoniazid (INH), rifampin and ethambutol for a period of 9m.
Pregnant women stricken with multi-drug resistant TB should be treated with isoniazid (INH), rifampin, pyrazinamide and ethambutol for a period of 9m. Since there is a pancity of data regarding the teratogenicity of pyrazinamide, it should not be used in pregnant women unless there is strong evidence that MDR-TB is present is present (previous treatment for TB or exposure to a known case of MDR-TB) |
|
|
HIV --- pregnancy
|
An HIV+ woman who is already receiving HAART should be counseled to continue her treatment regimen if her pregnancy is identified after her first trimester. (Zidovudine in particular is considered an essential component of the treatment regimen as it has been demonstrated to significantly decrease the vertical transmission of HIV).
For those HIV+ women whose pregnancies are identified early on in the first trimester, an acceptable alternative is to discontinue HAART or the remainder of the first trimester and then resume it thereafter. The preferred mode of delivery in an HIV+ women is elective cesarean section. HIV+ women should feed their infants with formula instead of breast milk, regardless of therapy given to the mother or infant. |
|
|
Pelvic cystic mass in pregnancy
|
A pregnant woman with a pelvic cystic mass needs to be observed carefully. If the mass is >5cm in size and persist beyond the first trimester or shows no regression in subsequent visits, surgical intervention is indicated due to high risk of rupture, hemorrhage and torsion, all of which may lead to preterm delivery. Removal of the cyst should be delayed until the 2nd trimester to decrease the chance of fetal complications.
|
|
|
UTI in pregnancy
|
Cephalexin, amoxicillin or nitrofurantoin X 3-7d, Trimthoprim-sulfamthoxazole is not advised in the first or third trimester of pregnancy. The use of sulfonamids near term can cause displacement of bilirubin in fetal circulation ---- increase the risk of hyprbilirubinemia and kernictrus. TMP-SMX affects folic acid metabolism during pregnancy.
Nitrourantoin is pregnancy risk category B, though it is contraindicatd at term, during labor and delivery or when the onset of labor is imminent. There is very little bacterial resistance to nitrofurantoin even though it has been used for the last 50 years, though it does have a lower cur rate and more side effects than TMP-SMX and fluoroquinolones in general. |
|
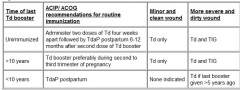
UTI in elderly
|
Asymptomatic bacteruria is common in elderly pt and does not require oral antibiotics therapy if the urine WBC count is < 20 WBC/HPF. Most of these pt’s bacteruria will resolve without treatment over a period of time. Very few pt may develop urosepsis, hence, pt should be advised to report any symptoms o UTI such as fever, dysuria, frequency or suprapubic pain. Repeat urine culture should be performed in 2m.
|
|
|
Syphilis in pregnancy
|
Penicillin
If penicillin allergic, penicillin desensitization is recommended (incrmntal does of oral penicillin V) |
|

Subchorionic hematoma
|
U/S is the best means of discerning bleeding between the endometrium and gestational sac in the pregnant woman, that is subchorionic hematoma. It appears on sonography as crescent-shaped hypoechoic regions adjacent to the gestational sac and are the most commonly identified source of first-trimster bleeding. Women with this condition are managd expectantly until the symptoms resolve or additional finding develop. Once a subchorionic hematoma has been diagnosed, it should be re-evaluated with a repeat U/S one week later. Unfortunately, there are no known therapeutic interventions for the condition. Pregnant womn who have subchorionic hematomas are at increased risk for experiencing spontaneous abortion. There appears to be a correlation between this risk and larger hematoma size, increased maternal age, and earlier gestational age.
The only management option for subchorionic hematoma is expectant management. Some clinicians repeat an ultrasound in two weeks to confirm fetal viability and assess for change in size of the hematoma. This is often reassuring to the patient, but does not alter management. A subchorionic hematoma is not an indication for an evaluation for an inherited thrombophilia |
|
|
Pyelonephritis in pregnancy
|
Hospitalization, iv ceftriaxone/ampicillin, gentamicin until pt is afebrile for 24-48h and experiencing an improvement in symptoms. Pt should then be discharged on oral antibiotics, with the entire treatment course lasting for 10-14d.
If the symptoms do not respond to antibiotic therapy within 48h, then a renal U/S to assess for perinephric abscess or renal calculi should be performed. |
|
|
Exercise in pregnancy
|
Mothers should attempt 30min of exercise onmost days at an intensity that does not exceed a 12-14 on a 20 pont scale. A more useful measure of appropriate intensity is to inform the mother that she should be able to carry on a conversation throughout her exercise routine. If she can not, then the intensity of her exercise is too great.
While water-immersion exercise is regarded as an excellent choice for pregnant women, scub dirving is specially prohibited in pregnancy due to the risk of decompression injury and gas emboli in the fetus. Walking or cycling is a good choice. Swimming is an ideal activity during pregnancy. Distance running, skiing should be avoided as well. |
|
|
Premature ovarian failure-- Hormone replacement therapy
|
Older postmenopausal women on hormone replacement therapy are at an increased risk for MI, DVT, strokes and breast cancer. The findings of this study do not apply to younger pt with premature ovarian failure. Hormone replacement therapy in the form of conjugated equine estrogen and medrooxyprogesterone with careful monitoring can be safely used in younger pt without any excessive cardiovascular risk.
Estrogen is the “gold standard” treatment for hypoestrogenic symptoms, improve bone mineral density and hot flashes. |
|
|
Post partum hemorrhage (PPH)
|
The most common cause of PPH is uterine atony and the first step with PPH is to do a pelvic examination to identify any retained placental fragments.
If the retained plancental products are not identified, manual uterine massage should be started. Uterine massage stimulate the uterus to contract. If bimanual uterine massage fails to control bleeding, uterotonic drugs like iv oxytocin are used to control bleeding. If bleeding does not stop with medical measures, surgical measures are taken. Uterine artery ligation is one of the surgical measures for the treatment of PPH. |
|
Premenstrual syndrome (PMS)
|
Behavioral and physical symptoms that occur in the second half of the menstrual cycle.
Premenstural dysphoric disorder (PMDD) is a severe form of PMS characterized by the prominence of anger and irritability. SSRI are first-line therapy for PMDD 15% of pt are resistant to fluxetine, in such cases, alprazolam is a good alternative and is given in the luteal phase of the menstrual cycle. |
|
|
Shoulder dyctocia
|
The mother should be told not to push while attempts are made to reposition the fetus. Suprapubic pressure directed downward and laterally should then be applied by an assistant. If suprapubic pressure fails to deliver the anterior shoulder, then typically the Mc Roberts maneuver is attempted, though many other techniques work as well (Rubin maneuver, Woods screw maneuver, delivery of posterior arm).
|
|
|
Prolonged active phase < 1.2cm/h
|
Hypotonic uterine contractions is the most common cause of arrest disorders in the active phase of labor. Pt with such conditions should undergo an augmentation of labor using amniotomy and/or oxytocin infusion
|
|
|
Perimenopause
|
Perimenopause is the time extending from 2y to 8y preceding menopause until one year following the last menstrual period. This state is associated ith normal ovulatory cycles interspersed with anovulatory cycles that vary in length, menses become irregular and heavy breakthrough bleeding may be reported.
Endometrial hyperplasia can develop during lengthy intervals of anovulation. If a pt complains of an episode of heavy dysfunction bleeding or of >6m of irregular menses, then endometrial surveillance in the form of vaginal U/S (to ensure the endometrial thickness is < 4mm) or endometrial biopsy is indicated. |
|
|
Cervical incompetence
|
Surgical treatment of cervical intraepithelial neoplasia before conception increases the incidence of cervical incompetence and preterm birth 200-300%.
p/w painless cervical dilation.after the first trimester with expulsion of a previable living fetus. Women with cervical insufficiency may be asymptomatic or may present with mild symptoms such as pelvic pressure, premenstrual-like cramping or backache, and increased vaginal discharge. These symptoms have usually been present over several days or weeks, typically beginning around 14 to 20 weeks of gestation. A slight change in the color (from clear, white, or light yellow to pink, tan, or spotting) and consistency (thinner) of vaginal discharge is also consistent with cervical ripening from any cause The cervix should be visually examined at the visit and its length measured by U/S in the second trimester(at 15-17w). Frequent cervical examination in the second trimester will aid in determining if either cerclage is necessary in the short term or C-section is necessary in the long term. Placment of cervical cerclage环扎术 should be performed in the second trimester, 13-17w. Cerclage removal should take place at 36-37w after fetal lung maturity has taken place but before the usual onset of spontaneous labor that could result in avulsion of the suture. C-section is indicated if cervical stenosis makes vaginal delivery difficult. From up-to-date I. Candidates for history-indicated cerclage — A minority of recurrent second trimester losses/births are primarily, and perhaps exclusively, caused by congenital or acquired structural weakness of the cervix, and can be treated effectively with support by a “history-indicated” cerclage. Anatomical, biochemical, and clinical evidence from observational studies and randomized trials consistently support this hypothesis [19-22]. We suggest history-indicated cerclage at 12 to 14 weeks for women who meet all of the following criteria: • Two or more consecutive prior second trimester pregnancy losses or three or more early (<34 weeks) preterm births. • Risk factors for cervical insufficiency. As discussed above, these risk factors include a history of cervical trauma and/or short labors or progressively earlier deliveries in successive pregnancies • Other causes of preterm birth (eg, infection, placental bleeding, multiple gestation) have been excluded. We also treat these women with 17-alpha-hydroxyprogesterone caproate weekly from 16 to 36 weeks of gestation. II. Candidates for ultrasound surveillance and possible ultrasound indicated cerclage — The majority of women with suspected cervical insufficiency do not meet the above criteria for history-indicated cerclage. For these women, we usually initiate TVU cervical length screening, administer 17-alpha-hydroxyprogesterone caproate prophylaxis, and apply a cerclage if cervical length decreases to <25 mm, We usually initiate cervical length screening at 14 weeks, but may screen as early as 12 weeks in women with early second trimester losses, recurrent second trimester losses, or prior large cold knife conization |
|
|
Contraception --- pt with sickle-cell disease
|
Pregnancis in pt with sickle-cell disease are associated with a very high risk of complications (acute crisis, endometrial infection, pyelonephritis and thrombombolic events), therefore, pt with sickle-cell disease need a safe and reliable method for contraception to prevent undesired pregnancies.
Depot medroxyprogesterone appears to be safe and effective in preventing pregnancies in those pt (progesterone-only pills may lead to a significant blood loss which may aggravate the anemia in these pt). The most common cause of secondary amenorrhea is pregnancy. Drugs that induce the cytochrome P450 system can reduce oral contraceptive efficacy. Numerous antisizure medications (phenytoin, carbamazepine, ethosuximide, Phenobarbital, topiramate) are known to decrease the efficacy of OCPs. |
|
Pruritus
|
Pruritus is a very common complaint during pregnancy. Common pruritic locations are the scalp, anus, vulva and abdomen (during the 3rd trimester)
|
|
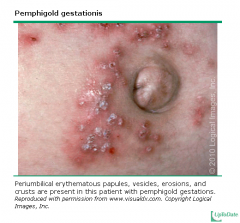
Herpes gestationis
|
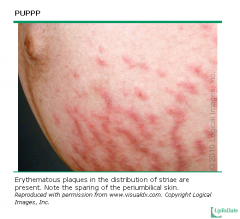
(pemphigoid gestationis) is an uncommon blistering起水泡dermatosis that is associated with pregnancy. It typically starts during the 2nd or 3rd trimester or postpartum period. It may first manifest as abdominal pruritis, a relatively common benign condition during pregnancy, with later development of a rash. The rash is localized around the umbilicus and is characterized by papules, urticarial plaques and vesicles, although bullae may also form.
Contrary to its name, herpes gestationis is not caused by a viral infection, and is believed to be an autoimmune disorder. DD: PUPPP (papules and plaques of pregnancy) often begins in the striae gravidarum, while pemphigoid gestationis is truly periumbilical. Immunofluorescent studies can definitively differentiate these two entities (herpes gestationis factor," an IgG1 antibody that can fix complement at the basement membrane zone) Tx: topical steroid (triamcinolon) /antihistamine |
|
|
Delivery of twins
|
Once the first twin is delivered, the positioning and heart rate of th second twin must be assessed with U/S. If labor has haltd, oxytocin should be administered.
The second twin does not have to b delivered within a fixed time frame after the first twin, Expectant management suffices for the spontaneous deliveries of most twins, but electronic fetal monitoring and U/S are of significant help in promptly recognizing fetal distress when it does occur. |
|
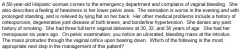
Uterine prolapse
|
Uterine prolapse is typically sen in multiparous, postmenopausal woman with a h/o multiple vaginal dliveries. The injury to the pelvic ligaments and loss of estrogen wakens the endopelvic fascia. The uterus and cervix descend down the vaginal canal towards the vaginal orifice (introitus).
Pt c/o a sensation of pressure or heaviness in the pelvic area, which is relieved by lying down and aggravated by prolonged standing or exertion. Some pt may c/o low back pain, dyspareunia or a visible mass at the introitus. In chronic cases. pt may have bleeding or discharge from ulcerative, superficial epithelium. Tx: All symptomatic pt should have surgical correction of the defect in th pelvic support. |
|
|
Trichomonas-Lactation
|
Lactating women infected with trichomonas should be treatd with metronidazole 2g PO for 1 dose. Breasteeding is thn discountinued briefly for 12-24h thereafter.
|
|
|
Pregnancy risk catgory
|
Category A
Controlled studies in women fail to demonstrate a risk to the fetus in the first trimester (and there is no evidence of a risk in later trimesters), and the possibility of fetal harm appears remote. Category B Either animal-reproduction studies have not demonstrated a fetal risk but there are no controlled studies in pregnant women, or animal-reproduction studies have shown an adverse effect (other than a decrease in fertility) that was not confirmed in controlled studies in women in the first trimester (and there is no evidence of a risk in later trimesters). Category C Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal or other) and there are no controlled studies in women, or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus. Category D There is positive evidence of human fetal risk, but the benefits from use in pregnant women may be acceptable despite the risk (e.g., if the drug is needed in a life-threatening situation or for a serious disease for which safer drugs cannot be used or are ineffective). Category X Studies in animals or human beings have demonstrated fetal abnormalities, or there is evidence of fetal risk based on human experience or both, and the risk of the use of the drug in pregnant women clearly outweighs any possible benefit. The drug is contraindicated in women who are or may become pregnant. |
|
|
Lesbian womn
|
have a lower risk of acquiring HPV infection and a lower chance of developing CIN and invasiave cervical carcinoma, a lower risk of contracting syphilis and Chlamydia infections than heterosexual or bisexual women.
|
|
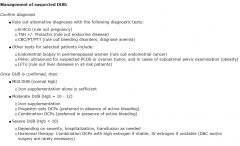
Dysfunctional uterine bleeding
|
Tx: Hormonal therapy to stabilize the endometrium
Estrogen should be used in all pt who are actively bleeding as it promotes hemostasis. High dose estrogen followed by progestin is the treatment of choice. For less severe cases, OCPs in does 3-4 times the regular doses can be used as an alternative. Iv conjugatd estrogen is used in pt who can not tolerate oral medications and in unstabl pt with severe bleeding as it can induce hemostasis rapidly. Progestin-only therapy is used for girls with moderate bleeding who can not tolerat or have contraindications to estrogen therapy. Dilation and curettage is used in rare situations where the pt continues to bleed excessively despite hormonal treatment or in pt who ar unable to take estrogen. |
|
|
Emergency contraception
|
Levonorgestrel is the recommended method of emergency contraception if used soon enough after an unprotectd sexual intercourse. It has maximal efficacy when used within the first 12h after intercourse, good efficacy within 48h and appears to work up to 120h.
Levonorgestrel seems to be more effective than thinly estradiol/ Levonorgestrel combination or high does estrogen. It also has fewer side effects. If > 120h, use copper intrauterine device. |
|
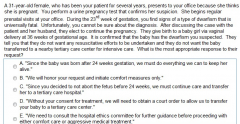
Stress urinary incontinence
|
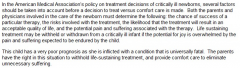
This history, physical examination and clinical stress testing are usually sufficient to diagnose stress urinary incontinence.
It is the most common cause of urinary incontinence in youngr females and occurs due to inadequate urthral support from th fascia and muscles. In a clinical stress tst, the pt is askd to relax and give a single vigorous cough. Leakage that occurs instantaneously with coughing is virtually diagnostic of stress urinary incontinence. |
|
|
Stress urinary incontinence
|
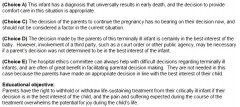
|
|
|
Vaginitis
|
Clinical features of vaginitis are very nonspecific and the dx should always be confirmed by microscopy to avoid inappropriate treatment. This is important to avoid frequent misdiagnosis and inappropriate treatment. The most commonly used techniques are saline and KOH preparation for microscopy. The vaginal secretions hav pseudohyphae in candidiasis, bacterial vaginosis is confirmed by the presence of clue cells in the smear. Motile trichomonads and an abundanc of polymorphonuclear cells are found in pt with trichomoniasii.
|
|
|
Septate uterus
|
Second-trimester spontaneous abortions are the typical problems associated with septate uterus. Surgical removal of the septum has been shown to b effective in treating second-trimester complications, however it is not usually effective in correcting first trimester complications associated with the septate uterus.
Septate uterus may raise the risk of poor implantation on a poorly vascularized and inhospitable不适居留的surface. Surgery is unlikely to correct infertility. |
|
|
Septic abortion
|
Febrile, tachycardic, hypotension, bloody, purulent vaginal discharge and a dilatd cervix
It is common complication of illegal abortion and can result in salpingitis, peritonitis and death I not treatd promptly. Tx: stabilize the pt, blood and endometrial culuture, initiat broad-spectrum parentral antibiotics (clindamycin+gentamicin+ampicillin or piperacillin-tazobactam or imipenem), surgically evacuate the uterine contents. |
|
|
breech presentations
|
Most of the breech presentations assume a cephalic presentation by 36-weeks gestation.
|
|
|
Hypercalcemia
|
is not associated with specific physical findings. There may be anxiety, depression, mild muscular weakness, constipation and peptic ulcer disease.
Hypocalcemia: Chvostk’s or Trousseau’s sign, hyperpigmntation, seizures, muscular weakness or hypotension., hypractive deep tendon reflex (hypermagnesmia---loss of deep tendon reflex) |
|
|
Euvolemic hypoosmolar hyponatremia
|
can be due to SIADH, hypothyroidism or adrenal insufficiency. If the pt is asymptomatic or the hyponatremia is mild (125-135mEq/L), treatment is first directed at correcting the underlying disorder (corticosteroid or levothyroxine).
Moderate hyponatremia and SIADH respond to water restriction. Symptomatic pt and those with severe hyponatremia may need sodium replacement using hyprtonic saline solution. In pt with symptomatic or severe hyponatremia (Na <115mq/L), an aggressive initial correction at th rate of 1.5-2 mEq/L/hour for th irst 3-4h is indicated. Hypertonic saline should be used initially in this setting for rapid correction of hyponatremia. The plasma sodium levels should be monitored frequently to avoid raising sodium levels > 12mEa/L in the first 24h. Administration of hypertonic saline is limited to patients with symptomatic or severe hyponatremia. |
|
|
hepatic encephalopathy
|
The common cause of hepatic encephalopathy
1. GI bleeding 2. Hypokalemia (associated with loop diurectics) 3. Hypovolemia 4. Hypoxia 5. Sedatives or tranquilizer 6. Hypoglycemia 7. Metabolic alkalosis 8. Infection (including spontaneous bacterial peritonitis) Intravenous potassium must be given immediately when hypokalemia is found in certain situations. Such as HE, ventilatory failure, and cardiac arrhythmia. In these cases, fast potassium replacement is critical to the pt’s recovery and prognosis. |
|
|
Hyperkalemia
|

|
|
|
Splenic sequestration crisis —
|
— With splenic sequestration crisis, vaso-occlusion within the spleen and splenic pooling of red cells produce a marked fall in hemoglobin concentration accompanied by persistent reticulocytosis and a rapidly enlarging spleen. There is a risk of hypovolemic shock, particularly in children. Although primarily associated with aplastic crisis, parvovirus B19 infection may also be a risk factor for splenic sequestration
The subjects who are susceptible to this syndrome are those with SCD whose spleens have not yet undergone fibrosis secondary to multiple episodes of splenic infarction. Sequestration can occur as early as a few weeks of age and may cause death before sickle cell disease is diagnosed A complete blood count should be obtained immediately in sickle cell disease pt who p/w abdo pain and splenomegaly, as this pt group is at risk for developing splenic sequestration crisis (SSC). In SSC, a dramatic fall in hemoglobin concentration occurs secondary to vaso-occlusion within the spleen and splenic pooling of RBC. Typically the spleen rapidly enlarges and th pt can go on to experience hypovolemic shock. Pt with SSC who do not receive blood transfusion in time have a mortality rate o 10-15%. |
|
|
Sickle cell crisis
|
It is the most common type of vasocclusive event in pt with sickle cell disease. Although most of these crises have no identifiable cause, events such as dehydration, cold, infection, stress, menses, alcohol consumption and nocturnal hypoxemia are known triggers
The first step in management of pt presenting with an acute painul episode is the administration of fluids orally or iv to ensure optimal hydration. |
|
|
head and neck cancers
|
About 60% of head and neck cancers are locally advanced at the time of diagnosis and are inoperable. Combined chemotherapy and radiotherapy promises superior results than chemo or radio alone.
|
|
|
primary CNS lymphoma.
|
The degree of immunosuppression (CD4 count) seems to be the major determinant of the survival in pt with primary CNS lymphoma.
|
|
|
Metoclopromide
|
(dopaminergic antagonist, D2 blocker) are occasionally used for chemotherapy-induced N&V. Its use has been associated with extrapyramidal symptoms: akathisia, dystonia and parkinsonian-like symptoms. Metoclorpromide has now been largely replaced by 5 HT3 serotonin receptor antagonist(ondansetron) and aprepitant.
|
|
|
colon cancer,
|
There is strong correlation between alcohol intake and the development of colon cancer, especially in those individuals consuming 45 grams or more alcohol per day (12 oz beer=13g).
|
|
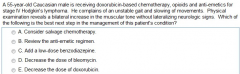
ITP
|
Corticosteroid therapy is the treatment of choice for ITP. Most adults respond to steroids within 2w, with most pt responding within the first week. IVIG can be used if steroids fail, in pt with life-threatening bleeding (GI or CNS bleeding)or in preparation for surgery (splenectomy.) Splenectomy is rarely performed in refractory cases.
|
|
|
HIT
|
Type I: within 2d of initiation of heparin therapy and is usually associated with a lesser degree of fall in the platelet count (nadir platelet count of 100,000/ul). The platelet count usually returns to normal with discontinuation of heparin and there are no clinical consequences.
Type II: more serious immune-mediated disorder, antibodies against heparin-platelet factor 4 comples, bind to platelet surface, activate platelet and aggregate----thrombocytopenia and platelet-rich clots, develop 4-10d after the initiation of heparin therapy. Platelet count: 30,000-60,000/ul. Spontaneous bleeding is UNUSUAL. Immune-mediated HIT is associated with both venous and arterial thrombosis. The major manifestations of venous thrombosis are DVT, PE, venous limb gangrene and cerebral sinus thrombosis. Arterial thrombois can lead to stroke, MI and limb and organ (kidneys, mesenteric) ischemia. Exposure to both heparin and warfarin should be discontinued in pt with HIT, They should be anticoagulated with direct thrombin inhibitors(argatroben or lepirudin) for the prevention or treatment of thromboembolic complications. The choice of agent depends on the coexisting medical conditions. Lepirudin should be used with caution in pt with renal insufficiency while the dose of argatroban should be adjusted in pt with hepatic dysfunction. Low molecular weight heparin should NOT be substituted for unfractioned heparin because it can also cross react with heparin-induced antibodies and induce more antibody formation |
|
|
Platelet dysfunction in pt with renal dysfunction
|
Platelet dysfunction is the major contributor of increasing bleeding tendency in pt with renal failure. Correction of platelet dysfunction is necessary in pt with active bleeding or those who are about to undergo a surgical prodecure. Several available options to correct the abnormality incude the following: correction of anemia, administration of desmopressin, dialysis, estrogen treatment, and cryoprecipitate infusion. Desmopressin represents the simplest and least toxic acute treatment of prolonged bleeding time. It acts by increasing the release of factor VIII: von Willebrand factor multimers from endothelium.
Cryoprecipitate infusion use is limited to pt who are not responding to blood transfusion and desmopressin. |
|
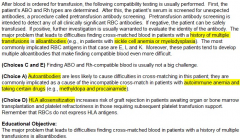
Alloantibodies in pt with h/o multiple transfusion
|

Pt who requires chronic RBC transfusion may form multiple antibodies to common Rh, Kell or other blood group antigens. The presence of such antibodies may increase the time required for a transfusion service to supply serologically compatible red cells, If undetected, these RBC antibodies may cause hemolysis, but severe hemolytic reactions are uncommon, In this case, the transfusion should be stopped immediately, and vigorous hydration should be started to treat the hypotension and to prevent renal failure. Low dose dopamine infusion and osmotic diuresis may also be employed.
|
|
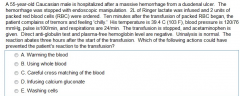
Alloantibodies in pt with h/o multiple transfusion
|
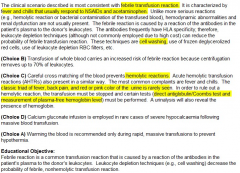
|
|
|
Immunologic blood transfusion reactions
|
1. FEBRILE NONHEMOLYTIC REACTIONS — The most common transfusion reaction is a febrile, nonhemolytic transfusion reaction (FNHTR). The clinical manifestations of this reaction include fever, often a chill, and sometimes mild dyspnea within one to six hours after transfusion of red cells or platelets. FNHTRs are benign, causing no lasting sequelae, but are uncomfortable and sometimes frightening to the patient. Furthermore, since fever, with or without a chill, also may be the sign of a severe, acute hemolytic transfusion reaction (see below) or infection, FNHTRs cannot be ignored. It is associated with class I HLA antibodies
Tx: 1).Stopping the transfusion and determining that a hemolytic reaction is not taking place, 2).Administration of antipyretics (aspirin should be avoided in thrombocytopenic patients) and moderate doses of meperidine in patients with severe chills and rigors Prevention — It is the general consensus that FNHTRs can be avoided or minimized by using leukoreduction to reduce the number of leukocytes transfused 2. ACUTE HEMOLYTIC REACTIONS It is a medical emergency that results from the rapid destruction of donor erythrocytes by preformed recipient antibodies. AHTRs are usually due to ABO incompatibility, most often the result of clerical or procedural error. Some acquired alloantibodies, such as anti-Rh or anti-Jka, are occasionally implicated, but AHTRs more typically occur when a group O recipient is transfused with non-group O red cells. These reactions involve naturally occurring IgM anti-A and anti-B, which fix complement and cause rapid intravascular hemolysis. This may lead to disseminated intravascular coagulation (DIC), shock, and acute renal failure due to acute tubular necrosis. Clinical presentation — The classic presenting triad of fever, flank pain, and red or brown urine (ie, hemoglobinuria) is rarely seen. Fever and chills may be the only manifestations and, in patients under anesthesia or in coma, DIC may be the presenting mode, with oozing of blood from puncture sites and hemoglobinuria. The plasma of a patient with an AHTR will generally be pink (plasma free hemoglobin >25 to 40 mg/dL) and the direct antiglobulin (Coombs) test will be positive, unless all of the transfused red cells have already been destroyed and/or removed at the time of testing. Initial approach — As noted above, fever is also the presenting sign of a "benign" FNHTR. Thus, whenever fever occurs after a red cell transfusion, one must first rule out a hemolytic transfusion reaction and take the following steps: • Stop the transfusion, but leave the intravenous line attached. The bag containing the transfused cells, along with all attached labels, should not be discarded, as repeat typing and cross-matching of this unit by the blood bank will most likely be required. • Maintain the patient's airway, blood pressure, and heart rate. • Begin an infusion of normal saline immediately to initiate a diuresis and avoid hypotension (see below). Avoid the use of Ringer's lactate solution because its content of calcium may initiate clotting of any blood remaining in the intravenous line. Avoid dextrose- containing solutions because the dextrose may hemolyze any of the remaining red cells in the line. • From the other arm, obtain a sample for a direct antiglobulin test, plasma free hemoglobin, and repeat type and cross-match. Save a urine sample for hemoglobin testing. • The blood bank should be alerted immediately, and a search for clerical error should be instituted. Every hospital has a protocol for evaluating transfusion reactions, which should be rigorously followed. This is of critical importance, since if blood samples or blood bags have been switched in error, there may be a second patient at risk for a similar event (ie, if patient A received blood meant for patient B, then patient B may receive the blood meant for patient A). Treatment — If there is any suggestion (eg, clerical mistake, hypotension, pink plasma or urine) that an AHTR is possible, and even before laboratory tests are available, generous fluid replacement with saline (100 to 200 mL/hour) to support a urine output above 100 to 200 mL/hour should be initiated immediately, in an attempt to prevent the development of acute oliguric renal failure. Vigorous supportive care is also important for the treatment of AHTRs. If there has been massive hemolysis and clinical or laboratory signs of disseminated intravascular coagulation, cautious and early heparinization (10 U/kg per hour) for the next 12 to 24 hours may be of value, although there are no recent studies on the effectiveness of this intervention. A vasopressor such as low-dose dopamine may be required. If massive intravascular hemolysis has already occurred, hyperkalemia is likely and cardiac monitoring and acute hemodialysis may be required. Accordingly, the patient's renal function and coagulation profile (eg, prothrombin time, partial thromboplastin time, fibrinogen, platelet count) should be monitored frequently |
|
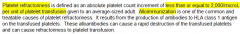
Platelet refractoriness
|
The post-transfusion platelet count should be measured 10-60min after the completion of transfusion. Each unit of platelet transfused should cause an immediate post-transfusion rise in the platelet count by >5,000/ul, Platelet refractoriness due to alloimmunization should be considered if platet transfusion fails to cause the expected increment in the platelet count.
A platelet count with a normal increment of one hour after transfusion, but with a rapid return to baseline within 24 hours indicates reduced platelet survival in the circulation, This is typically seen in pt with DIC, sepsis, active bleeding or in pt who use drugs that reduce platelet survival. |
|
|
Polycythemia
|
Hemoglobin >18.5 g/dL in M and 16.5g/dL in F
Serum erythropoietin is a good initial dx test for the evaluation of polycythemia and helps to guid the remainder of the work-up. A low erythropoietin level suggests polycythemia vera, where a high erythropoietin level suggests a secondary cause of polycythemia, such as chronic hypoxia or a hormone-producing neoplasma (renal cell carcinoma). Treatment of secondary polycythemia should be directed towards the underlying cause. Workup CBC, erythropoietin, UA, carboxyhemoglobulin, nocturnal oximetry, bone marrow biopsy, JAK2 mutation |
|
|
Multiple myeloma
|
A complete skeletal series (skull, long bones and spine, a whole body X-ray) should be performed once a pt has been diagnosed with multiple myeloma to identify impending pathological fractures. Conventional skeletal surveys reveal punched-out lytic lesions, diffuse osteopenia or fractures in nearly 80% of pt at the time of diagnosis.
Bone scans are not useful for these pt. Bone scans primarily detect blastic lesions like metastatic prostate cancer (NOT lytic lesions). Furthermore, technetium-99m bone scanning is much less sensitive for lytic lesions compared to conventional roentgenography and is therefore not recommended. Multiple myeloma pt usually do not have elevated bone alkaline phosphatase levels. Hyperviscosity syndrome results from increased serum viscosity due to high protein content. It can be observed in pt with multiple myeloma, although it is more commonly seen in Waldenstrom’s macroglobulinemia as a result o increased amounts of IgM. Serum hyperviscosity impairs microcirculation in the brain and cause headache, dizziness, vertigo, nystagmus, hearing loss and visual impairment. In severe cases, somnolence, coma and seizures may result. Mucosal hemorrhage is also typical due to impaired platelet function. |
|
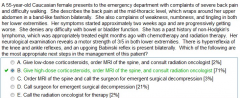
Flutamind—leuprolide for pt with metastatic prostate cancer
|
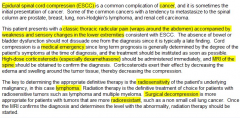
Androgen depletion is the primary treatment for men with a metastatic prostate cancer. It is usually palliative rather than curative and most pt lose the responsiveness to hormonal manipulations within 2y. In most cases , LHRH agonist (leuprolide) are used as the irst line therapy or advanced metastatic prostate cancer. These bind to the LHRH receptors in the anterior pituitary gland and cause an initial release of LH and FSH, which causes a transient rise of testosterone levels. After approximately one week of continuous therapy, there is down regulation of LHRH receptors, causing a decrease in the levels o LH. This leads to a significant decrease in the testosterone levels. In the first week of therapy, the patient’s symptoms tend to get worse during the initial testosterone surge.
LHRH agonist monotherapy is contraindicated in pt with painful vertebral metastases and severe ureteral obstruction. These symptoms get worse during the initial testosterone surge seen in the first week of therapy. In such cases, an antiandrogen (flutamide) is given for one week before starting LHRH agonist monotherapy to block the effects of the initial testosterone surge. ****** External beam radiation therapy should be used for pain alleviation in pt with single or few focal bone metastatic lesions due to hormone-refractory prostate cancer. Corticosteroids reduce inflammation by inhibiting prostaglandin synthesis. These drugs are only useful when inflammation or edema surrounding the tumor causes pain secondary to compression or visceral distention. These are also useful in pt with epidural spinal cord compression. |
|
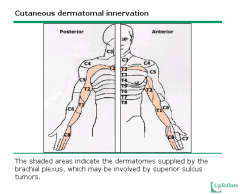
Pancoast’s tumor (Superior sulcus tumors)
|
Spinal cord compression develops in up to 25% of pt with Pancoast’s tumor duing the course of the disease.
Shoulder pain is the most common initial presentation of Pancoast’s tumor. Lesions in the superior sulcus may result in shoulder and arm pain (in the distribution of the C8, T1, and T2 dermatomes), Horner's syndrome, and weakness and atrophy of the muscles of the hand, or pain and paresthesia of the fourth and fifth digits and the medial aspect of the arm and forearm. Abnormal sensation and pain in the T2 territory (the axilla and medial aspect of the upper arm) may also be an early finding, and the triceps reflex may be lost a constellation of symptoms referred to as Pancoast's syndrome. The majority of patients with superior sulcus tumors present with one or more of these complaints. Due to the peripheral location of the tumor, pulmonary symptoms such as cough, hemoptysis, and dyspnea are uncommon until late in the disease. Superior sulcus tumors invade the intervertebral foramina early in the course of disease in approximately 5 percent of patients and may cause spinal cord compression and paraplegia. Approximately 25 percent of patients ultimately develop spinal cord compromise Chest movement asymmetry and asymmetric lower extremity deep tendon reflexes indicated phrenic nerve involvement and possible invasion of the intervertebral foramina. These are dangerous signs because these may quickly result in spinal cord compromise and need immediate therapy. |
|
|
Superor vena cava syndrome (SVCS)
|
The best diagnostic test for SVCS is a contrast CT scan of the neck and chest, which will reveal an obstruction of the superior vena cave due to the pulmonary mass, the metastatic nodes and an intravenous thrombus. CT scan is very useful because it can reveal the extent of obstruction and provide a histopathologic diagnosis (via percutaneous biopsy), which will determine the particular therapeutic regimen required to manage the underlying malignancy.
80% of SVCS are due to bronchogenic carcinoma. Dyspnea, persistent cough, facial fullness and neck pain and progress into hoarseness, dysphagia, chest pain and syncope. PE: edema and erythema of the neck, dilated veins of the arms and neck, advanced cases is manifested by cyanosis, collateral veins in the thorax, ocular proptosis and lingual edema. |
|
|
Tamoxifen – Breast cancer
|
Tamoxifen use is associated with the development of endometrial hyperplasia and cancer. Most of these cancers are localized, stage I lesions and are seen in women > 50y.
It is recommended that Premenopausal women on tamoxifen do NOT require any additional testing except for an annual gynecologic examination, a detailed history and routine Pap smear. Postmenopausal women just need annual gynecologic exam with further investigation (either tranvaginal ultrasound or endometrial biopsy) if they have abnormal bleeding or vaginal symptoms. A transvaginal U/S(TVUS) in asymptomatic women is associated with significant false positive results which require unnessary subsequent endometrial sampling. |
|

Anemia of chronic disease (ACD)
|
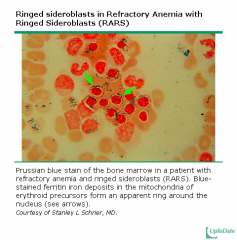
The anemia is usually normocytic and normochromic, although it may become microcytic and hypochromic in long-standing cases. The absolute reticulocyte count is frequently low.
Low serum iron + elevated ferritin levels + normal/low transferring saturation + low transferin level Bone marrow: normal/increased amounts of storage iron in the macrophages and a decreased number of sideroblasts. bone marrow macrophages contain normal or increased amounts of storage iron, reflecting reduced macrophage iron export. In addition, erythroid precursors show decreased or absent staining for iron (ie, decreased numbers of sideroblasts), reflecting reduced availability of iron for red cell production. Sideroblasts are atypical, abnormal nucleated erythroblasts (precursors to mature red blood cells) with granules of iron accumulated in perinuclear mitochondria. Sideroblasts are seen in aspirates of bone marrow. Treatment of ACD: 1. treat underlying disease, frequent follow-up visits 2.Erythropoietin injection if erythropoietin < 500 mU/ml 3.if anemia is severe, blood transfusion. Sideroblastic anemia or sideroachrestic anemia is a disease in which the bone marrow produces ringed sideroblasts rather than healthy red blood cells (erythrocytes). It may be caused either by a genetic disorder or indirectly as part of myelodysplastic syndrome, which can evolve into hematological malignancies (especially acute myelogenous leukemia). In sideroblastic anemia, the body has iron available but cannot incorporate it into hemoglobin, which red blood cells need to transport oxygen efficiently. Dx: Bone marrow shows erythroid hyperplasia with a maturation arrest. In excess of 40% of the developing erythrocytes are ringed sideroblasts. Serum iron, percentage saturation and ferritin are increased (only form of microcytic anemia in which the circulating iron level is increased). The TIBC is normal to decreased. Stainable marrow hemosiderin is increased. The diagnostic hallmark of the sideroblastic anemias is the presence of ring sideroblasts. The amount of iron in bone marrow macrophages is strikingly increased, due to the presence of ineffective erythropoiesis (intramedullary hemolysis) |
|
|
Neutropenic fever
|
in any pt should be considered a medical emergency. The pt can have a serious and life-threatening infection, even in the absence of typical signs and symptoms.
|
|
|
The anemia of pt with end stage renal disease
|
is generally due to erythropoietin deficiency. Other causes of anemia should be ruled out before starting erythropoietin therapy. Iron-deficiency anemia is a common cause of suboptimal increase in hematocrit and hemoglobin level following erythropoietin therapy. Blood transfusion is usually avoided in pt with end stage renal disease because they can sensitize a pt for allograft rejection following kidney transplantation.
|
|
Lung cancer
|
Accurate histological identification and staging of the tumor, along with preoperative physiologic assessment of lung function is an important initial step in the optimal management of pt with lung cancer.
An initial CT scan should be obtained in all pt with lung cancer. |
|
|
Trimethoprim, methotrexate and phenytoin
|
can interfere with folate metabolism and result in folic acid deficiency anemia.
Tx: folinic acid (Leucovorin: folinic acid is more potent than folic acid) |
|
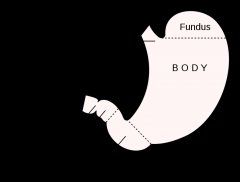
Autoimmune metaplastic atrophic gastritis (AMAG)
|
1. glandular atrophy, mainly affects the gastric body and fundus, little changes are observed in the gastric antrum (absent rugae in the fundus)
2. intestinal metaplasia and inflammation 3. Autoantibody against oxyntic cells and intrinsic factor, associated with pernicious anemia. |
|
|
Lobular carcinoma in situ (LCIS)
|
LCIS is noninvasive lesion that arises from the lobules and terminal ducts of the breast. It almost always represents an incidental finding that is diagnosed on a breast biopsy that is performed for some other reason, such as an area of fibrocystic change or a fibroadenoma. In most instances, LCIS is not identified clinically, mammographically, or by gross pathologic examination While the lesion itself has no malignant potential, it signiies an increased risk of developing invasive lobular or ductal carcinoma in either breast (7-18 times the risk of the general population). It is not considered premalignant lesions, as the cancers that subsequently develop may occur anywhere in the breasts, not necessarily at the site of the atypia. Therefore, when these high-risk lesions are discovered, the focus should be on careful surveillance and consideration of risk reduction strategies, as opposed to directed therapy towards the lesion
It is recommended that cases where LCIS is diagnosed by needle biopsy proceed to excisional biopsy (A surgical procedure in which an entire abnormal area is removed for diagnostic examination under a microscope) since up to 38% of cases may be upstaged to ductal carcinoma in situ(DCIS) or invasive cancer when the entire lesion is removed. The most common management course is follow-up surveillance. Chemoprevention with selective estrogen receptor modulators (SERMs) such as tamoxien or raloxifene, is an alternative option. Some pt may request prophylactic bilateral mastectomy which is also a viable alternative. — If LCIS is identified by a core needle biopsy, an excisional biopsy must be performed to exclude an associated malignancy. Observational studies have identified DCIS or an invasive cancer in approximately 15 to 38 percent of patients with LCIS. — — If the LCIS is diagnosed on an excisional breast biopsy, no further surgery is required. Wide surgical excision with histologically negative margins (ie, lumpectomy) is not needed since LCIS is often multicentric and is not managed as a precursor lesion [50,82,83]. If an invasive carcinoma is detected, appropriate management should be initiated. |
|
|
Ductal carcinoma in situ (DCIS)
|
DCIS of the breast represents a heterogeneous group of neoplastic lesions confined to the breast ducts and lobules. The diagnosis of DCIS has increased dramatically with the introduction of screening mammography.
Therapeutic approaches include surgery, radiation therapy, and adjuvant endocrine therapy. |
|
|
Whole brain radiation therapy
|
Whole brain radiation therapy is the mainstay of treatment of multiple brain metastases
|
|
|
SLE
|
Premature atherosclerosis is the most common cause of myocardia infarction in SLE pt. Coronary atherosclerosis is being increasingly recognized a cause of morbidity and mortality in SLE pt, especially in young pt who had long-standing disease and had been on corticosteroids.
|
|

Paget’s disease
|
is usually diagnosed incidentally on a radiograph that shows thickened bone with inhomogenous density or “cotton wool” appearance. Pt may also present with an elevated ALP with normal Ca and no sign of hepatobiliary pathology.
X-ray: Plain films early in the disease course may show a predominantly osteolytic lesion. Over time, however, there is evidence of an osteoblast response, and the bone thickens and enlarges A radionucleotide bone scan is also an effective test for diagnosing Paget’s disease due to its high metabolic turnover. It is a disease of increased bone turnover. It is characterized by an accelerated rate of bone remodeling, resulting in overgrowth of bone at a single or multiple sites and impaired integrity of affected bone. Commonly affected areas include the skull, spine, pelvis, and long bones of the lower extremity. The majority of patients with Paget disease of bone are asymptomatic. The diagnosis in such patients is usually made incidentally following a routine chemistry screen showing an elevated serum concentration of alkaline phosphatase of bone origin or an imaging study obtained for some other reason that shows pagetic changes in bone. The two main clinical manifestations of Paget disease are pain due to the pagetic lesion in bone itself or from secondary consequences of bone overgrowth and deformities in affected areas, such as osteoarthritis or nerve impingement. Fractures, bone tumors, neurologic disease, and abnormalities in calcium and phosphate balance can also occur. In addition, because of the vascularity of pagetic bone, excessive bleeding may occur during orthopaedic surgery. Hearing loss is a common complication in pt with Paget’s disease and is thought to be secondary to compression of auditory nerve or involvement of the cochlear and/or cochlear capsule. Treatment with calcitonin or bisphosphates can slow the progression of hearing loss, but is unlikey to reserve hearing loss that has already occurred. |
|
|
Chronic glucocorticoid therapy
|
VitD+Ca, check bone densitometry every year
Bisphosphonates can be added if the risk of osteoporosis is very high especially in postmenopausal women. Caution should be exercised when prescribing these to premenopausal women given the possible teratogeni risk. Treatment could be warranted if bone mineral density studies reveal a T score of <-1.5 that continues to rapidly deteriorate. Calcitoin is used if the bisphosponate are contraindicated or not tolerated. |
|
|
Polymyositis
|
Proximal muscle weakness with increased CPK levels indicates a muscle disorder. Inflammatory myositis can lead to increased serum ferritin levels, which is an acute first phase protein.
|
|
|
Reiter syndrome
|
People with IBD are routinely warned against taking NSAIDs. The reason to avoid these common over-the-counter painkillers is that they may affect a relapse, or flare-up, of IBD symptoms. Pt with inflammatory bowel disease and Reiter syndrome should be treated with methotrexate, antibiotics and exercise.
|
|
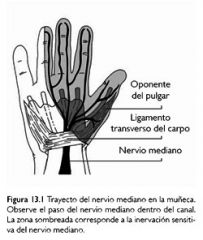
Carpal tunnel syndrome
|
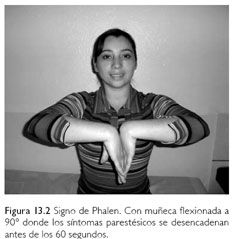
p/w pain, paresthesias or less commonly weakness in the hand. Symptoms are frequently worse at night and may be relieved by shaking the hands or running then under warm water.
Capal tunnel syndrome is associated with a h/o wrist trauma or fracture, DM, rheumatoid arthritis, hypothyroidism, acromegaly, pregnancy, menopause, end stage renal disease and dialysis, obesity and fibromyalgia. It is suggested by specific physical findings, including pain or parestesias after 30-60 sec of acute wrist flexion (the Phalen maneuver) or tapping of the median nerve (Hoffman Tinel test).. Phalen’s test is slightly more sensitive than Tinel’s sign. A hand elevation test is positive if symptoms are reproduced by raising the hands over the head. Nerve conduction studies are frequently used to confirm a diagnosis of Carpal Tunnel Syndrome and can demonstrate changes of focal demyelination (Compression of the median nerve results in loss of normal myelination, axonal loss may also occur if the compression is particularly severe.) in the median nerve at the level of the carpal tunnel and possibly even axonal loss, Nerve conduction studies will demonstrate slowed conduction along the median nerve at the level of the carpal tunnel, with a normal conduction velocity proximally, Reduced amplitudes of nerve conduction can occur if there is axonal loss. Nerve conduction studies are frequently combined with EMG. Nerve conduction studies are helpful to confirm the dx, exclude other etiologies and determine severity of the condition. When standard methods (NASIDS, corticosteroid, splinting) of treatment of carpal tunnel syndrome fail, it is important to focus on occupational rehabilitation as a means of limiting symptom severity. The pressure within the carpal tunnel rises significantly with a number of activities, including wrist flexion and extension, making a fist, holding items, pushing and finger work such as key punching and typing, It is therefore important to minimize these tasks as much as possible in this pt population. In addition, the periodic performance of brief wrist and hand exercises known to reduce intrantunnel pressure should also be recommended. In the majority of pt, conservative treatment is usually enough to relieve the symptoms and prevent the progression of the disease and its complications, Continuous wrist splinting is a simple and effective way to keep the wrist in a neutral position and to reduce the pressue on the nerve in the carpal tunnel. It is especially useful to reduce the nighttime symptoms. A trial of carpal tunnel injection with glucocorticoids may be helpful in pt with persistent pain despite conservative management, however, steroid injection is not a benign procedure. In the wost-case scenario, it can cause permanent nerve injury with a claw hand deformity, therefore this has to be performed by highly-skilled physicians only. |
|
|
Raynaud phenomenon
|
Calcium antagonist, typically nifedipine or amlodipine (dihydropyridine calcium channel blockers), as well as nondihydropyridine diltiazem are considered the first-line pharmacological therapy for pt with Raynaud phenomenon.
Secondary RP — Since a variety of possible insults can disrupt the normal complex regulation of regional blood flow to the digits and skin, the number of disorders associated with RP is extensive. The most common associated disorders are scleroderma, SLE, other connective tissue diseases, occlusive vascular disease, drug effects, hematologic abnormalities, and use of vibrating tools: • Other connective tissue diseases (mixed connective tissue disease, overlap syndromes, polymyositis, dermatomyositis, rheumatoid arthritis, Sjögren's syndrome, undifferentiated connective tissue disease, and vasculitis) • Occlusive vascular disease (arteriosclerosis, atheroemboli, and thromboangiitis obliterans) (see "Thromboangiitis obliterans (Buerger's disease)") • Drug-induced (amphetamines, beta blockers, bleomycin, cisplatin, clonidine, cocaine, cyclosporine, ergot, interferon-alpha, methysergide, nicotine, vinyl chloride, and vinblastine) • Hemorrheologic (Cold agglutinin disease, cryofibrinogenemia, cryoglobulinemia, paraproteinemia, and polycythemia) • Vibration-induced (eg, pneumatic drills and hammers) • Vascular trauma (eg, injury to the distal ulnar artery in the hypothenar hammer syndrome) • Frostbite When managing pt with Raynaud phenomemon, potential precipitating factors such as medications and environmental factors such as frostbite, vibration should be first excluded. The presence of symptoms suggestive of systemic disease (arthralgias, myalgias, fever and weight loss) in pt with Raynaud phenomenon warrants further evaluation, this may include ANA, RF, CBC, blood chemistry, urinalysis and measurement of complement levels. |
|
|
Rotato cuff tendonitis
|
Rotato cuff tendonitis p/w lateral shoulder pain aggravated by movements requiing abduction and external rotation of the shoulder (reaching or lifting the arms up).
Frozen shoulder refers to a stiffened glenohumeral joint, and is most commonly caused by rotator cuff tendonitis. It is suspected when the lateral pain pattern is accompanied by stiffness and a decreased range of motion in abduction and external rotation. Rotato cuff tear is likely if the pain is accompanied by weakness or loss of strength during external rotation or abduction of the shoulder. Anterior should pain is seen in pt with acromioclavicular or glenohumeral joint osteoarthritis and biceps tendonitis. Posterior shoulder pain is the least common pain pattern and is usually a referred pain from the cervical spine. The common causes are nerve impingement due to disc herniation and spinal stenosis at the cervical spine level. Poorly localized pain is usually due to referred pain from the neck, bone structures or nerve compression. |
|
|
Sjogren syndrome
|
Dry eyes (keratoconjunctivitis sicca) and dry mouth (xerostomia).
Complications of dry mouth include dental caries, candidiasis (up to 70% pt: white patches on the buccal mucosa) and chronic esophagitis. Do you wake up at night feeling dry and then drink some water? Do you frequently drink water to help you swallow some dry foods? |
|

Myopathy
|
Myopathy should be suspected in a pt who p/w isolated proximal muscle weakness, particularly in the absence of physical findings to suggest a central nervous system etiology. An EMG should be used to confirm the dx of myopathy, whereas muscle biopsy can help determine the underlying cause.
Nerve conduction and electromyographic (EMG) studies are used when the site of the lesion causing weakness is suspected to be in the peripheral nervous system, the neuromuscular junction, or the muscle itself. The EMG is also of value in directing the site of muscle biopsy. Electromyography (EMG) is the clinical study of the electrical activity of muscle fibers individually and collectively. The desired goal of EMG analysis is the characterization of a disease process as neurogenic or myopathic, or normal Elevations of plasma muscle enzymes (creatine kinase, aldolase, lactate dehydrogenase, and the aminotransferases) are highly suggestive of myopathy. However a negative test does not exclude the dx.They can, however, also be elevated in motor neuron disease or can be induced by strenuous exercise, intramuscular injections, or muscle trauma in the absence of generalized muscle disease. `z Rheumatoid arthritis (RA)-like symptoms with small joint involvement and a weekly positive RF test are especially characterized for parvovirus infecition. RA is unlikely if there is no evidence of synovitis and the symptoms are of less than 6w duration. Viral arthritis is typically self-limited and of short duration. No long-term sequelae are usually observed. |
|
|
Ankylosing spondylitis
|
The most common and important extraarticular manifestations of ankylosing spondylitis are acute anterior uveitis, aortic regurgitation, apical pulmonary fibrosis, IgA nephropathy and restrictive lung disease. Once a dx of ankylosing spondylitis is considered, it is important to search for concurrent extraarticular manifestations.Although they are usually asympotomatic in the initial stages, many pt have restrictive lung disease due to limited costovertebral joint motion and development o apical pulmonary fibrosis. It is important to counsel such pt regarding smoking cessation to prevent early deterioration of lung function.
Radiographs and acute phase reaxtants (i.e. ESR) are used to monitor the disease progression of pt with ankylosing spondylitis. Life expectancy of pt with ankylosing spondylitis is not reduced. Most pt with ankylosing spondylitis do well and have no functional or employment disabilities, |
|

Osteonecrosis
|
Staging — Numerous staging systems for osteonecrosis of the femoral head have been developed since the first one described by Ficat and Arlet, which was based primarily upon radiographic findings. Newer imaging modalities and the need for quantification of involvement have led to these revisions. The Association of Research Circulation Osseous (ARCO) developed a staging system in an attempt to bring uniformity to clinical trials of treatment strategies .
• Stage 0 — All diagnostic studies normal, diagnosis by histology only • Stage 1 — Plain radiographs and computed tomography normal, magnetic resonance imaging positive and biopsy positive, extent of involvement A, B, or C (less than 15 percent, 15 to 30 percent, and greater than 30 percent, respectively). • Stage 2 — Radiographs positive but no collapse, extent of involvement A, B, or C. • Stage 3 — Early flattening of dome, crescent sign, computed tomography or tomograms may be needed, extent of involvement A, B, or C, further characterization by amount of depression (in millimeters) . • Stage 4 — Flattening of femoral head with joint space narrowing, possible other signs of early osteoarthritis |
|
|
Lumbar spinal stenosis
|
The pain disappears/decreases upon sitting down, spine flexion, bends orward (carry a grocery cart)
The pain increases with spine extension Neurogenic (or pseudo) claudication is a hallmark of LSS. This is the tendency for symptoms, usually pain, to be exacerbated with walking, standing, and/or maintaining certain postures, and relieved with sitting or lying. Many patients with LSS are symptomatic only when active. In one systematic review of clinical findings in LSS, neurogenic claudication was moderately sensitive and present in 82 percent of patients . Exacerbation by prolonged standing in an erect posture was an even more sensitive but less specific sign. No pain with sitting was the most specific finding. More than half of patients with LSS also reported relief with sitting or flexion at the waist (squatting, leaning forward), findings that were relatively specific for LSS (84 and 92 percent respectively), but less sensitive. Neurogenic (or pseudo) claudication: claudication, from the Latin for limp, because the patient feels a painful cramping or weakness in the legs. NC should therefore be distinguished from vascular claudication, which is when the claudication stems from a circulatory problem, not a neural problem. Dx: MRI Tx: conservative or a lumbar epidural block. If fail, surgical decompression through a laminectomy. |
|
|
Cyclosporin-gout-transplantation
|
Cyclosporin increases serum uric acid levels by decreasing urate excretion from the kidneys. Joint aspiration will determine the definitive diagnosis of acute monoarthritis in majority of patients.
Acute gouty monoarticular arthritis in renal failure and post-transplant patients is best treated by increasing the dose of systemic steroids or by injection of intraarticular glucocorticoids.The use of NSAID and colchine is not recommended in such pt. Colchincine , concomitant use with azathioprine is associated with significant leucopenia. |
|
|
Rheumatoid arthritis
|
Rheumatoid factor (RF) is only positive in 70-80% of rheumatoid arthritis, so the absenceof RF does not exclude the diagnosis. RF level does not typically change with disease activity and it is possible for pt to have more than mild disease with a negative RF.
Erosions joint disease in rheumatoid arthritis is a clear-cut indication for the use of disease-modifying anti-rheumatic drugs (DMARDs), and methotrexate is the initial drug of choice for this purpose. |
|
|
Acute gount
|
NSAIDs and colchicines are contraindicated in pt with renal failure. Instead, corticosteroids should be used in these pt and can be injected locally in pt with a mono-articular arthritis or given orally in pt with multiple joint involvement.
Contraindication of NSAIDs: renal failure, heart failure, PUD, NSAID allergy Side effect of colchine: diarrhea, abdo cramps, N&V |
|
|
Hypertension in pt with gout arthritis
|
Angiotensin receptor blocker losartan, has a modest uricosuric effect
Furosemide and hydrochlorothiazide should be avoided. |
|
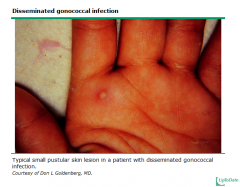
Disseminated gonococcal infection
|
Gonococal arthritis is probably the most common cause of acute non-traumatic mono- and oligoarthritis in young healthy adults. The typical synovial fluid leukycye count in gonococcal arthritis is around 50, 000 cells/mm3, however, cell count below 10,000 cells/mm3 can be present in occasional cases.
In pt with suspected disseminated gonococcal infection, culturing the joint fluid and the mucosal surfaces, including the urethral, cervical, rectal and oral mucosa, should be done. >80% of pt with disseminated gonococcal infection have positive cultures from at least one of the mucosal sites. Synovial fluid culture alone yields positive results in < 50% of pt with gonococcal arthritis. Tenosynovitis is a unique finding in pt with disseminated gonococcal infection, it is very unusual for other forms of infection. The tenosynovitis, dermatitis, polyarthralgia syndrome — Patients with this form of DGI typically present with the following clinical features: • The acute stage of illness is characterized by fever, chills, and generalized malaise. Fever may spontaneously disappear or diminish in magnitude as the disorder progresses. • Tenosynovitis is a unique finding in this form of DGI, and is unusual in other forms of infectious arthritis. Often multiple tendons are simultaneously inflamed, particularly at the wrist, fingers, ankle, and toes. • Dermatitis typically consists of painless lesions that often are few in number. Lesions are usually pustular or vesiculopustular, although hemorrhagic macules, papules, bullae, or nodules rarely occur . Pustular or vesicular skin lesions are often transient and even without treatment may only last for three to four days. Patients may be unaware of the presence of skin lesions. Rarely, patients with DGI can develop lesions that are urticarial or others that resemble erythema nodosum or erythema multiforme . Skin lesions rarely number more than 40; and it is common to find between 2 and 10 lesions in an individual patient. Lesions are rarely present on the face. Although skin lesions and tenosynovitis can spontaneously regress even without treatment, joint involvement will usually progress unless specific treatment is given. The white blood cell count can be elevated or normal in patients with this form of DG |
|
|
Statin --- myopathy
|
• Physical activity can lead to an elevation in serum CPK levels. Unless necessary, serum CPK levels should not be measured following an intense physical activity.
• A mild elevation of CPK levels is common and is not a contraindication to continue treatment with atovastain . You can stop a statin when the CPK level is more than 10 times above the upper limit of normal range. |
|
|
Sjogren’s disease ----- B cell lymphoma
|
Sjogren’s disease results in polyclonal B celll activation and infiltration of the salivary glands. The increased lymphocyte activation can go awry and result in the development o B cell lymphoma in some pt. The lifetime is 5% for Sjorgren’s syndrome ---- much higher than the risk for the general population
|
|

Hemochromatosis
|
Liver dysfunction, central hypogonadism, DM, arthropathy, typical “hook like” osteophytes on X-ray
A fasting transferring saturation over 50% is very suspicious of hemachromatosis. Liver biopsy is the gold standard for diagnosis. Checking or the familial hmachromatosis gene (C282Y and H63D) is very useful for identifying family members who are at risk for developing hemochromatosis. |
|
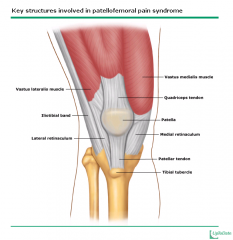
Patello-femoral pain syndrome
|
Most common cause of knee pain in pt younger than 45 years of age and is particularly in women. The syndrome is classified as “overuse ” injury and is also common in athlete. The typical clinical scenario includes anterior knee pain that is provoked by climbing the stairs or prolonged sitting. A PE may reveal retropatellar pain and crepitation on vigorous right patellar compression.
|
|
Low back pain
|
Most pt with low back pain should be managed conservatively with pain control and physical therapy unless there are findings to suggest infection or tumor. Further evaluation with ESR/CRP and lumbar spine radiographs should be done if symptoms last longer than 6w, while MRI should generally be reserved for pt with symptoms greater than 12w in the absence of concerning clinical findings.
|
|
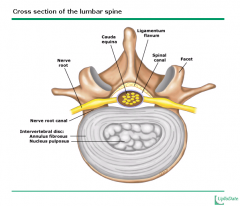
Nerve root irritation
|
The pain is frequently brie and shooting and radiates along the corresponding nerve distribution. It can be provoked by forward bending, coughing or straining and it diminishes on lying down, A positive straight-leg raising test at a 60 degres angle or less is characteristic.
The contralateral (crossed) straight leg raise test refers to passive elevation of the unaffected leg by the examiner. The test is positive when lifting the unaffected leg reproduces radicular pain in the affected leg. It is relatively specific for radiculopathy due to disc herniation, but has poor sensitivity The straight leg raise test is more sensitive but less specific than the contralateral straight leg raise for the diagnosis of radiculopathy due to disc herniation [36]. It is most helpful in the evaluation of radiculopathy at the L5 and S1 levels |
|
|
Rhabdomyolysis
|
CK > 10000U/L, muscle tenderness, increased muscle tone, renal failure, hyperkalemia, hypocalcemia or hyperphosphatemia (celll breakdown)
Cocaine or alcohol intoxication as well as severe trauma or extreme exertion can lead to RM. Neuroleptic malignant syndrome , hypothermia, hypothyroidism and polymoysitis have also been associated with RM. Tx: iv NSS to ensure adenquate hydration, volume replacement must be started as soon as RM is diagnosed or highly suspected., alkalinization of the urine, mannitol and diuresis |
|
|
Varenicline –stop smoking
|
The most commonly used pharmacotherapies for smoking cessation include nicotine replacement, bupropion (antidepressant) and varenicline. Varenicline is a partial agonist of the subunit of the nicotine acetylcholine receptor that controls nicotine dependence. Its side effects is suicidal ideation and erratic or bizarre behavior . It is recommended that pt who have unstable psychiatric symptoms or a h/o previous suicidal ideation avoid the drug and should be considered second-line for any pt with a h/o major depression.
|
|
|
Mammography
|
The current USPSTF guidelines recommend screening mammography, with or without clinical breast examination, every 2 years for women aged 50-74.
There is insuicient evidence to recommend for or against routine clinical breast examination alone as a screening tool for breast cancer.. |
|
|
Sun exposure
|
Sun protection behaviors (clothing), suncreens and maintaining adequate hydration are the key factors to prevent skin damage from sun exposure.
|
|
|
TB exposure
|
PPD testing should be promptly perormed on individuals exposed to active infectious tuberculosis, If the results are negative, the PPD test should be repeated in 3m.
If the results are positive, a chest X-ray should be taken to check for signs of infection, If PPD conversion occurs, monotherapy with INH is necessary. |
|
|
Screening for children at high risk of CAD
|
Children at high risk of developming CAD as adults should be screened soon after they are 2y old. The risk is defined as the presence of family members including parents, grandparent, aunts and uncles having high blood cholesterol or premature CAD.
The rationale behind the cut-off value of 2 years resides in the fact that the diet under this age is high in fat and cholesterol, making it inappropriate and useless to test children <2y. For children >2y, screenin should be as follows 1. If a family member has a total cholesterol > 240 mg/dL, the child should have random cholesterol measured, if this latter is < 170mg/dL, repeat in 5 years, if it is >200 mg/dL, order FLP 2. If the family member has a h/o premature CAD, order FLP (fasting lipid panel) directly High random cholesterol level in a child requires confirmation by repeating the test 1-2 weeks later. ** Your total blood cholesterol is a measure of LDL cholesterol, HDL cholesterol, and other lipid components |
|
|
Increased total serum cholesterol level
|
It is recommended to perform a complete lipid profile in a pt with a total serum cholesterol level of > 200 mg/dL. The pt’s high total cholesterol level can be due to the increase in HDL. VLDL or LDL cholesterol fractions. Increased HDL The primary treatment for increased VLDL cholesterol (increased triglycerides) and increased LDL cholesterol are different, therefore the exact acuse the elevated total serum cholesterol levels must be identified by checking the complete lipid profile in the pt.
Hormone replacement therapy can cause significant hypertriglyceridemia. Drug therapy is not indicated until triglycerides remain significantly elevated despite discontinuation of HRT. |
|
|
Osteoporosis prevention
|
The interventions that have proven to offer more benefit are
Smoking cessation (If smoke >1 pack per day), raloxiene, Ca +VitD, discontinuation of medications such as heparin or glucocoriticoids HRT is extremely effective in osteoporosis prevention, but widespread use is not advisable because of the risk of malignancy or cardiovascular disease._ |
|
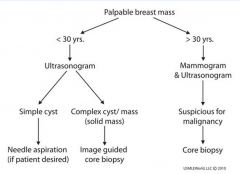
Mass in breast
|
Ultrasound alone is used to evaluate palpable breast lesions in pt <30y, but a combination of both mammography and U/S should be used or pt >30y.. Breast MRI is reserved or certain diagnostic dilemmas but is not recommended or evaluation of palpable abnormalities. MRI is associated with high false positive rates and increases pt anxiety and biops rates for benign lesions.
|
|
|
Alcohol abuse
|
Alcohol is frequently used among pt in their twenties, but it is infrequently discussed with pt as many perceive the activity to be “normal”. However, the rates of alcohol abuse are also higher among pt in their twenties than any other age group.
Alcohol dependence is marked by the presence of > 3 of the following signs or symptoms: tolerance, withdrawal, continued desire to cut down, use in larger amount than intended , considerable time spending revolving around alcohol use, failure to fultill obligations or continued use despite physical problems. |
|
|
Screening for Chlamydia infection
|
The U.S. Preventive Services Task Force (USPSTF) recommends routine screening for Chlamydia infection in all sexually active women age <=24 years, and in other asymptomatic women at increased risk for this infection.
|
|
|
Meningococcal infection prophylaxis
|
Individuals who have been in prolonged close contact (mouth to mouth resuscitation or intubate a pt) with a case of invasive meningococcal infection should be placed on prophylactic antibiotics to eradicate pharyngeal carriage of the organism. Unless there has been directe exposure to respiratory secretions, the majority of hearlthcare workers do not require chemoprophylaxis. Rifampin (600mg PO bid for 4 doses) is the standard treatment, but ciprofloxacin (500mg PO single dose) is an equally accceptalbe alternative for adult pt who cannot tolerate rifampin.
Studies have demonstrated reduced steroid levels in women who use OCP concomitantly with rifampin, pt on OCPs should be placed on ciprofloxaxin instead. |
|
|
Cigarette smoking
|
Cigarette smoking causes significant physiological and psychological dependence, Withdrawal symptoms are extremely common in pt attempting to quit. Some of the common symptoms include restlessness, anxiety, irritability, frustration, decreased concentration, insomnia, or depressed mood, These generally peak in the first 3-4d after smoking cessation and usually resolve in the next 3-4w. These symptoms and the associated intense craving for cigarettes are responsible for the majority of relapses seen in pt.
Current recommendations for the management of smoking cessation involve a combination of behavioral therapy and a pharmacologic intervention such as buproprion or nicotine replacement. Nicotine replacement therapy (gum, patch or inhaler) acts by maintaining a low level of nicotine in the blood. It is preferred for the amelioration of withdrawal symptoms during the early stages of smoking cessation. |
|
|
Varenicline –stop smoking
|
The most commonly used pharmacotherapies for smoking cessation include nicotine replacement, bupropion (antidepressant) and varenicline. Varenicline is a partial agonist of the subunit of the nicotine acetylcholine receptor that controls nicotine dependence. Its side effects is suicidal ideation and erratic or bizarre behavior . It is recommended that pt who have unstable psychiatric symptoms or a h/o previous suicidal ideation avoid the drug and should be considered second-line for any pt with a h/o major depression.
|
|
|
Hereditary form of breast cancer
|
A hereditary form of breast cancer should be suspected if ther is a h/o a first degree relative with early age of breast cancer, multiple aected relatives, relatives with breast and ovarian cancer or relatives with more than one primary cancer,
Genetic testing should be done in these pt, Option or pt who are BRCA + mutation include prophylactic mastectomy and/or oophorectomy卵巢切除术, increased surveillance and chemoprevention with OCPs or selective estrogen receptor modulators(SERMs) Oral contraceptive use in BRCA1 and BRCA2 mutation carriers appears to decrease the risk of ovarian cancer. Chemoprevention using tamoxifen for five years reduces the incidence of breast cancer by approximately 50 percent in women with a moderately increased risk for breast cancer Raloxifene is slightly less effective than tamoxifen in reducing breast cancer risk, but is associated with fewer serious side effects. |
|
|
An adequate blood pressure control
|
especially systolic blood pressure, is the best measure for primary prevention of stroke. Good diabetes control, as well as smoking cessation, is also beneficial, but not as effective..
|
|
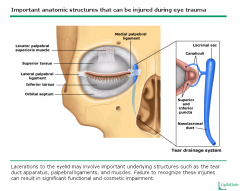
Eyelid laceration
|
Horizontal lacerations of the upper eyelid may involve the orbital septum, a structure that separates orbital content from the lid tissue. The presence of orbital fat tissue in the wound indicates a high probability o septum injury and a possible levator palpebrae injury. Levator unction should be tested by asking him to look up and down.
Canaliculi泪小管are most susceptible to medial laceration of the eyelids. tarsus 睑板 The most common pathogen isolated rom cultures of corneal foreign bodies is coagulase negative Staphylococcus. Other common pathogens include Streptococcus, Haemophilus and Pseudomonas. Pseudomonas is a common cause of bacterial infection in contact lens wearers. |
|
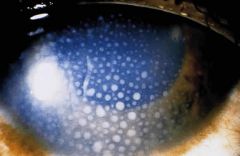
Anterior uveitis前葡萄膜炎(iritis)
|
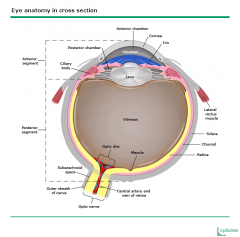
pain, redness, variable visual loss and a constricted and irregular pupil. There is no foreign body sensation per se. Patients with an active corneal process and iritis will display an aversive response when the penlight is shined in the affected and in the uninvolved eye(photophobia). The cardinal sign of iritis is ciliary flush: injection that gives the appearance of a red ring around the iris. Typically, there is no discharge and only minimal tearing. The patient may choose to keep the eyes closed to block out light but, in a dimly lit environment, the patient is able to keep the affected eye open spontaneously. To properly distinguish ititis from other causes of a red eye, it is important to visualize the anterior segment of the eye with slit lamp examination, If leukocytes (keratitic precipitates, deposits of white blood cells on the endothelium) are seen in the anterior segment, which contains the aqueous humor ound between the cornea and the lens, then the dx of iritis is confirmed. A hazy “flare”, which is indicative of protein accumulation secondary to a damaged blood-aqueous barrier may also be seen.
keratitic precipitates The uvea is the middle portion of the eye. The term derives from the Latin word for grape, since anatomists once thought that the peeling of the outside of the eye left a grape-like structure beneath. The anterior portion of the uvea includes the iris and ciliary body; the posterior portion of the uvea is known as the choroids • Inflammation of the anterior uveal tract is called anterior uveitis and is synonymous with iritis. When the adjacent ciliary body is also inflamed, the process is known as iridocyclitis . • Terms used to describe forms of uveitis posterior to the lens include vitritis, intermediate uveitis, pars planitis, choroiditis, retinitis, chorioretinitis, and retinochoroiditis. Panuveitis refers to simultaneous inflammation anterior and posterior to the lens with a component that affects the retina or choroids Uveitis may be divided into four major subsets based upon the etiology of the inflammation: • Infections: CMV, Toxoplasmosis, syphilis, TB, cat scratch diseae, West Nile, Herpes • Systemic immune-mediated disease • Syndromes confined primarily to the eye • Masquerade syndromes A genetic predisposition may contribute to the development of uveitis. Infectious causes of uveitis — Cytomegalovirus (CMV), Toxoplasmosis, Syphilis,Tuberculosis ,Cat scratch disease ,West Nile viral infection,herpes simplex and herpes zoster Systemic inflammatory diseases associated with uveitis — Uveitis can occur as a manifestation of many systemic diseases . • Spondyloarthritides (SpA), such as ankylosing spondylitis and reactive arthritis, are the most common systemic immune disorders associated with uveitis in North America and Europe. Twenty to 40 percent of patients with either of these HLA-B27-related disorders develop the sudden onset of anterior uveitis. When it occurs, uveitis is often the manifestation to suggest the diagnosis of the systemic illness. Uveitis in association with spondyloarthritis is twice as common in males as in females. In contrast to the uveitis associated with the spondyloarthropathies, uveitis associated with IBD or psoriatic arthritis is frequently bilateral, posterior to the lens, insidious in onset, chronic in duration, and more common in females than males • Sarcoidosis accounts for a significant percentage of patients with uveitis in most series from referral centers. Approximately 20 percent of patients develop eye disease as their initial presentation of sarcoid. The eye disease can take on many forms, including uveitis, dry eyes, optic neuritis, lid inflammation, or orbital disease. Uveitis in patients with sarcoid is frequently associated with retinal vasculitis, which may be either perivascular or involve retinal vascular changes . The eye disease may persist despite the resolution of adenopathy. 15-20% of pt with sarcoidosis have eye involvement, Anterior uveitis is the most common presentation among different ophthalmic manifestations of disease. • As many as 80 percent of patients with Behçet's disease develop uveitis. Uveitis is often the dominant manifestation of this disease and is typically bilateral. Similar to HLA-B27-associated iritis, it is frequently episodic, but, unlike HLA-B27-associated disease, the uveitis generally does not resolve completely between episodes. Behçet’s uveitis often presents as a panuveitis, and retinal vasculitis is a frequent manifestation of Behçet's disease. The uveitis typically leads to blindness if the eye inflammation is not treated. Masquerade syndromes — A number of noninfectious processes can be mistaken for an inflammatory process; most of these are malignancies. The most common malignancy that presents like uveitis in adults is lymphoma, typically a B cell type that is confined to the eye and the central nervous system. The eye disease is usually bilateral and generally presents as the insidious onset of visual obscuration, such as floaters. Ocular lymphoma may be difficult to diagnose, but should be suspected when inflammation is refractory to glucocorticoids, when neurological symptoms are present, or when bilateral posterior eye inflammation has begun after age 45.\ SYMPTOMS — The symptoms of uveitis depend upon the portion of the uveal tract that is involved. Anterior uveitis may produce pain and redness, although these symptoms are minimal if inflammation begins insidiously (eg, in juvenile idiopathic arthritis). The degree of visual loss associated with anterior uveitis is variable. By contrast, posterior or intermediate uveitis is more likely to be painless but may result in visual changes such as floaters or reduced visual acuity. Floaters or debris in the visual field may also result from noninflammatory processes such as normal aging. Redness of the eye is not a prominent feature of posterior inflammation unless there is an accompanying anterior uveitis. Anterior uveitis is about four times more common than posterior uveitis. Red eye — Although many patients with anterior uveitis have a red eye, this finding must be distinguished from other causes of a red eye, such as corneal inflammation (keratitis), conjunctival inflammation (conjunctivitis), blood vessel inflammation in the episclera or sclera (episcleritis and scleritis, respectively), or acute closed angle glaucoma. Iritis (anterior uveitis) can usually be distinguished by redness that is primarily noted at the limbus (the junction between the cornea and the sclera), a constricted pupil, and pain. DIAGNOSIS — Ultimately, iritis is distinguished from other causes of a red eye by slit lamp examination. This examination allows the trained observer to visualize the anterior segment of the eye. Leukocytes are not normally found in the aqueous humor that fills the space between the cornea and the lens; their presence in the anterior chamber is readily appreciated with the slit lamp and is diagnostic of anterior uveitis. A haze, described by ophthalmologists as "flare," may also be appreciated by slit lamp examination and reflects protein accumulation in the aqueous humor secondary to disruption of the blood aqueous barrier. In comparison to anterior uveitis, posterior or intermediate uveitis is diagnosed by direct visualization of active chorioretinal inflammation and/or by detection of leukocytes in the vitreous humor on ophthalmic examination. The diagnosis of panuveitis is made when inflammation is detected simultaneously in the anterior chamber, vitreous, and retina or choroid. These findings are identified either by use of a slit lamp in conjunction with special lenses to focus the beam posterior to the lens or with an indirect ophthalmoscope and a handheld lens. Complete examination of the eye posterior to the lens usually includes a technique called scleral depression. This maneuver allows the examiner to look for an inflammatory exudate over the pars plana, the portion of the eye just between the retina and the ciliary body. Exudates or "snowbanks" are characteristic of a relatively common form of intermediate uveitis known as pars planitis |
|
|
Cataracts
|
Cataracts and associated macular degeneration are extremely common in the elderly population and often result in visual impairment. Elderly pt should be thoroughly evaluated for the severity of macular degeneration, as they may not benefit from cataract surgery.
|
|
|
Orbital cellulites
|
typically arises from an extension of infection of the paranasal sinuses. It is a potentially life-threatening condition, warranting admission to the hospital and treatement with broad-spectrum iv antibiotics (cefoxitin or ampicillin-sulbactam) for 3d and oral therapy or an additional 2-3w.
|
|
|
Incisional biopsy
|
A biopsy in which only a sample of the suspicious tissue is cut into (incised) and removed for purposes of diagnosis. A incisional biopsy is in contrast to an excisional biopsy in which an entire lesion, usually a tumor, is removed.
|
|
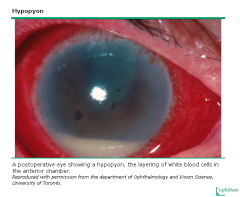
Endophthalmitis眼内炎
|
Endophthalmitis is an emergency that can be suspected in pt who p/w acute unilateral deterioration of vision and conjunctival and lid edema and erythema. PE: swollen eyelids and edema or erythema of the conjunctiva. Hypopyon, a layer of leucocytes in the anterior chamber, is frequently present. In 80% of the cases, the retinal vessels can not be seen.
Although the pt may need to be admitted to the hospital, the most immediate measure required is the intravitreal administration of antibiotics, which can only be done by a skilled ophthalmologist. Tx: Immediate management must be done by an ophthalmologist, who will confirm the dx using aspiration and vitrectomy to obtain vitreous or aqueous cultures and administer antibiotics by the intravitreal route. |
|
|
Ocular melanoma
|
An ocular melanoma is a primary malignant tumor arising from the melanocytes within the uvea, It is an infrequent tumor which is usually diagnosed during either a routine unoscopic examination or a undoscopic exam for some other disorder. It remains asymptomatic for a long time and usually p/w progressive and painless visual field abnormalities or blurring of vision., or floaters or even pain if the tumor impinges
Dx: eye U/S for diagnosis, MRI to document any extrascleral extension for staging and treatment decision Tx: surgical enucleation or radiotherapy All pigmented lesions that are suspicious for cutaneous melanoma should be completely excised or accurate diagnosis and staging. Excisional biopsy: A surgical procedure in which an entire abnormal area is removed for diagnostic examination under a microscope. |
|
Blepharospasm睑痉挛
|
A form of focal dystonia (Dystonia is a movement disorder characterized by involuntary, sustained muscle contractions that result in twisting and repetitive movements or abnormal postures). Periodic involuntary eye closure that can be provoked by external stimuli (bright light or irritants like smoking) and increased blinking is typical. Older women are particulary predisposed to this condition (dry eyes in postmenopausal women may serve as a trigger for blepharospasm.)
Botulinum toxin injections are the mainstay of treatment |
|
Toxic shock syndrome 外毒素
Septic shock 内毒素 |
|
|
|
Toxic shock syndrome 外毒素
Septic shock 内毒素 |
|
|
|
HIV postexposure prophylaxis
|
Occupational transmission of HIV due to blood and certain body fluids (semen, vaginal secretions and any other body luid containing visible blood, CS, pleural, pericardial, synovial luid)
Standard precautions do NOT apply to urine, sweat, tears, sputum, vomitus and nasal secretions or feces as long as there is no gross visible blood. Contact with saliva, tears or human sweat has never been shown to cause transmission of HIV. Numerous reports literature about human bites show that HIV has never been transmitted in this manner. Human bite---no HIV transmission The rate o transmission of HIV is < 1% in cases where the source pt is known to be HIV+. Post-exposure prophylaxis is recommended for all healthcare workers who have had a percutaneous or mucous membrane exposure to HIV-infected bodily fluids. Two nucleoside reversse transcriptase inhibitors for 4w is the usually regimen (The source pt has an asymptomatic infection or low viral load), with the addition of a protease inhibitor in cases where the source pt has a high viral load. Prophylaxis should ideally be started within 2h of the exposure. |
|
|
HIV- candida endophthalmitis
|
Oropharyngeal and esophageal candidiasis arises commonly in HIV+ pt and can disseminate widely to multiple organs, including the eye (hematogenous seeding )
The presenceof candida endophthalmintis is a marker for widespread disseminated candidiasis and should not be taken lightly. It is frequently characterized by ocular pain. Photophobia. Scotomas and fever. Risk factors that place pt at greatest risk for developing candida endophthalmitis include: central venous catheters, total parenteral nutrition, broad-spectrum antibiotic therapy, prior abdominal surgery, neutropenia, corticosteroid therapy and injection durg abuse. Tx: Patient with candida endophthalmitis who have chorioretinitis with vitreal involvement should be treated with vitrectomy and systemic amphotericin B and/or fluconazole. An early vitrectomy improves the likelihood of a positive outcome, and iv intravitreal injection of amphotericin B may be of help. Prompt dx and treatment is essential as the condition can worsen quickly. |
|
|
HIV – thrombocytopenia
|
Primary HIV associated thrombocytopenia (PHAT) affects 40% of HIV+ pt at some point. From a clinical standpoint. PHAT is highly similar to ITP. Up to 20% of pt with PHAT will experience a spontaneous remission. However most will require some intervention.
The mainstay of therapy for PHAT is zidovudine, which also reduce the occurrence of opportunistic infection and Kaposi’s sarcoma. Even though it has potential for suppression of myeloid and erythroid precursors, AZT increase platelet production in HIV pt. Experts recommend the inclusion of zidovudine at a minimum does of 600mg/day in a multiagent antiretroviral regimen. If the thrombocytopenia does not begin to resolve within 4-8w of therapy, the zidovudine dosage can be increased to 1000-1500 mg/day. Clostridum dificile-associated colitis It can take several forms, ranging from mild self-limited diarrhea to life-threatening fulminant colitis., abdominal distension, diffuse abdominal tenderness, fever and grossly bloody stool. Limited endoscopy of unprepared bowel with minimal air inflation is a good diagnostic option in severely ill patients with suspected Clostridium dificile-associated colitis. Although stool cytotoxin test for C. dificile toxin may seem the most appropriate test, endoscopy is sometimes more useful in severely ill pt because it can be done quickly. The high-risk antibiotics include clindamycin, ampicillin, amoxicillin and cephalosporins. Clindamycin is believed to have the highest probability of provoking C. dificile infection. Tx: metronidazole, vancomycin |
|
|
Diabetic patients with infected pedal ulcers –osteomyellitis?
|
Probing to bone — Probing for bone should be included in the initial assessment of all diabetic patients with infected pedal ulcers, since palpating bone on probing the pedal ulcer is sufficient for diagnosis of osteomyelitis. This was illustrated in a prospective study of 76 cases of infected foot ulcers; palpating bone on probing the pedal ulcer had a sensitivity, specificity, positive predictive value and negative predictive value of 66, 85, 89 and 56 percent, respectively. If bone is palpated on probing, specialized roentgenographic and radionuclide tests to diagnose osteomyelitis are not necessary.
While diagnosing osteomyelitis is important, it is unfortunately also difficult. Clinical and laboratory signs and symptoms are generally unhelpful . Bone infection may not show up on plain radiographs in the first 2 weeks, and any X-ray abnormalities detected may be caused by the neuropathic bone disorders that frequently occur in diabetes. More accurate imaging studies, such as radionuclide scans or magnetic resonance imaging, are expensive and not universally available . In 1995, Grayson et al. described a clinical technique they used in diabetic patients with a foot infection consisting of exploring the wound for palpable bone with a sterile blunt metal probe. Their most important finding was that the probe-to-bone (PTB) test had a positive predictive value of 89%, leading them to conclude that a positive test usually made imaging studies for diagnosing osteomyelitis unnecessary. Since then, many have considered a positive PTB sufficient evidence for osteomyelitis Dx: X-ray: periosteal reaction and osseous lucency probe-to-bone, REACH THE BONE MRI Culture of deep tissue obtained by curettage |
|
|
Herpes zoster
|
Disseminated herpes zoster :more than twenty skin lesions outside the primary or adjacent dermatomes; other organs, such as the liver or brain may also be affected (causing hepatitis or encephalitis respectively), and the condition may be life-threatening.
Herpes zoster is also considered infectious, although the risk of transmission is not as high as that of varicella. According to the current recommendations, all pt with disseminated herpes zoster should be maintained on contact and airborne recommendations, all pt with disseminated herpes zoster should be maintained on contact and airborne isolation until all skin lesions are dry and crusted. Contact precautions are indicated in hospitalized pt with localized herpes zoster, but there are not currently recommended in a community setting. |
|
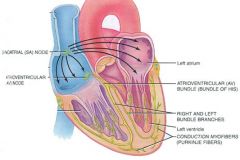
Aortic valve endocarditis
|
can cause conduction syetem abnormalities because of its close proximity to the proximal ventricular conduction system, Perivalvular abscess should be suspected in that case.
|
|
|
Invasive aspergillosis
|
Invasive aspergillosis is common in BMT recipients. It typically involves the respiratory tract, including the lungs and the sinuses (localized headache, nasal bleeding).
|
|

Transverse myelitis
|
Transverse myelitis (TM) is a segmental spinal cord injury caused by acute inflammation. It typically follows an URI that can be mild and is characterized by rapidly progressive paraplegia, sensory loss and pelvic organ dysfunction. Dull back pain may also be present. In pt with acute and subacute myelopathy, compressive lesions, like an epidural abscess, tumore and herniated intervertebral disk should be immediately ruled out,
Most cases of TM are idiopathic and presumably result from an autoimmune process. up to half of these patients have a preceding infection. TM is also associated with connective tissue diseases, including: • Systemic lupus erythematosus • Mixed connective tissue disease • Sjogren's syndrome • Scleroderma • Antiphospholipid antibody syndrome • Ankylosing spondylitis • Rheumatoid arthritis The initial evaluation should include an immediate MRI. MRI of the involved section of the spinal cord shows gadolinium-enhancing signal abnormality, usually extending over one or more cord segments DD: Guillain Barre syndrome In the pt, sensory level and early loss o bowel and bladder function point toward myelopathy rather than GB syndrome |
|
|
Recurrent UTI
|
Antibiotic prophylaxis can be considered in young female pt who have had >2 UTIs in 6m or >3 UTI in a year. Prophylaxis can either be 6-12m or solely postcoital. Fluoroquinolines, sulfamethoxazole-trimethoprim and nitrourantoin are the most commonly used agents. An additional option is providing femiale pt with antibiotics in advance and allow the pt to self-diagnose and treat her UTI. Further diagnostic evaluation in these pt is typically unrevealing unless there is clinical evidence to suggest the presence of nephrolithiasis or obstruction. Additional measures include voiding after intercourse and drinking large amounts of water to augmentdiuresis.
Differentiating a relapse from a recurrent UTI may be difficult. Recurrent: the infecting organism is different from that of the original infection or An infection with the same organism occurs after 2w of completion of treatment Relapse: An infection with the same organism occurs within 2w of completion of treatment. A urinalysis and a urine culture are extremely important in such cases. Urine culture before and after antibiotic treatment is important in pt with recurrent UTIs. One should ensure that the urine culture is negative before starting prophylactic antibiotics to prevent recurrent UTI and the urine culture is negative after the initial treatment is completed. Prophylaxis for recurrent UTI should not be undertaken until a negative culture 1-2w after treatment has confirmed eradication of the UTI. |
|
|
HIV-syphilis
|
HIV-infected pt with late latent syphilis or latent syphilis of unknown duration should have a CSF examination before treatment even if pt is asymptomatic, Pt with normal CSF analysis should receive benzathine penicillin G IM for 3w.
HIV pt with neurosyphilis (symptomatic or asymptomatic) and syphilitic ocular diseae are usually treated with aqueous crystalline penicillin G IV for 2w. HIV infected pt with early syphilis or early latent syphilis <1y duration should receive benzathine长效 penicillin G IM in a single dose. • HIV-infected patients with primary, secondary, or early latent syphilis should receive benzathine penicillin G (2.4 million units IM) in a single dose . • Patients with late latent syphilis, or the more common latent syphilis of unknown duration, should receive benzathine penicillin G (2.4 million units IM) weekly for three consecutive weeks. • Neurosyphilis should be treated with aqueous crystalline penicillin G (3 to 4 million units IV every four hours or as a continuous infusion for a total daily dose of 18 to 24 million units) for 14 day。 An additional dose of IM benzathine penicillin (2.4 million units) may be considered at the end of the treatment course to complete three weeks of therapy for late disease. Jarish-Herxheimer reaction: acute febrile reaction that develops within 24h after the initiation of any treatment for syphilis is commonly referred to as Jarisch-Herxheimer reaction. Fever is usually accompanied with malaise, chills, headache and myalgias. It may be due to an immunological reaction to the rupture of spirochetes. HIV coinfection is not accompanied by a more severe reaction or increase in the incidence of the reaction. No effective prevention is available. |
|
|
HIV-esophagitis
|
Failure to respond to anti-fungal drugs indicates some cause other than candidiasis. The patient with odynophagia who does not respond to a trial of antifungal therapy should undergo upper endoscopic evaluation, An exception is the patient with evidence of oral or labial HSV, for whom an empiric trial of oral acyclovir is also reasonable.
Giant ulcers with no virus found on biopsy suggest aphthous ulcers口疮, which is treated with prednisone. CMV esophagitis are characterized by one or more deep ulcerations, usually in the distal third of the esophagus. These ulcers are typically oblong, with a sharply demarcated, "punched-out" appearance, and a bland base. HSV esophagitis more widespread involvement, its typically shallow, erosive injury (similar to the appearance of erosive reflux esophagitis), and its more abrupt onset. HSV can cause intensely painful swallowing and frank ulceration and, unlike CMV, is often associated with labial or oral cavity lesions, which are important clues to esophageal involvemen |
|
|
Indinavir-HIV
|
Crystal-induced nephropathy is a well-known side effect of indinavir therapy (protease inhibitor for HIV tx). It is caused by the precipitation of the drug in the urine and obstruction of the urine flow.
The common acute life-threatening reactions associated with HIV therapy include: Dianosine-induced pancreatitis Abacavir-related hypersensitivity syndrome Lactic acidosis secondary to the use of any of the NRTIs Stevens-Jonhson syndrome secondary to the use of any of the NNRTIs Nevirapine-associated liver failure In a treatment-naïve HIV+ pt, HAART should decrease the viral load to <50 copies/mL within 6m. |
|
|
Systemic sclerosis – macrocytic anemia
|
Bacterial overgrowth should be suspected as a cause of VitB12 deficiency in pt with intestinal stasis secondary to anatomic abnormalities such as surgically created blind loops, abnormal small bowel motility and fistulas between the proximal and distal GI tract. Use of proton pump inhibitors can be a precipitating factor. Jejunal aspirate is the gold standard dx test. (intrinsic factor protects the vitamin from catabolism by intestinal bacteria.)
|
|
|
Chronic prostatis
|
First-line drug: quinolones preferably ciprofloxacin or levofloxacin
Second-line: TMP-SMX Therapy must be given for 6-12w. UTI First line: quinolone |
|
|
HIV(+) pt not already on HAART
|
should have their CD4 count and viral load measured every 3-4m.
|
|
|
HIV lipodystrophy – Nucleoside reverse transcriptase inhibitor
|
HIV lipodystrophy p/w lipoatrophy, fat accumulation or both in different areas (cushingoid pattern). A pattern with increased fat tissue deposition on the back of the neck and abdomen along with extremities and face is suggestive of HIV lipodystrophy. Insulin resistance and dyslipidemia are closely interrelated with HIV lipodystrophy.
Tx: if triglyceride > 500 mg/dL, gemfibrozil If triglyceride < 500 mg/dL, statin |
|
|
Salmonellosis
|
does not need to be treated with antibiotics in immunocompetent individuals age 12m or older.
Tx: Replacement fluid and electrolytes as they are at risk for becoming dehydrated. Supportive therapy and observation |
|
|
Ampicillin-associated rash in pt with infectious mononucleosis
|
is immune-mediated and is caused by circulating IgG and IgM antibodies toward penicillin derivatives. Such antibodies have actually been demonstrated in pt with EBV-associated infectious mononucleosis.
|
|
|
Oral candidiasis (thrush)
|
These plaques can typically be removed and a residual area of inflammation seen where the plaque has been removed. Most are asymptomatic, although some may c/o a strange, cottony taste in the mouth. The pt should be observed for proper use of his inhaler as the thrush may be a sign that he is using it improperly with a large amount of the medicine depositing in his oropharynx as opposed to passing into his lungs. Candia can also cause esophagitis (odynophagia) if the infection progresses. It is very unusual for a young and otherwise healthy adult, especially when there is also an accompanying lymphoadenopathy. In such a setting, an underlying immunodeficiency should be suspected. HIV testing should be tested.
The best initial therapy for oral candidiasis (thrush) is a topical antifungal (nystatin suspension or clotrimazole troches,) with an oral antiungal such as fluconazole used for resistant cases. Pt should be advised to rinse their mouth after using inhaler. |
|
Necrotizing fasciitis
|

Necrotizing fasciitis is a fulminant infection of the subcutaneous tissue that spreads along the fascial planes and extensive tissue necrosis and destruction.
Type I: pt with underlying DM and peripheral vascular disease, by a mixture of aerobic and anaerobic microorganisms’ Type II: pt with NO concurrent medical illness, h/o laceration, blunt trauma, surgical procedure or long h/o iv durg use as a predisposing factor. It is typically caused by group A streptococci (strep pyogenes). Severe pain in the absence of significant skin changes is the inital presentation. The infection spreads rapidly along the fascial plane with erythema, blister and bullae formation, fever, malaise, systemic toxicity and shock, developing in a rapid sequence. In some cases, the infection can lead to extensive tissue necrosis and destruction with minimal skin changes. Tx: A clinical suspicion of necrotizing fasciiitis warrants urgent, aggressive surgical exploration and debridement of the involved tissue to prevent morbidity and mortality. Clindamycin or penicillin is the drug of choice for the treatment of necrotizing fasciitis/myonecrosis due to Group A strep. ** group A streptococci is the typical etiologic agent of erysipelas (red, painful, edematous and elevated, a sharp demarcation rom the uninvolved skin, see below picture) |
|

MELD scoring system
|
The most commonly used calculation to predict mortality in pt with liver disease (90 day survival) is the Model for End-Stage Liver Disease (MELD) scoring system.
Bilirubin INR Serum creatinine MELD has largely replaced the Child-Turcotte-Pugh scoring system since it relies only on objective variables and is applicable along a broad continuum of disease. 95% survival – score of <15 65% survival – score of 30 10-15% survival --- score of 40 The MELD scoring system is used to select pt for placement of a transjugular intrahepatic portosystemic shunt (TIPS), with pt that have a score of <14 having the best outcome and with the procedure being avoided in pt with a score >24. The MELD scoring system is also used to calculate a pt’s priority on the liver transplant list, with pt that have a higher MELD score taking precedence should a suitable donor liver become available. |
|
Immune reconstitution inflammatory syndrome
|
Immune reconstitution inflammatory syndrome (IRIS) is a paradoxical worsening of preexisting (and sometimes subclinical) infection in HIV+ individuals. The syndrome usually occurs days to weeks after the initiation of treatment with highly active antiretroviral therapy and is thought to arise secondary to the rapid improvement in immune unction allowed or by HAART. The inflammatory reactions that develop at the sites of preexisting infection are responsible or the worsening of the pt’s clinical presentation. Occational this can cause severe long-term sequelae, especially if neurologic tissues are involved.
Tx: IRIS is self-limited and is best managed with continued HAART and antibiotic treatment of the underlying pathogen. |
|
Community-acquired pneumonia and influenza
|
Community-acquired pneumonia and influenza together is one of the leading causes of death in the US, It is important to appropriately triage these pt into low, intermediate and high risk of short-term morbidity and mortality,
|
|
|
Erythyma gangrenosum
|
It is associated with lesions of the skin or mucous that rapidly worsen and evove into nodular patches marked by hemorrhage, ulceration and necrosis.
Pseudomonas aeruginosa bacteremia is usually treated with a two-drug regimen to limit the emeregence of antibiotic resistance. Such regimen typically include an amnioglycoside (tobramycin or amikacin) and an extended –sepctrum antipseudomonal penicillin (piperacillin) or antipseudomonal cephalosporin (cefazidime头孢他定 or cefepime头孢吡肟). Surgical debridement is not indicated in the treatment of ecthyma gangrenosum. |
|
|
Catheter related infections
|
Catheter removal is recommended in catheter related infections where there is hemodynamic instability, severe sepsis with organ hypotension, endocarditis, suppurative trombophlebitis or persistent bacteremia after 72h of appropriate antibiotic therapy. Vancomycin is used for empiric antibiotic treatment with the addition of gram negative coverage if the pt is neutropeni or septic.
|
|
|
Pentamidine
|
Pentamidine iv therapy is associated with a number of metabolic and electrolyte disturbances including hyperkalemia, hypokalemia, hypocalcemia, hyperglycemia and hypoglycemia. Their incidence may reach 70% of treated pt. Hypoglycemia should be promptly detected by performing a finger stick blood glucose level test in the pt
|
|
|
Lyme disease
|
Tx: iv ceftriaxone if there is early disseminated disease consisting of carditis or neurological symptoms beyond carnial nerve palsy.
Oral doxycycline, amoxicillin or ceuroxime for localized Lyme disease. |
|
|
Diphtheria antitoxin
|
Diphtheria antitoxin is made with horse serum, thus the risk of hypersensitivity or serum sickness is approximately 10%. There is also a lesser risk of anaphylaxis.
|
|
|
Current level of immunosuppression
|
CD4 lymphocye count is an indicator of the current level of immunosuppression and is CD4 count referred to by some authors as “the immunologic damage that has already occured”
Viral laod is a good marker of disease activity or the potential for future damage to the immune system. It is referred to as “the damage that is about to occur”. |
|
Streptococcal pharyngitis
|
Dx: > 3 of the following has a roughly 50% positive predictive value for streptococcal pharyngitis, but there is an 80% negative predictive value for streptococcal pharyngitis
1. Tonsillar exudates 2. tender anterior cervical lymphadenopathy 3. Fever 4. absence of cough |
|

Pearly penile papules阴茎珍珠状丘疹
|
Pearly penile papules are a normal variant and are not spread by sexual contacts or activity. These asymptomatic papues are more common in uncircumcised males and typically appear as one or multiple rows of small, flesh-colored, dome-topped or filiform papules positioned circumferentially around the corona of sulcus of the gland penis. Tx is not necessary.
|
|

Cutaneous cryptococcosis
|
An early manifestation of disseminated cryptococcosis in pt with HIV disease. It manifests as multiple, discrete, reddish colored papules with central umbilication.
Dx: histopathologic examination of the biopsy specimen from the skin lesions is necessary to confirm the dx of cutaneous cryptococcosis: a granulomatous inflammatory reaction with multinucleatd giant cells, histiocytes, lymphocytes, neutrophils and plasma cells with numerous yeast-like organisms present both in the free spaces and within the histiocytes and giant cells. Special stains such as Periodic Acid Schiff and Gomori’s methenamine silver nitrate are commonly emplyed to identify the organism in the biopsy specimen. |
|
|
Multiple medications – elderly-adverse durg reaction
|
Multiple medications are the most common factor in predisposing elderly pt to an increased incidence of adverse drug reaction. Pt > 65y take an average of 2-6 prescribed durgs and 1-3 non-prescription drugs daily. These pt are at an increased risk preoperatively for anesthetic and operative drug reactions. The most common medications associated with adverse drug reactions include anti-psychotics, anti-hypertensives, sedatives, diuretics, NSAIDS, corticosteroids and digoxin.
|
|

Ischemic stroke
|

Pt with acute ischemic stroke and CT scan of the head negative for hemorrhage who are treated with tissue plasminogen activator< 4.5h (optimally within the first 3h after the onset of neurologic symptoms) should not receive antiplatelet therapy, anticoagulation or invasive testing during the first 24h after treatment. Frequent neurologic checks, no invasive testing or procedures. Strict control with iv medications, such as labetalol, nitroprusside or nicardipine is recommended to keep BP at 180/105 mmHg.
Aspirin can be started after 24-48h if pt is stable. Clopidogrel is a more effective antiplatelet agent than aspirin and should be substituted in pt who have had a cerebrovascular event and aspirin failure. It is important to maximize control of modifiable vacular risk factors (DM, hyperlipidemia, smoking, HTN) in order to give the chosen antiplaetlet agent the best chance of reducing the risk of future cerebrovascular events. |
|
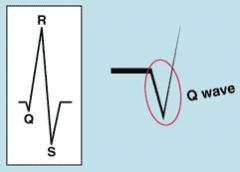
Pathologic Q waves
|
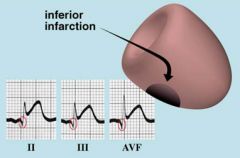
The Q wave is the first downward wave of the QRS complex, and it is followed by an upward R wave
Pathologic Q waves are a sign of previous myocardial infarction. They are the result of absence of electrical activity. A myocardial infarction can be thought of as an elecrical 'hole' as scar tissue is electrically dead and therefore results in pathologic Q waves. Pathologic Q waves are not an early sign of myocardial infarction, but generally take several hours to days to develop. Once pathologic Q waves have developed they rarely go away. However, if the myocardial infarction is reperfused early (e.g. as a result of percutaneous coronary intervention) stunned myocardial tissue can recover and pathologic Q waves disappear. In all other situations they usually persist indefinitely. The precise criteria for pathologic Q waves have been debated. Here we present the latest definition as accepted by the ESC and ACC. Definition of a pathologic Q wave Any Q-wave in leads V2–V3 ≥ 0.02 s or QS complex in leads V2 and V3 Q-wave ≥ 0.03 s and > 0.1 mV deep or QS complex in leads I, II, aVL, aVF, or V4–V6 in any two leads of a contiguous lead grouping (I, aVL,V6; V4–V6; II, III, and aVF) R-wave ≥ 0.04 s in V1–V2 and R/S ≥ 1 with a concordant positive T-wave in the absence of a conduction defect Notes • Absence of pathologic Q waves does not exclude a myocardial infarction! • Lead III often shows Q waves, which are not pathologic as long as Q waves are absent in leads II and aVF (the contiguous leads) |
|
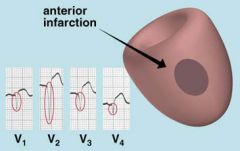
Pathologic Q waves
|
Pathologic Q waves
|
|
Pathologic Q waves
|
Pathologic Q waves
|
|
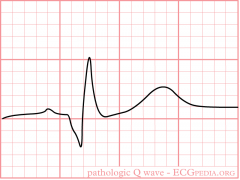
Pathologic Q waves
|

Pathologic Q waves
|
|
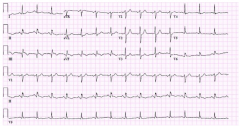
Pathologic Q waves
|
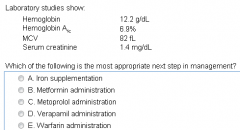
|
|
Pathologic Q waves
|

Pathologic Q waves
|
|

Pathologic Q waves
|
Pathologic Q waves
|
|

Abdominal gunshot wounds
|
Abdominal gunshot wounds can cause significant injury, most commonly to the small bowel, colon and liver. Pt should first be completely undressed to evaluate for Abdominal wounds, entry and exit points and wounds in other parts of the body.
Pt who are hemodynamically unstable, have evidence of peritonitis or have evisceration of any organs need immediate exploratory laparotomy. Pt without any of the above may be evaluated with plain films which can show the bullet if there is no exit wound. |
|
Abdominal gunshot wounds
|
Abdominal gunshot wounds.
|
|
|
PSA – prostate cancer
|
Elevated PSA can result from benign prostate hyperplasia, prostate cancer, prostate inflammation or infection and perineal trauma.
Men with an either abnormal digital rectal examination (showing prostate nodules or asymmetry) or elevated PSA level (4-10 ng/mL) should be referred for transrectal unltrasound-guided prostate biopsy (TRUS). Some guidelines recommended that men with PSA levels of 2.5-4 ng/mL have repeat testing several weeks or months later to monitor the trend. If the repeated PSA is elevated, then the pt should be referred for consideration of TRUS. The positive predictive value of an elevated PSA level of 4-10 ng/mL is almost 25% and increases dramatically as the PSA level rise > 10 ng/mL. |
|
Organ transplantation from cadaveric donors
|
** The primary goal of medical management of a brain dead organ donor is t maintain a euvolemic, normotensive and normathermic state.
|
|
Organ transplantation from cadaveric donors
|
Organ transplantation from cadaveric donors
|
|
|
Organ transplantation from cadaveric donors
|
Organ transplantation from cadaveric donors
|
|
|
Mood disorders /troubled home lift ---Transplantation
|
Mood disorders and a toubled home life in possible transplant recipients are major issues that may predispose pt to poor outcomes after surgery. Mood disorders, however, are potentially treatable psychiatric conditions and their mere presence does not prevent a potential candidat from heart transplantation. These problems must be considered along with the resit of the information available when contemplating a pt’s suitability for organ transplantation.
|
|

Brain death
|

It is not unusual to see purely spinal reflexes manifesting as isolated limb movements in a brain dead person.
|
|
|
Brain death
|
The dx of brain death can usually be made clinically at the bed side.
Clinical setting: There are a number of prerequisites before one can begin considering a pt “brain dead” 1. Clinical or neuroimaging evidence of an acute CNS catastrophe that is compatible with the clinical diagnosis of brain death, ie, the cause of brain death should be known. 2. Exclusion of complicating medical conditions that may confound clinical assessment (no severe electrolyte, acid-base, endocrine or circulatory like shock disturbance) 3. No drug intoxication or poisoning, which may confound the clinical assessment 4. Core temperature > 36’C. Hypothermia may also confound the dx assessment of brain death and can also delay the increase in PaCO2 necessary to complete the apnea test. A warming blanket is required to achieve normothermia in many pt with brain death. There is little evidence base for a choice of threshold temperature. 5. Normal systolic BP >100 mgHg. Vasopressors may be required. Neurologic examination — The examination must demonstrate absent cerebral or brainstem function with all of the following findings: • Coma • Absent brain-originating motor response, including response to pain stimulus above the neck or other brain-originating movements, eg, seizures, decerebrate or decorticate posturing. • Absent pupillary light reflex; pupils are midposition or dilated (4 to 9 mm) • Absent corneal reflexes • Absent oculovestibular reflexes (caloric responses) • Absent jaw jerk • Absent gag, sucking, or rooting reflex • Absent cough with tracheal suctioning • Absent sucking or rooting reflexes • Apnea as demonstrated by apnea test, described below However reflexes and movements which require only functioning of the spinal cord and peripheral nerves may occur in pt with brain death: flexion of the toes with foot percussion, flexion at the hip, knee and/or ankle with foot stimulation (i.e. triple flexion response), superficial abdominal reflexes. Apnea test — The apnea test is performed after all other criteria for brain death have been met. Core temperature ≥36ºC or 97ºF, systolic blood pressure ≥100 mmHg, eucapnia (PaCO2 35 to 45 mmHg), absence of hypoxia, and euvolemic status are prerequisites. The test is not valid in patients who chronically have high PaCO2 values (CO2 retainers) and in cases of neuromuscular paralysis or high cervical spinal cord lesions. In a positive apnea test there is no respiratory response to a PaCO2 >60 mmHg or 20 mmHg greater than baseline values and a final arterial pH of <7.28. Observation period — The length of observation required to determine brain death varies extensively. A follow-up evaluation after 24 hours was an early requirement for brain death diagnosis in the United States. Later, requirements in this regard were made age dependent: a 48-hour evaluation interval for infants age seven days to two months, 24 hours for those greater than two months to one year, and 12 hours for those between 1 and 18 years. An observation period for adults is considered optional (6-24h); six hours is often recommended with longer periods, up to 24 hours, recommended in cases of hypoxic ischemic encephalopathy |
|
Translator in hospitals
|
If multiple physicians are responsible for a pt’s medical care, it is crucial that they communicate regularly about key treatment objectives and preferred means of accomplishing those objectives. so that family members are provided with a clear and cohesive picture of the medical team’s assessment and plan. If such communication is absent, family members are left feeling that care is being provided in a haphazard or ineffective fashion.
|
|
Translator in hospitals
|
Translator in hospitals
|
|

Translator in hospitals
|

Translator in hospitals
|
|
Genetic test --- confidentiality
|
|
|

Herbs
|
saw palmetto美洲蒲葵--- benign prostatic hyperplasia, side effect: HTN
Kava卡瓦药(一种利尿剂)----- anxiety and insomnia, its concomitant use with alcohol, benzodiazepines or other prescription sedatives can potentiate their effect and cause excessive drowsiness or disorientation Galic --- hypercholesterolemia St John’s wort ----- depression, P450 inducer Licorice欧亚甘草 –aldosterone-like effect, aggravate HTN, contraindicated in pt with HTN Black cohosh总状升麻---- premenstrual syndrome and menopausal symptoms, excessive use can cause hypotension, use with caution in pt already on antihypertensive medications Contraindicated in pregnancy due to uterine contraction Horse chestnut ---- venous insufficiency or chronic venous stasis, can cause bleeding in pt already on aspirin or warfarin Ginkgo--- antioxidant, mild memory loss, dementia, macular degeneration and peripheral vascular disease, can interact with aspirin or warfarin leading to spontaneous bleeding Feverfew ---- migraine headache |
|
|
|
|
|
|
|
|
Withdraw patients
|
All physicians have a moral obligation to provide continuity of care for their pt. It is not appropriate to withdraw or discontinue pt care in the middle of a hospitalization or during an acute ongoing medical treatment. All physicians have the option to choose who they want to serve, however once they are involved in a case, they should not neglect the pt. If a physican wishes to withdraw from a case, he can do so if he provides the pt or the caregivers a notice long in advance so as to sufficiently permit the transfer of medical care to another physican. In the vignette, the gastroenterologist is already involved with the pt’s care since he has already performed the procedure. He can opt to withdraw from the pt’s care only if there is another gastroenterologist willing to assume pt care responsibility.
|
|
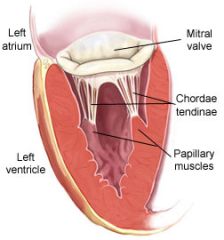
Acute heart failure
|

The 4 most common cause of acute heart failure are papillary muscle rupture, infective endocarditis, rupture of chordae tendineae and chest wall trauma with compromise of the valvular apparatus. The most common cause of isolated, severe acute mitral regurgitation in adults is rupture of chordae tendineae with or without associated myxomatous disease. The Dx is confirmed by echocardiography.
Spontaneous papillary muscle rupture usually presents in elderly people who have acute chest pain or as a complication of myocardial infarction. Mitral regurgitation: systolic murmur at the cardiac apex, the murmur decreases with Valsalva maneuver and increase with the grip maneuver, radiating to the axilla. Maran or Ehlers-Danlos syndrome (EDS) must be suspected in pt with connective tissue abnormalities and an acute MR secondary to chordae tendineae rupture, although a primary, pre-existing mitral valve prolapse is the most common cause. EDS can cause a myxomatous degeneration of the mitral valve, leading to acute rupture of chordae tendineae. Pes planus扁平足and scoliosis脊柱侧凸are frequent, though no specific findings. The skin can be velvety or thin and is usually covered with multiple characteristic “cigarette-paper” scars, due to its frailty and easy bruisability. A past h/o hernias and MVP is common. Joint hypermobility and skin hyperextensibility (rubber man syndrome) can be dramatic in severe cases. cigarette-paper” scars in EDS,s Marfan syndrome: degeneration of the mitral and aortic valves. The presentation is usually chronic, progressive mitral regurgitation and rarely acute regurgitation due to ruptured chordae tendineae. |
|
Atiral fibrillation
|

No p wave, irregulary irregular rhythm, AF with rapid ventricular response.
Pt who are hemodynamically unstable should receive urgent cardioversion. The initial step in managing AF in a hemodynamically stable pt is rate control with a beta-blocker or non-dihydropridine CCB (verapamil) or digoxin. Pt will often spontaneously convert back to sinus rhythm after treatment with b-blocker.Anticoagulation is other key component of AF management, assuming the pt does not quicky spontaneously convert back to normal sinus rhythm. CHADS2 scoring system is used to help determine a pt’s risk of stroke and whether anticoagulation requires wararin or if aspirin is sufficient. One point is given for a h/o congestive heart failure, HTN, DM or age>75 and 2 points are given if the pt has had a prior ischemic stroke or transient ischemic attack. Pt with CHADS2 score of 0 can be treated with aspirin and those with a score of >=3 should be treated with warfarin. Atiral fibrillation with a high ventricular rate must be managed with CCB (diltiazem) or beta-blockers (esmolol, metoprolol, propranolol). Rate control is achieved with diltiazem, metoprolol or esmolol 5min after administration. On the contrary, it takes 5.5h for digoxin to have a significant effect in rate control. CCB is first choice for AF pt with asthma. Amiodarone is the recommended first line antiarrhyhmic drug to maintain normal sinus rhythm in pt with paroxyxmal atrial fibrillation and structural heart disease. **Amiodarone slows metabolism of warfarin by the liver and lead to supratherapeutic INR levels, the dose of warfarin should be decreased by 25% when amiodarone is introduced and the INR should be closely followed until it has reached a new stable level. Other medications that increase the effect of warfarin include cephalosporin, ciprofloxacin, erythromycin and fluconzole. Amiodarone increased effect of warfarin and digoxin ** Amiodarone: pulmonary toxicity is the most serious adverse effect that is responsible for most of the deaths associated with amiodarone therapy. Chronic interstial pneumonitis (most common, nonproductive cough, fever pleuritic chest pain, weight loss, dyspnea on exertion and a focal or diffuse interstitial opacity on CXR), organizing pneumonia, ARDS, rarely with a solitary pulmonary mass. It is usually seen after months to years of amiodarone therapy, especially in pt who are on higher maintenance doses. It is a cumulative dose effect, and the serum amiodarone levels are usually within the normal range in these pt. |
|
|
Metformin
|
Metformin use is contraindicated in pt with renal failure, sepsis, hepartic dysfunction and severe heart failure. It should also be stopped in pt who are at risk to develop renal failure, such as those who will undergo angiography, a procedure that involves infusion of a high load of contrast agents.
|
|
|
Multifocal atrial tachycardia (MAT)
|
Multifocal atrial tachycardia (MAT) is a tachyarrhthmia that arises in pt with hypoxia, COPD, hypomagnesemia, hypokalemia, heart disease or individuals who are taking aminophylline, theophylline isoproterenol. It is characterized by the presenc of narrow QRS complexes, P waves of >3 different morphologies and variable PR segments and R-R intervals. The HR can reach up to 200/min
Tx: correct the underlying cause, if not effective, use beta-blocers. In pt with COPD, verapamil is the drug of choice. |
|
|
Digoxin toxicity
|
N/V, anorexia, fatigue, confusion, visual disturbance, cardiac abnormalities
Verapamil inhibit the reneal tubular secretion of digoxin---digoxin toxicity Medications that cause digoxin toxicity: verapamil, quinidine, amiodarone, spironolactone |
|

Left bundle branch block
|
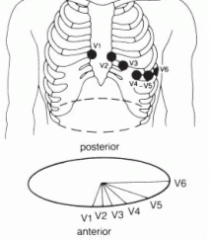
I, avL, V5, V6: a marked prolongation in the rise of those tall R waves, which will either be broad on top or notched. ( normal I, avL , V5, V6 has already tall R wave)
normal ECG A new left bundle branch block on an ECG in pt with acute chest pain is suggestive of possible MI and should be managed aggressively with coronary angiography and medical therapy. |
|
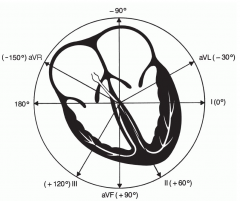
Left bundle branch block
|
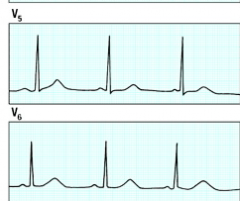
|
|
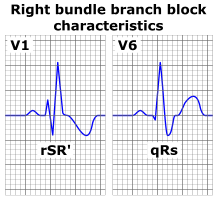
Right bundle branch block
|
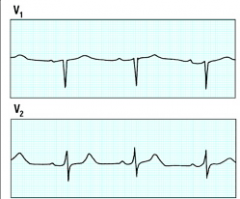
QRS > 0.12 sec,
RSR’-rabit ear (second R wave) in V1,V2 (normal QRS in V1,V2 consists of a small positive R wave and a deep negative S, reflecting the electrical dominance of the left ventricle) Carotid dissection A unilateral headache with associated Horner’s syndrome (miosis, ptosis and anhidrosis) is generally a carotid dissection until proven otherwise and MRA is the initial diagnostic modality of choice. The sympathetic chain providing innervation to the head traves on the carotid artery. Carotid dissection can be due to trauma, connective tissue disease, smoking , neck manipulation, HYN and three point restraint seatbelts in motor vehicle accidents. These pt are at a high risk for developing cerebral infarction. Tx: anticoagulation with platelet agents and/or heparin. |
|
|
Structural heart disease --- nonsustained ventricular tachycardia
|
Structural heart disease is the most common cause of nonsustained monomorphic ventricular tachycardia (HR > 120/min , last < 30 sec) and should be ruled out before searching for other causes. Some structural abnormalities that can lead to nonsustained ventricular tachycardia include scarred MI, ventricular hypertrophy, dilated left ventricle (dilated cardiomyopathy), and valvular abnormalities such as mitral valve prolapse.
DD: 1.a prolonged QT interval ---- congenital QT syndrome --- nonsustained polymorphic ventricular tachycardia (torsade de pointes) 1. Electrolye abnormalities (hypokalemia/hypomagnesemia) --- polymorphic ventricular tachycardia |
|
|
Preoperative cardiac testing
|
Low risk procedure ---- risk of cardiac death or nonfatal MI is < 1%
Endoscopic procedure, most ambulatory or superficial surgeries Further preoperative cardiac testing is usually not required Intermediate risk proecedure Intrathoracic, intraperitoneal or orthopedic surgery High risk procedure: vascular surgery |
|
Acute pericarditis following a transmural MI
|
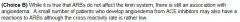
Acute pericarditis 1-4 days following a transmural MI is usually transient and should be managed by pain control with aspirin;. There are some concerns that other NSAIDs may increase the risk of myocardia rupture after a transmural MI
|
|
Lidocaine
|
Lidocaine is the drug of choice for pt with TCA-induced ventricular arrhythmias.
TCA --- hypotensive, anticholinergic effects, CNS manifestations, cardiac arrhythmia TCA inhibit fast sodium channels, which result to slowing of the phase 0 depolarization in His-Purkinje tissue and the myocardium ---- QRS prolongation and reentrant arrhythmia like ventricular tachycardia, ventricular fibrillation and torsades de pointes occlusion EKG Inferior infarction RCA inferior leads II, III, and aVF. diaphragmatic surface of the heart Posterior infarction RCA looking for reciprocal changes in the anterior leads, especially V1. Lateral infarction CFX left lateral leads I, aVL, V5, and V6 left lateral wall of the heart Anterior infarction LAD precordial leads (V1 -V6) the anterior surface of the left ventricle The 2 most commonly used antihypertensive agents in the management of hypertensive crisis complicated by acute pulmonary edema are IV nitroglycerine and IV nitroprusside |
|
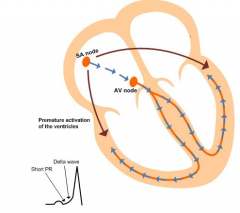
Wolff-Parkinson-White syndrome
|
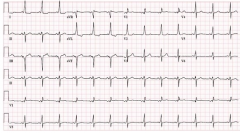
ECG: short PR interval < 0.12sec, delta wave and wide QRS complex > 0.12sec. Development of atrial fibrillation can be dangerous as it can result in ventricular fibrillation and cardiac arrest.
Although pt with WPW pattern on EKG can be completely asymptomatic, some develop tachyarrhythmias. Paroxysmal supraventricular tachycardia is the most common arrhythmia. It is usually a regular, narrow complex tachycardia. If pt with ventricular preexcitation develop atrial fibrillation, they can conduct down the accessory pathway from the atria to the ventricles at a very fast rate, therefore syncope and collapse are common. Alcohol can be precipitant for atrial fibrillation. Tx: catheter-ablation therapy is the recommended therapy in symptomatic pt with WPW syndrome. Cathe-ablation therapy has a nearly 90% efficacy rate and < 5% risk of complications, replacing surgical ablation as the preferred treatment for accessory pathways. |
|
Torsade de pointes – nonsynchronized electric defibrillation
|
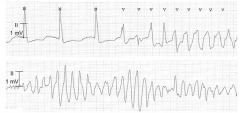
Synchronized electric defibrillation is indicated for pt with stable ventricular tachycardia, AF, atrial flutter or supra ventricular tachycardia.
Magnesiu sulfate is the drug of choice in stable pt. It should be administered regardless of the pt’s serum Mg levels. Mg prevents the recurrence of arrhythmia. Benefits are seen even if there is no readily observed improvement or changes in the EKG findings (shortening of the QT interval) and serum Mg levels. Amiodarone can potentially casue torsade de pointes. It is contraindicated in pt with torsades. Because of the polymorphic nature of torsades de pointes, synchronized cardioversion may not be possible, and the patient may require an unsynchronized shock (or defibrillation). Defibrillation is a common treatment for life-threatening cardiac dysrhythmias, ventricular fibrillation, and pulseless ventricular tachycardia. Defibrillation consists of delivering a therapeutic dose of electrical energy to the affected heart with a device called a defibrillator. |
|
|
Torsade de pointes – nonsynchronized electric defibrillation
|

|
|
|
MI-SEX
|
All pt should refrain from sexual activity for the first 2w following myocardial infarction. Post –MI pt who have undergone coronary revasculization are considered low-risk for repeat MI and can resume sexual activity at 6w.
|
|
|
Coronary artery bypass graft
|
Coronary artery bypass graft is indicated in pt with severe 3 vessel coronary artery disease or left main disease.
CABG improves long-term survival in DM pt with multivessel disease and recent Q-wave infarction compared to angioplasty. Good perioperative control of the blood glucose levels is advocated during CABG. An insulin drip achieves better bood glucose control during CABG and decrease the incidence of sternotomy wound infections. |
|
|
Drug-induced lupus
|
Hydralazine (increase cGMP levels), procainamide, penicillamine, isoniazid, minocycline, diltiazem, methyldopa, chlorpromazine, interfereon-a
Flu-like symptoms: Fever, malaise, arthralgias, myalgias and maculopapular facial rash, Lymphadenopathy, splenomegaly, pleurisy and pericarditis, antihistone antibody (+) |
|

Chronic stable angina
|
Coronary angiography should be used to risk stratify pt with evidence of heart failure, a high likelihood of severe coronary artery disease or disabling anginal symptoms.
|
|
|
Unstable angina
|
Deciding Between the Conservative and the Invasive Approaches to Treatment
In addition to stabilization, which is done in all patients with these conditions, early catheterization with angioplasty and stenting is recommended in many patients with unstable angina and NSTEMI. Generally, if you are considered a low-risk patient, your doctor may choose to manage your condition without immediate invasive therapy. Otherwise, an invasive approach is clearly preferable. The risk score that is used to make this determination is the "TIMI" score, taken from the TIMI clinical trials. This score is determined by looking for the following seven clinical features: • Age 65 years or older • Presence of at least three risk factors for CHD (hypertension, diabetes, high lipids, smoking, or family history of early MI) • Prior coronary blockage of > 50% • Presence of ST segment deviation on admission ECG • At least two angina episodes in prior 24 hours • Elevated cardiac enzymes • Use of aspirin in prior seven days(which is probably a marker for more severe coronary disease) If you have two or fewer of these seven risk factors (that is, a TIMI score of 2 or less), many cardiologists will choose to manage your condition without immediate cardiac catheterization, as long as your clinical condition stabilizes quickly. Otherwise your doctor will want you to go to the catheterization laboratory soon after stabilization measures have been initiated. If you do not receive invasive therapy, you should have stress testing prior to hospital discharge, and if you show signs of continued cardiac ischemia on stress testing, you will likely be sent for cardiac catheterization before going home. |
|
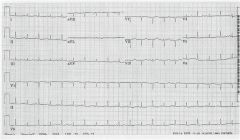
Cardiac tamponade
|
Cardiac tamponade will cause a limitation of fluid entering the ventricles and an ECHO will reveal diastolic collapse of both the right atrium and ventricle.
A marked inspiratory drop in systolic BP > 20mmHg is an important physical finding in cardiac tamponade, also seen in severe COPD and constrictive pericarditis. ECG: low limb voltage with alternating size of QRS complex due to swinging of the heart (DD: acute pericarditis --- diffuse ST segment elevation and PR depression in all leads, treat with NSAIDs) CXR” enlarged cardiac silhouette PE: muffled/distant heart sounds QRS alterns.. |
|
|
Cocaine-related chest pain
|
Management is similar to that of chest pain in the general population with a few key exceptions.
Benzodiazepines-lorazepam shoud be given early to decrease neuropsychiatric manifestation of cocaine use and thereby improve HTN and tachycardia. Beta-blockers should be avoided in pt with cocaine-related chest pain to avoid coronary vasospasm caused by unopposed alpha stimulation.. Cocaine incrased rate of MI and aortic dissection, and the risk of these complications is highest in the first hours after drug use. When BP does not improve with benzodiazepine, phentolamine is particularly effective and additionally decreases coronary artery vasospasm, although nitroprusside and nitroglycerine are also reasonable options. *** Cocaine-associated vasospasm may lead to coronary artery thrombosis, which can not be reversed by vasodilator agents. In pt with transmurial ischemia (ST elevation), the initial treatment regimen consist of nitrate or CBC, aspirin and benzodiazepine. If the pt does not improve with these durgs. Immediate coronary angiography should be performed to check for any coronary thrombus. |
|
|
Mobitz II second-degree AV block
|
EKG: bradycardia with preservation of the PR interval, periodic loss of QRS complex.
Can cause dizziness, episodes of syncope or transient altered mental status Tx: permanent cardiac pacemarker insertion. At least 2 negative troponins spaced 6h apart are needed to exclude myocardial infarction. Outpatient management of chest discomfort should only be considered in pt where there is a clear alternative explanation or the chest pain or in very young pt where suspicion for CAD is low. Stress testing should only be done after MI has been excluded with serial troponins. |
|
|
e bradycardia after an acute inferior wall MI
|
Symptomatic severe bradycardia after an acute inferior wall MI is usually transient and typically resolves within the next 24h. Pt are usually asymptomatic and require no further treatment, however severe bradycardia can result in low cardiac output and thereby cause hypotension and subsequent hemodynamic compromise, as well as worsening of ongoing ischemia.
Tx: atropine |
|
|
Hydrochlorothiazide --- photo sensitivity
|
Thiazides are sulfonamides, hydrochlorothiazide use can cause photosensitivity rash
Tx: discontinue drug, sunscreen, avoid sun exposure For pt being medically managed, smoking cessation is the intervention with the greatest likelihood of slowing AAA progression. |
|
|
Thiazolidinedione --- fluid retention, pulmonary edema
|
The thiazolidinedione medications (pioglitazone) can result in fluid retention via PPAR- agonist effects on the renal collectin/g tubule resulting in sodium reabsorption. This effect is uaually seen in pt with underlying heart failure.
|
|
|
Long-acting antipsychotics
|
Haloperidol decanoate, risperidone, fluphenazine
|
|
|
Insomnia in elderly
|
Behavioral therapy and relaxation techniques
|
|
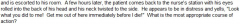
Acute dystonic reactions
|
Acute dystonic reactions from antipsychotic medication
Tx: anticholinergic medications (benztropine or thihexyphenidyl) or diphenhydramine. |
|
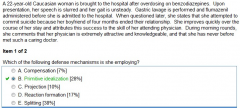
Primitive idealization
|
Pt with borderline personality disorder tend to use a psychological defense mechanism known as splitting, in which an external objects are classified as wholly good or wholly bad. Primitive idealization is one aspect of splitting in which another individual is viewed as perfect.
|
|

Dialectical方言的behavior therapy --- borderline personality disorder
|
The most recognized psychotherapeutic strategy for OCD is cognitive-behavioral therapy, which involves identifying and correcting cognitive errors and changing one’s behavior with techniques such as desensitization and conditioning.
SSRI are the medications of choice for OCD. The tricyclic antidepressant clomipramine can also be used. Conditioning ---- Tx for phobia. |
|
|
Bipolar pregnant women
|
Electroconvulsive therapy is the treatment o choice for severely manic pregnant pt, especially if the risk of suicide is great.
|
|
|
Good prognostic indicators in psychotic
|
pt include acute symptoms onset, stable social support, good premorbid functioning, no past psychiatric history, no family history of psychiatric illness and a known precipitating factor for the psychosis. In addition, it has been shown that pt who primarily have hallucinations, delusions or disorganized thought have less impairment of function than do those with predominantly negative symptoms (blunted affect, loss of motivation or anhedonia)
|
|
|
Serotonin syndrome
|
SSRI: FLoxetine, PARoxetine, SErtraline, CIalopram
MAOI: Tranylcypromine, Phenelzine, Isocarboxazid, Selegiline (selective MAO-B inhibitor) Serotonin syndrome: similar presentation to malignant neuroleptic syndrome, fever, hyperthermia diaphoresis, tachycardia, agitation and muscular rigidity, myoclonus, cardiovascular collapse, flushing, diarrhea, seizure Tx: 5-HT2 antagonist: cyproheptadine |
|
|
Urine immunoassay screens
|
for drug abuse are inexpensive and rapid. They usually provide results within one hour. They detect tricyclinc antidepressants, tetrahydrocannadinol, opiates, benzodiazepines, cocaine metabolites, barbiturates, phencyclidine, salicylates, and acetaminophen. Due to the rapidity of the rest, they can influence the management of the patients.
|
|
|
Drug addiction
|
Drug rehabilitation programs are ther preferred means of initiating recovery from drug addiction, while group therapy programs (Alcoholics Anonymous) are the preferred means of maintaining drug and alcohol abstinence.
Inpatient hospitalization would be indicated in pt who was experiencing physical withdrawal symptoms or who posed a danger to himself or others. Once the pt is medically stable, however, he/she should be placed in a drug rehabilitation program that can better accomplish the short and long-term goals of recovery. |
|
|
Narcolepsy
|
Behavioral interventions are an important component of therapy for pt with narcolepsy. Keeping a rigid and adequate sleep schedule is often helpful because these pt do not need more sleep compared to healthy controls. To reduce the inappropriate sleep episodes, scheduling 1 or 2 naps during the day is effective. A brie nap can significantly reduce daytime sleepiness in narcolepsy pt, unlike the sleepiness of sleep apnea and other disorders associated with poor quality sleep.
Hypnagogic/hypnopompic hallucinations do not require treatment with neuroleptic drugs. Tx: Modafinil (increases the release of monoamines) is used to treat excessive sleepiness caused by narcolepsy Amphetamine |
|
|
Major depression
|
In pt with a first episode of depression, antidepressant medications should be continued for > 6m after remission of their depressive symptoms.
|

