![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
679 Cards in this Set
- Front
- Back
|
4 categories of child abuse. |
physical
sexual psychological neglect |
|
|
What's a dead giveaway of child abuse?
|
history is discordant with physical findings
or if there is a delay in obtaining appropriate medical care |
|
|
What 3 signs are dead giveaways of sexual abuse?
|
genital:
trauma bleeding discharge |
|
|
What are sx of vaginal foreign body?
|
foul-smelling vaginal d/c, bleeding, pain
|
|
|
What can be easily mistaken for physical abuse?
|
mongolian spots
(common in first few years of life) |
|
|
Vaginal d/c that is cultured positive for an organism can suggest sexual abuse. Between G and C, which one is definitive evidence for sexual abuse?
|
Neisseria gonorrhea
definitive evidence of sexual abuse Chlamydia trachomatis can be acquired from the mother during delivery and can persist for up to 3 years |
|
|
Risk factors for child abuse.
|
parents with a hx of alcoholism or drug use
children with MR, handicap, repeated hospitalizations |
|
|
Clinical presentation of child abuse in infants.
|
abuse or neglect in infants:
apnea sz feeding intolerance somnolence FTT |
|
|
Clinical presentation of child abuse in older children.
|
poor hygiene
behavioral abnormalities |
|
|
Physical Exam
Child Abuse |
bruises
burns fractures |
|
|
Describe the burns that represent child abuse.
|
the burn marks are geometric patterns, like:
cigarette burns belt marks stocking-glove burns found in atypical places (face, thighs) |
|
|
Describe the fractures that represent child abuse.
|
Spiral fractures of the humerus and femur
epiphyseal-metaphyseal "bucket fractures" shaking or jerking child's limbs (highly diagnostic) posterior rib fractures (caused by squeezing chest) |
|
|
Name some conditions that mimic bruising.
|
bleeding d/o
Mongolian spots |
|
|
Name some conditions that mimic fractures.
|
osteogenesis imperfecta
|
|
|
Name some conditions that mimic burns.
|
bullous impetigo
"coining" (like what they do in asian cultures) |
|
|
How do you diagnose bone fractures in child abuse?
|
x-ray skeletal survey
may not show up in x-ray until 1-2 weeks after injury bone scan shows fractures in various stages of healing, as early as 48 hrs |
|
|
What lab tests do you get if suspect sexual abuse?
How fast should you get these tests? |
gonorrhea
chlamydia syphilis HIV sperm get within 72 hrs of assault |
|
|
How do you r/o shaken baby syndrome?
|
opthalmologic exam for retinal hemorrhages
non-contrast CT for subdural hematomas head MRI to visualize white matter changes assoc with violent shaking and bleedings |
|
|
Tx
Child Abuse |
document injuries
(location, size, shape, color, etc) notify Child Protective Services for possible removal of child from home hospitalize if necessary to tx and protect child |
|
|
CONGENITAL HEART DISEASE
Describe the general idea behind acyanotic conditions. |
"pink babies"
have L to R shunts in which oxygenated blood from lungs is shunted back into pulm circulation |
|
|
CONGENITAL HEART DISEASE
Describe the general idea behind cyanotic conditions. |
"blue babies"
have R to L shunts in which deoxygenated blood is shunted into the systemic circulation |
|
|
CONGENITAL HEART DISEASE
The 5 T's that have R to L shunts and briefly describe each one. HINT: 1-2-3-4-5 |
Truncus Arteriosus
ONE arterial vessel arising from both ventricles Transposition of the great vessels TWO arteries switched Tricuspid atresia THREE Tetralogy of Fallot FOUR Total anomalous pulmonary venous return FIVE words |
|
|
Of the 5 T's of congenital heart disease, which one causes severe cyanosis and presents within the first few hours of life?
|
Transposition of the great vessels
|
|
|
CONGENITAL HEART DISEASE
Name 3 noncyanotic heart defects. |
The 3 Ds
VSD ASD PDA |
|
|
Most common congenital heart disease.
|
VSD
|
|
|
What conditions commonly feature a VSD?
|
fetal alcohol syndrome
TORCH Apert's syndrome cri du chat ALL THE TRISOMIES THAT SURVIVE Down syndrome Trisomies 13 Trisomies 18 |
|
|
What is Apert's syndrome?
|
cranial deformities
fusion of the fingers and toes |
|
|
Clinical Presentation
VSD at Birth (HINT: depends on small vs large defects) |
FOR SMALL DEFECTS
usually asymptomatic at birth FOR LARGE DEFECTS frequent respiratory infections dyspnea FTT CHF |
|
|
Physical Exam
VSD at Birth (HINT: depends on small vs large defects) |
FOR SMALL DEFECTS
harsh holosystolic murmur LLSB FOR LARGE DEFECTS soft holosystolic murmur that is more blowing accompanied by systolic thrill, crackles, hepatomegaly, narrow S2 with an increased P2, mid-diastolic apical rumble reflecting increased flow across mitral valve |
|
|
Diagnosis
VSD |
ECHO
is diagnostic EKG LVH and maybe RVH CXR cardiomegaly increased pulm vascular markings |
|
|
Tx
VSD (HINT: depends on small vs large defect) |
SMALL DEFECTS
close spontaneously monitor with echo abx during procedures if the VSD was previusly repaired with prosthetic material LARGE DEFECTS surgery if symptomatic or fail medical mgmt, < 1yo w/ signs of pulm HTN, older children whose VSD did not change in size |
|
|
Tx for VSD sx
|
CHF SX
diruetics inotropes ACEIs |
|
|
ASDs are associated with what conditions?
|
Holt-Oram syndrome
fetal alcohol syndrome Down syndrome |
|
|
Name 3 findings in Holt-Oram syndrome.
|
ASD
first-degree heart block absent radii (radius bone not developed) |
|
|
There are two types of endocardial cushion defects:
Ostium primum ASD Ostium secundum ASD Describe what ostium primum ASD is. |
less common than ostium secundum ASD
it is a defect in the atrial septum that is located at the level of the mitral/tricuspid valve it is also very close to where the atrial and ventricular septum meet this area is called the endocardial cushion where valves and septum meet |
|
|
There are two types of endocardial cushion defects:
Ostium primum ASD Ostium secundum ASD Describe what ostium secundum ASD is. |
more common than ostium primum ASD
most common type of ASD |
|
|
An ostium primum ASD is also known as:
|
atrioventricular septal defect
|
|
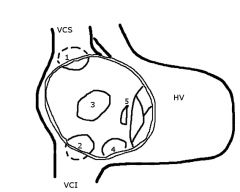
Which one is the ostium primium and secundum ASD?
|
3
ostium secundum 5 ostium primum |
|
|
Sx of ASD
(both ostium primum and secundum) |
easy fatigability
frequent respiratory infections FTT frequently asymptomatic |
|
|
At what age do ostium primum and secundum sx appear?
|
OSTIUM PRIMUM
early childhood OSTIUM SECUNDUM late childhood early adulthood |
|
|
PHYSICAL EXAMINATION
ASD |
RV heave
wide adn fixed, split S2 systolic ejection murmur at LUSB (from increased flow across pulm valve) may also be mid-diastolic rumble at LLSB |
|
|
DIAGNOSIS
ASD |
ECHO with color flow Doppler
- reveals blood flow between atria - paradoxical ventricular wall motion - dilated RV EKG RVH RAE PR prolongation is common CXR cardiomegaly increased pulm vascular markings |
|
|
TX
ASD |
90% of defects close spontaneously and do not require tx
SURGERY surgical or catheter closure is indicated in infants with CHF and in pts with a 2:1 ratio of pulmonary to systemic blood flow |
|
|
Complications of ASD if left uncorrected.
|
Arrythmias
RV dysfunction Eisenmenger's syndrome |
|
|
Do ASDs and VSDs normally present at birth?
|
rarely, unless Eisenmenger's syndrome has developed
(R to L and cyanosis) remember ASD, VSD, PDA are acyanotic conditions |
|
|
Mechanism behind the sx of PDA.
|
failure of the ductus arteriosus to close
leads to L to R shunt (aorta to pulmonary artery) |
|
|
Risk factors of PDA.
|
1st trimester Rubella infection
prematurity female gender |
|
|
Clinical Presentation
PDA |
SMALL DEFECTS
asymptomatic LARGE DEFECTS FTT recurrent lower respiratory tract infections lower extremity clubbing CHF |
|
|
PHYSICAL EXAM
PDA |
continuous "machinery murmur"
2nd intercostal, left sternal border loud S2 wide pulse pressure bounding peripheral pulses |
|
|
What causes bounding peripheral pulses?
|
high LV stroke volume
or low diastolic pressure as blood runs off the systemic into the pulmonary circulation |
|
|
What is wide pulse pressure?
Give some examples that causes this. |
difference systolic and diastolic pressure
wide pulse pressure is usually caused by: HTN hardening of arteries/plaques/athero shunting aortic regurg increased HR |
|
|
DIAGNOSIS
PDA |
color flow Doppler
shows blood flow from aorta into pulm artery is diagnostic ECHO larger PDAs show LAE, RVE EKG LVH CXR cardiomegaly (if PDA is large) |
|
|
Tx
PDA |
MEDICAL MGMT
INDOMETHACIN - unless the PDA is needed for survival - or if there's a contraindication SURGICAL CLOSURE - if indomethacin FAILS - or if child > 6-8 mo |
|
|
Mnemonic for PDA tx with indomethacin.
|
Come IN and CLOSE the door.
Give INdomethacin to CLOSE a PDA |
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: ASD and endocardial cushion defects |
Down syndrome
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: PDA |
congenital rubella
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: coarctation of the aorta |
Turner's syndrome
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: coronary artery aneurysms |
Kawasaki disease
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: Congenital heart block |
neonatal lupus
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: supravalvular aortic stenosis |
Williams syndrome
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: conotruncal abnormalities |
Tetralogy of Fallot
(overriding aorta) Truncus arteriosus DiGeorge syndrome (Tetralogy) Velocardiofacial syndrome |
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: bicuspid aortic valve |
Turner's syndrome
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: Ebstein's anomaly |
maternal lithium use during pregnancy
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: Heart failure |
neonatal thyrotoxicosis
|
|
|
PEDIATRIC HEART CONDITIONS AND THEIR DISEASE ASSOCIATIONS
What disease is associated with: asymmetric septal hypertrophy and transposition of the great vessels |
maternal diabetes
|
|
|
What are 4 things that can cause a shock-like state within the first few weeks of life?
|
1 - sepsis
2 - inborn errors of metabolism 3 - ductal-dependent congenital heart disease 4 - congenital adrenal hyperplasia |
|
|
Coarctation of the aorta is associated with 3 conditions:
|
1 - Turners
2 - berry aneurysms 3 - male gender |
|
|
More than 2/3 of pts with coaractation of the aorta also have what other finding?
|
bicuspid aortic valve
|
|
|
In what conditions is a PDA needed for survival?
|
transposition of the great vessels
tetralogy of Fallot hypoplastic left heart IN CRITICAL COARCTATION OF AORTA |
|
|
When is indomethacin contraindicated?
|
intraventricular hemorrhage
|
|
|
98% of coarctation of aorta is located where?
|
just distal to the left subclavian artery
|
|
|
Clinical Presentation
Coarctation of the Aorta |
asymptomatic HTN
(upper extremity HTN) lower extremity claudication syncope epistaxis HA |
|
|
Classical Physical Exam
Coarctation of the Aorta |
upper extremity HTN than lower extremity
different L and R arm BP indicates the position of the coarctation |
|
|
Additional Physical Exam
Coarctation of the Aorta |
murmur btw scapulae
weak femoral pulses radiofemoral delay short systolic murmur in the left axilla forceful apical impulse |
|
|
Coarctation of the Aorta
Describe the differential cyanosis in the limbs. |
the left arm and lower extremities have a LOWER O2 SATURATION than the lower extremities
the right arm is preductal, whereas the left and lower extremities are postductal |
|
|
DIAGNOSIS
Coarctation of the Aorta |
ECHO AND COLOR FLOW DOPPLER
diagnostic CXR cardiomegaly pulm congestion "3" sign (pre- and postdilatation of the coaractation with aortic wall indentation) "rib notching" (due to collateral circulation thru the intercostal arteires) |
|
|
Tx
Coarctation of the Aorta |
FOR SEVERE COARCTATION IN INFANCY
keep the ductus arteriosus open with prostaglandin E1 (PGE1) SURGICAL CORRECTION OR BALLOON ANGIOPLASTY is controversial MONITOR FOR: restenosis aneurysm development aortic dissection |
|
|
What is a secondary cause of hypertension in children?
|
coarctation
|
|
|
What is the most common CYANOTIC congenital heart lesion in the newborn?
|
transposition of the great vessels
|
|
|
Describe the transposition of the great vessels.
|
aorta --> RV
pulm artery --> LV this creates a parallel pulmonary and systemic circulation |
|
|
In transposition of the great vessels, what is required to keep the infant alive?
|
ASD
VSD PDA |
|
|
Risk factors for transposition of the great vessels.
|
diabetic mothers
DiGeorge syndrome |
|
|
Clinical Presentation
transposition of the great vessels |
cyanosis within the first few hrs of life
|
|
|
Physical Exam
transposition of the great vessels |
FROM TRANSPOSITION
tachpynea progressive hypoxemia extreme cyanosis FROM CHF single loud S2 FROM OTHER DEFECTS VSD systolic murmur at left sternal border |
|
|
Diagnosis
transposition of the great vessels |
Echo
CXR "egg-shaped silhouette" - narrow heart base - absence of main pulm artery segment - increased pulm vascular markings |
|
|
Tx
transposition of the great vessels |
Open the PDA with IV PGE1
If cannot open PDA and surgery is not feasible, perform balloon atrial septostomy to create/enlarge an ASD Surgical correction is definitive |
|
|
DiGeorge syndrome
Mnemonic CATCH 22 |
Cardiac abnormalities (transposition and tetralogy)
Abnormal facies Thymic aplasia Cleft palate Hypocalcemia 22q11 deletion |
|
|
What is the most common cyanotic heart diseae of childhood?
|
tetralogy of fallot
|
|
|
Briefly, the tx for transposition of the great vessels and tetralogy of Fallot are treated the same way. Describe the tx.
|
both are initially treated with PGE1, but are definitively treated with surgical correction
|
|
|
Name 4 elements of Tetralogy of Fallot.
|
pulmonary stenosis
overriding aorta RVH VSD |
|
|
What is the cause of the early cyanosis in tetralogy?
|
R to L shunt across the VSD
|
|
|
Risk factors for tetralogy of fallot.
|
maternal PKU
DiGeorge syndrome |
|
|
Clinical Presentation
Tetralogy of Fallot |
begins in early CHILDHOOD
(not infancy) dyspnea fatigability cyanosis is frequently absent at birth |
|
|
The degree of cyanosis in tetralogy of fallot is related to what?
|
severity of cyanosis is related to extent of pulmonary stenosis
as right-sided pressures decrease in the first few weeks after birth (pulm stenosis decreases), shunt direction reverses and cyanosis decreases if pulm stenosis is severe, right-sided pressures may remain high and cyanosis worsens over lifetime |
|
|
Clinical Presentation
Tetralogy of Fallot Why do children squat? |
to relieve hypoxemic episodes called "tet" spells
squatting increases systemic vascular resistance --> increases aortic wave reflection --> increasing pressure on the left side of the heart --> decreasing the right to left shunt --> thus decreasing the amount of deoxygenated blood entering the systemic circulation |
|
|
Clinical Presentation
Tetralogy of Fallot Long-term hypoxemia may lead to what? |
FTT
mental status changes |
|
|
Physical Exam
Tetralogy of Fallot |
systolic ejection murmur at LUSB
(RV outflow obstruction) RV heave single S2 |
|
|
Diagnosis
Tetralogy of Fallot |
ECHO and Catherization
CXR "boot-shaped heart" decreased pulmonary vascular markings (but remember that a VSD may result in increased pulm vascular markings) EKG RVH right-axis deviation |
|
|
Tx
Tetralogy of Fallot |
PGE1 to keep PDA open if stenosis is severe
O2 (to treat hypercapnic tet spells) propanolol phenylephrine knee-chest positoin fluids morphine TEMPORARY PALLIATION create an artificial shunt (balloon atrial septostomy) DEFINITIVE surgical correction |
|
|
Definitive surgical correction of Tetralogy of Fallot is named after who?
|
Blalock-Taussig shunt
|
|
|
What are 4 areas of developmental milestones?
|
gross motor
fine motor language social/cognitive |
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 2 months |
lifts head/chest when prone
|
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 4-5 months |
rolls front to back and back to front
|
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 6 months |
sits unassisted
|
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 9-10 months |
crawls
pulls to stand |
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 12 months |
walks alone
throws object |
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 2 years |
walks up/down steps
jumps |
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 3 years |
rides tricycle
climbs stairs with alternating feet |
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 4 years |
hops
|
|
|
DEVELOPMENTAL MILESTONES
GROSS MOTOR Age: 5 years |
skips
walks backward for long distances |
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 2 months |
tracks past midline
|
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 4-5 months |
grasps rattle
|
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 6 months |
demonstrates raking grasp
transfers objects from hand to hand |
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 9-10 months |
uses 3-finger pincer grasp
(immature grasp) |
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 12 months |
uses 2-finger pincer grasp
(mature grasp) |
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 2 years |
builds tower of 6 cubes
|
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 3 years |
copies a circle
uses utensils |
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 4 years |
copies a cross
(square at 4.5 years) |
|
|
DEVELOPMENTAL MILESTONES
FINE MOTOR Age: 5 years |
copies a triangle
ties shoelaces knows L and R prints letters |
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 2 months |
alerts to sound
coos |
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 4-5 months |
laughs and squeals
orients to voice begins to make consonant sounds |
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 6 months |
babbles
(talking but no one understands) |
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 9-10 months |
says "mama/dada"
says first word at 11 months |
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 12 months |
uses 1-3 words
follows 1-step commands |
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 2 years |
uses 2-word phrases
follows 2-step commands |
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 3 years |
uses 3-word sentences
|
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 4 years |
knows colors and some numbers
|
|
|
DEVELOPMENTAL MILESTONES
LANGUAGE Age: 5 years |
uses 5-word sentences
|
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 2 months |
smile and recognize parents
|
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 4-5 months |
laugh and look around
|
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 6 months |
demonstrates stranger anxiety
|
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 9-10 months |
waves bye-bye
plays pat-a-cake |
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 12 months |
imitates actions
exhibits separation anxiety |
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 2 years |
removes clothes
|
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 3 years |
brushes teeth with help
washes/dries hands |
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 4 years |
exhibits cooperative play
plays board games |
|
|
DEVELOPMENTAL MILESTONES
SOCIAL/COGNITIVE Age: 5 years |
exhibits domestic role playing
plays dress-up |
|
|
How much weight do newborns lose right-away?
How fast do they regain that weight? |
they lose up to 10% of their weight
regains this weight by 2 weeks of life |
|
|
Signs of autism in terms of not meeting developmental milestones.
(4) |
no babbling and/or gesturing by 12 months
no single words by 16 months no 2-word phrases by 24 months failure to make eye contact other deficits in language/social skills |
|
|
In a child with FTT, what do the growth curves look like?
WEIGHT curve HEIGHT curve HEAD CIRCUMFERENCE curve |
first they will fall off the weight curve
then the height curve then the head circumference curve |
|
|
Each well-child check should include plotting of what values?
|
height
weight head circumference |
|
|
Increased head circumference indicates what?
|
hydrdocephalus
tumor |
|
|
Decreased head circumference indicates what?
|
microcephaly
(TORCH infections) |
|
|
What is the pattern of weight changes in the first year of life?
|
lose 10% of birth weight (BW) in first few days
regains BW in 14 days doubles weight in 4-5 months triple weight in 1 year quadruple weight in 2 years |
|
|
Define FTT in two different ways.
|
(1)
persistent weight less than the 5th percentile for age (2) "falling-off the growth curve" crossing 2 major percentile lines on a growth chart |
|
|
What is organic FTT?
|
due to an underlying medical condition:
cystic fibrosis congenital heart disease celiac sprue pyloric stenosis chronic infection (HIV) GERD |
|
|
What is non-organic FTT?
|
psychosocial factors:
maternal depression neglect abuse |
|
|
DIAGNOSIS
FTT |
get a careful dietary history
close observation of maternal-infant interactions (esp preparation of formula and feeding) BOTH OF THESE ARE CRITICAL |
|
|
Tx
Children who are neglected or severely malnourished |
hospitalize the child
calorie counts supplemental nutrition (if breastfeeding is inadequate) |
|
|
Major Milestones in Language Development
When should they meet the following milestone? 1-word, 1-step commands |
12 months
|
|
|
Major Milestones in Language Development
When should they meet the following milestone? 5 words |
15 months
|
|
|
Major Milestones in Language Development
When should they meet the following milestone? 8 words |
18 months
|
|
|
Major Milestones in Language Development
When should they meet the following milestone? 2-word phrases, 2-step commands |
2 years
|
|
|
Major Milestones in Language Development
When should they meet the following milestone? 3-word phrases |
3 years
|
|
|
Describe the 4-step process of normal sexual development in a girl.
|
1 - thelarche (breast buds)
2 - pubarche (pubic hair) 3 - growth spurt 4 - menarche (menses) |
|
|
Describe the 4-step process of normal sexual development in a boy.
|
1 - gonadarche (testicles enlarge)
2 - pubarche (pubic hair) 3 - adrenarche (axillary/facial hair, voice changes) 4 - growth spurt |
|
|
Average age of puberty in girls in US.
|
10.5 yo
(5th-6th grade) |
|
|
Average age of menarche in girls in US.
|
12.5 yo
(roughly middle school) |
|
|
Average age of puberty in boys.
|
11.5 yo
(roughly middle school) |
|
|
Define delayed puberty in boys.
|
no testicular enlargement in boys by 14
|
|
|
Define delayed puberty in girls.
|
no breast development or pubic hair by 13
|
|
|
What is constitutional growth delay?
|
normal variant
growth curve lags behind others of the same age, but is consistent + family history children will often catch up and reach their target height potential |
|
|
What are some pathologic causes of delayed puberty?
HINT: systemic (2) congenital/genetic (2) endocrine (5) |
SYSTEMIC DISEASES
IBD malnutrition (anorexia) CONGENITAL gonadal dysgenesis (Klinefelter, Turners) ENDOCRINE ABNORM hypopituitarism hypothyroidism Kallmann's syndrome androgen insensitivity Prader-Willi syndrome |
|
|
GENETIC ABNORMALITY
Down syndrome |
meiotoic nondisjunction
(95%) robertsonian translocation (4%) mosaicism (1%) |
|
|
GENETIC ABNORMALITY
Edwards' syndrome |
Trisomy 18
|
|
|
GENETIC ABNORMALITY
Patau's syndrome |
Trisomy 13
|
|
|
GENETIC ABNORMALITY
Klinefelter's syndrome (male) |
47,XXY
presence of an inactivated X chromosome (Barr body) |
|
|
GENETIC ABNORMALITY
Turner's syndrome (female) |
45,XO
missing 1 X chromosome no Barr body |
|
|
GENETIC ABNORMALITY
Double Y males |
47,XYY
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
What is associated with increased incidence of Down syndrome? |
advanced maternal age
|
|
|
COMMON CHARACTERSITICS OF GENETIC ABNORMALITIES
Physical Exam of Down Syndrome (8) |
MR
flat facial profile upslanted eyes epicanthal folds simian crease general hypotonia atlantoaxial instability extra neck folds (nuchal folds sometimes seen on prenatal US) |
|
|
COMMON CHARACTERSITICS OF GENETIC ABNORMALITIES
What are diseases commonly found in Down syndrome? |
duodenal atresia
Hirschsprung's disease congenital heart disease (most commonly AV canal defects - 60%; ASD, VSD, PDA - 20%) |
|
|
COMMON CHARACTERSITICS OF GENETIC ABNORMALITIES
Down syndrome is associated with increased risk of what other diseases? |
ALL
hypothyroidism early-onset Alzheimer's |
|
|
GENETIC ABNORMALITY
Pheylketonuria (PKU) |
AR
decreased pheylalanine hydroxylase - or - decreased tetrahydrobiopterin cofactor |
|
|
GENETIC ABNORMALITY
Fragile X Syndrome |
X-linked dominant
affects the methylation and expression of the FMR1 gene |
|
|
COMMON CHARACTERISTICS OF OF GENETIC ABNORMALITIES
Clinical Presentation of Edwards' sydrome |
severe MR
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Physical Exam of Edwards' syndrome |
rocker-bottom feet
low-set ears micrognathia clenched hands (overlapping 4th and 5th digits) prominent occiput |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Edwards' syndrome is assoc with what other findings? |
congenital heart disease
horseshoe kidneys |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
How long do pts with Edwards' syndrome have to live? |
within 1 year of birth
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Clinical Presentation of Patau's syndrome |
severe MR
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Physical Exam of Patau's syndrome |

micropthalmia
microcephaly cleft lip/palate "punched-out" scalp lesions polydactyly |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
What internal organ malformations are present in Patau's syndrome? |
holoprosencephaly
omphalocele |
|
|
What is holoproscencephaly?
|
during embryogenesis, the brain fails to split into R and L hemispheres
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
What other diseases are associated with Patau's syndrome? |
congenital heart disease
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
How long do pts with Patau's syndrome have to live? |
death within 1 year of birth
lots die in utero bc the holoprosencephaly is so severe and incompatible with life |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
What increases the chances of giving birth to a baby with Klinefelter's syndrome? |
advanced maternal age
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
What reproductive abnormality is commonly found in Klinefelter's syndrome? |
hypogonadism
dysfunctional testes or ovaries leads to low testosterone production (hypoandrogenism) or low estrogen production (hypoestrogenism) also leads to impaired spermatogenesis and ovulation (infertility) |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Physical Exam of Klinefelter's syndrome |
testicular atrophy
eunuchoid body shape (castrated male) tall stature long extremities ANDROGEN DEFICIENCY gynecomastia female hair distribution |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Tx of Klinefelter's syndrome |
give testosterone:
- to prevent gynecomastia - improve secondary sexual characterstics |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Is Turner's associated with advanced maternal age? |
NO
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Turner's syndrome is the most common cause of what condition and why? |
primary amenorrhea
due to ovarian dysgenesis (decreased estrogen) |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Internal organ malformations of Turners syndrome |
coarctation of the aorta
bicuspid aortic valve may have horseshoe kidney |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Physical Exam Turner's syndrome |
short stature
shield chest widely spaced nipples webbed neck decreased femoral pulses (due to coarctation of the aorta) NEONATAL PERIOD lymphedema of hands and feet horseshoe kidney |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
What is the most likely patient population that has double Y (47, XYY)? |
inmates
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Physical Exam Double Y males |
phenotypically normal!
very tall severe acne antisocial behavior (1-2% of XYY males) |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Pathogenesis of phenylketonuria (PKU) |
tyrosine becomes essential and phenylalanine builds up excess phenyl ketones
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
At what age do sx appear in PKU? |
asymptomatic at birth
presents within first few months of life |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Clinical Presentation PKU |
MR
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Physical Exam PKU |
fair hair and skin (light)
eczema blond hair blue eyes musty urine ordor |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
What kind of diseases are PKU pts at most risk of developing? |
heart disease
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Tx PKU |
remove phenylalanine from diet
(aka artificial sweeteners) add tyrosine to diet |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Special instructions to mother who has PKU |
a mother with PKU must restrict diet as stated earlier, before conception
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Clinical Presentation Fragile X syndrome |
2nd most common cause of genetic MR
autistic behaviors |
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Physical Exam Fragile X syndrome |
large jaw, testes, ears
|
|
|
COMMON CHARACTERISTICS OF GENETIC ABNORMALITIES
Karyotype of Fragile X syndrome may show what? |
a triplet repeat disorder may show genetic anticipation
|
|
|
What is genetic anticipation?
|
a phenomenon whereby the symptoms of a genetic disorder become apparent at an earlier age as it is passed on to the next generation
|
|
|
GENETIC ABNORMALITIES
Cystic Fibrosis What is the genetic abnormality? And what is the inheritance pattern? |
AR
mutations in CFTR gene on chromosome 7 |
|
|
Pathogenesis of cystic fibrosis
|
widespread exocrine gland dysfunction
|
|
|
How do you differentiate cystic fibrosis based upon the sx you get as an infant vs older?
|
INFANT
predominantly GI sx LATER IN LIFE pulmonary sx |
|
|
What is the first sign of cystic fibrosis?
|
meconium ileus
|
|
|
What is meconium ileus?
|
a mechanical obstruction in the ileum caused by meconium
the meconium becomes thick and congested |
|
|
Clinical Presentation
Cystic Fibrosis AGE: infancy |
meconium ileus
|
|
|
Clinical Presentation
Cystic Fibrosis AGE: childhood and later |
FTT
chronic sinopulmonary disease recurrent pulmonary infections *chronic cough* dyspnea hemoptysis chronic sinusitis |
|
|
What are the organisms involved in CF recurrent pulmonary infections?
|
Pseudomonas
S. aureus |
|
|
Pulmonary Physical Exam
CF AGE: childhood and later |
cyanosis
*digital clubbing* bronchiectasis rhonchi rales hyperresonance to percussion **NASAL POLYPOSIS** |
|
|
GI Physical Exam
CF AGE: childhood and later |
**greasy stools**
flatulence |
|
|
What are systemic findings in CF?
|
pancreatitis
rectal prolapse hypoproteinemia biliary cirrhosis jaundice esophageal varices |
|
|
Electrolyte disturbances in CF.
|
unexplained hyponatremia
"salty-tasting" skin type 2 DM |
|
|
Malabsorption sx in CF.
|
fat-soluble vitamin deficiency
A, D, E, K so any manifestations in the deficiencies of these vitamins |
|
|
Fertility status of CF.
|
male infertility
due to agenesis of the vas deferens |
|
|
Diagnosis
CF |
sweat chloride test > 60 mEq/L
if < 20 yo sweat chloride test > 80 mEq/L in adults |
|
|
How do you confirm a diagnosis of CF?
|
genetic testing
|
|
|
ABG results in CF.
|
hypochloremic alkalosis
|
|
|
How do you distinguish between carrier state for CF and actually having the disease?
|
do a sweat test
also, one good copy of the CFTR gene is all you need to prevent this disease, so CF is AR |
|
|
Medical Mgmt
CF |
PULMONARY SX
chest physical therapy bronchodilators corticosteroids abx (to cover Psudomonas) DNase GI / MALABSORPTION SX pancreatic enzymes fat-soluble vitamins A-D-E-K |
|
|
Diet recommendations for CF
|
high-calorie
high-protein |
|
|
Surgical Tx
CF |
lung or pancreas transplants
|
|
|
Life expectancy for CF
|
used to be ~ 20 years
with newer treatments past ~30 years |
|
|
LYSOSOMAL STORAGE DISEASE
MODE OF INHERITANCE Fabrys Disease |
X-linked recessive
|
|
|
LYSOSOMAL STORAGE DISEASE
MODE OF INHERITANCE Krabbe's Disease |
AR
|
|
|
LYSOSOMAL STORAGE DISEASE
MODE OF INHERITANCE Gaucher's Disease |
AR
|
|
|
LYSOSOMAL STORAGE DISEASE
MODE OF INHERITANCE Niemann-Pick Disease |
AR
|
|
|
LYSOSOMAL STORAGE DISEASE
MODE OF INHERITANCE Metachromatic Leukodystrophy |
AR
|
|
|
LYSOSOMAL STORAGE DISEASE
MODE OF INHERITANCE Hurler's Syndrome |
AR
|
|
|
LYSOSOMAL STORAGE DISEASE
MODE OF INHERITANCE Hunter's Syndrome |
X-linked recessive
Hunters need to see (no corneal clouding) to aim for the X. corneal clouding is seen in Hurler's syndrome |
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY What causes Fabrys disease? |
deficiency of alpha-galactosidase A
leads to accumulation of ceramide trihexoside in heart, brain, kidneys |
|
|
LYSOSOMAL STORAGE DISEASE
Clinical Presentation Fabrys Disease |
**severe neuropathic limb pain**
joint swelling skin rash (angiokeratomas) may have a family hx of: renal failure MI Stroke |
|
|
LYSOSOMAL STORAGE DISEASE
Physical Exam Fabrys Disease |
ANGIOKERATOMAS
benign cutaneous lesion of capillaries, resulting in small marks of red to blue color and characterized by hyperkeratosis TELANGIECTASIAS small dilated blood vessels near the surface of the skin or mucous membranes |
|
|
LYSOSOMAL STORAGE DISEASE
Fabrys disease can lead to what conditions? |
renal failure
MI and stroke (thromboembolic events) |
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY Krabbe's disease |
galactosylceramidase deficiency leads to absence of galactosylceramide and galactoside
leads to accumulation of GALACTOcerebroside in the brain |
|
|
LYSOSOMAL STORAGE DISEASE
Characteristics Krabbe's disease |
**progressive CNS degeneration**
optic atrophy spasticity death within first 3 yrs of life |
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY Gaucher's disease |
deficiency of *glucocerebrosidase*
leads to accumulation of GLUCOcerebroside in brain, liver, spleen, and bone marrow |
|
|
LYSOSOMAL STORAGE DISEASE
What are the appearance of Gaucher's cells? (from a skin bx) |
"crinkled paper"
enlarged cytoplasm |
|
|
LYSOSOMAL STORAGE DISEASE
Labs Gaucher's disease |
anemia
thrombocytopenia |
|
|
LYSOSOMAL STORAGE DISEASE
Presentation of Infantile Form Gaucher's disease |
early, rapid neurologic decline
|
|
|
LYSOSOMAL STORAGE DISEASE
Presentation of Adult Form Gaucher's disease |
(more common form)
compatible with normal life span does not affect the brain |
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY Neimann-Pick disease |
deficiency of sphingomyelinase leads to buildup fo SPHINGOmyelin cholesterol in reticuloendothelial and parenchymal cells and tissues
No man PICKs his nose with his sphinger. |
|
|
LYSOSOMAL STORAGE DISEASE
Life span of Niemann-Pick disease |
patients with type A die by age 3
|
|
|
LYSOSOMAL STORAGE DISEASE
Physical Exam Niemann-Pick disease |
cherry-red spot
hepatosplenomegaly |
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY Tay-Sachs Disease |
absence of hexosaminidase that leads to GM2 GANGLIOside accumulation
|
|
|
LYSOSOMAL STORAGE DISEASE
Clinical Presentation in Infants Tay-Sachs disease |
infants appear normal until 3-6 months of age
when weakness begins and development slows and regresses exaggerated startle response |
|
|
What is the startle response and at what age do you lose this reflex?
|
startle response
lifetime reflex brainstem reflex to protect the back of the neck (whole-body startle), or the eye (eyeblink), and facilitates escape from sudden stimuli |
|
|
LYSOSOMAL STORAGE DISEASE
Life span of tay-sachs disease. |
death by 3 yo
|
|
|
LYSOSOMAL STORAGE DISEASE
Physical Exam Tay-Sachs Disease |
cherr-red spot
NO hepatosplenomegaly |
|
|
LYSOSOMAL STORAGE DISEASE
Tay-Sachs carrier rate |
1 in 30 Jews of European descent
(1 in 300 for others) |
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY Metachromatic leukodystorphy |
deficiency of arylsulfatase A that leads to accumulation of SULFAtide in the brain, kidney, liver, and peripheral nerves
|
|
|
LYSOSOMAL STORAGE DISEASE
What causes the sx in metachromatic leukodystrophy? |
demyelination leads to progressive ataxia and dementia
|
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY Hurler's syndrome |
deficiency of alpha-L-iduronidase
|
|
|
LYSOSOMAL STORAGE DISEASE
Characteristics Hurler's Syndrome |
corneal clouding
MR gargoylism (coarse facial features) |
|
|
LYSOSOMAL STORAGE DISEASE
ETIOLOGY Hunter's syndrome |
deficiency of iduronate sulfatase
|
|
|
LYSOSOMAL STORAGE DISEASE
Characteristics Hunter's syndrome |
Hunter is a milder form of Hurlers
no corneal clouding mild MR Hunters need to see (no corneal clouding) to aim for the X (X-linked recessive). |
|
|
What is the most common cause of bowel obstruction in the first 2 years of life?
|
intussusception
|
|
|
Risk factors for intussusception.
|
potential lead points
(Meckel's diverticulum) intestinal lymphoma Henoch-Schonlein purpura parasites polyps adenovirus rotavirus celiac disease cF |
|
|
Whats the most common site for intussusception?
|
proximal to the ileocecal valve
|
|
|
Intussusception
Clinical Presentation |
abrupt-onset, colicky abdominal pain
flexed knees vomiting bloody mucus in stool ("currant jelly stool") hemoccult positive |
|
|
Intussusception
Physical Exam |
positive stool guaiac
palpable "sausage-shaped" RUQ abdominal mass absence of bowel in RLQ ("empty" on palpation) |
|
|
Diagnosis
Intussusception |
air-contrast barium enema is both diagnostic and therapeutic
|
|
|
Imaging
Intussusception |
abdominal plain films
- normal in early setting - later shows SBO, performation, soft tissue mass US "target sign" |
|
|
Other Tx
Intussusception |
fluids
lytes CBC for leukocytosis NG tube for decompression |
|
|
Emergent Tx
Intussusception |
if child is unstable or has peritoneal signs or if enema reduction is unsuccessful -->
surgical reduction and resection of gangrenous bowel |
|
|
Classic metabolic derangement in pyloric stenosis.
|
hypochloremic, hypokalemic metabolic alkalosis
(due to persistent emesis of HCl) |
|
|
What is pyloric stenosis?
|
hypertrophy of the pyloric sphincter
leads to gastric outlet obstruction |
|
|
What conditions are associated with pyloric stenosis?
|
tracheoesophageal fistula
a maternal hx of pyloric stenosis erythromycin ingestion |
|
|
Clinical Presentation
Pyloric Stenosis |
non-bilious emesis begins at 3 weeks of age
progresses to projectile emesis after feedings may suffer from malnutrition and dehydration |
|
|
Physical Exam
Pyloric Stenosis |
palpable olive-shaped,mobile, non-tender epigastric mass
visible gastric peristaltic waves |
|
|
Diagnosis
Pyloric Stenosis |
ABDOMINAL US
hypertrophic pylorus (US is the top choice) BARIUM STUDIES narrow pyloric channel "string sign" pyloric beak |
|
|
Tx
Pyloric Stenosis |
pyloromyotomy
fluids lytes |
|
|
Meckel's rule of 2's.
|
children under 2
2x more common in males 2 types of tissue (pancreatic/gastric) 2 inches long within 2 feet of ileocecal valve 2% of population |
|
|
What is the cause of meckel's diverticulum?
|
failure of the omphalomesenteric (or vitelline) duct to obliterate
the resulting heterotopic gastric tissue causes ulcers and bleeding |
|
|
Meckel's Diverticulum
Clinical Presentation |
asymptomatic, discovered incidentally
CLASSICAL PRESENTATION sudden, intermittent, painless rectal bleeding |
|
|
Complications
Meckel's Diverticulum |
intestinal obstruction
diverticulitis (may mimic acute appendicitis) volvulus intussusception |
|
|
Diagnosis
Meckel's Diverticulum |
DIAGNOSTIC
Meckel scintigraphy scan (technetium-99m pertechnetate) detects ectopic gastric tissue PLAIN FILMS limited use, but can help visualize obstruction or perforation |
|
|
Tx
Meckel's Diverticulum |
in presence of active bleeding, surgical excision of diverticulum together with adjacent ileal segment
(ulcers frequently develop in the adjacent ileum) |
|
|
What causes Hirschsprung's Disease?
|
congenital lack of ganglion cells in the distal colon
leads to uncoordinated peristalsis and decreased motility |
|
|
What is associated with Hirschsprung's disease?
|
male gender
Down sydnrome Waardenburg's syndrome MEN 2 |
|
|
Name 3 characteristics of Waardenburg's syndrome.
|
genetic d/o
varying degrees of deafness iris pigment (two eyes different color) hair hypopigmentation (white forelock) and of course, Hirschsprung's |
|
|
Clinical Presentation
Hirschsprung's Disease In Neonate |
failure to pass meconium within 48 hrs of birth
bilious vomiting FTT |
|
|
Clinical Presentation
Hirschsprung's Disease In children with less severe lesions |
chronic constipation
|
|
|
Physical Exam
Hirschsprung's Disease |
abdominal distention
explosive discharge of stool following a rectal examination lack of stool in the rectum abnormal sphincter tone |
|
|
Diagnosis
Hirschsprung's Disease (4 modalities) |
INITIAL IMAGING
barium enema shows narrowed distal colon with proximal dilation X-RAYS distended bowel loops with a paucity of air in the rectum ANORECTAL MANOMETRY detects failure of the internal sphincter to relax after distention of the rectal lumen DEFINITIVE rectal bx shows absence of myenteric (Auerbach's) plexus and submucosal (Meissner's) plexus along with hypertrophied nerve trunks enhanced with acetylcholinesterase stain |
|
|
Tx
Hirschsprung's Disease |
2-STAGE SURGICAL REPAIR
1 - create a diverting colostomy at time of diagnosis 2 - several weeks later perform a definitive "pull-through" procedure connecting the remaining colon to the rectum |
|
|
What is malrotation with volvulus?
|
congenital malrotation of the midgut results in abnormal positioning of the small intestine
|
|
|
What are the two characteristics of malrotation?
|
cecum in the right hypochondrium
(ie below the ribs on the right side, where the liver is) ligament of Treitz formation of fibrous bands (Ladd's bands) |
|
|
What effect do the fibrous bands of malrotation have?
|
predisposes to obstruction and constriction of blood flow
|
|
|
Clinical Presentation
Malrotation With Volvulus |
presents in 1st month of life with:
bilious emesis crampy abdominal pain abdominal distention blood or mucus in stool |
|
|
Diagnosis
Malrotation With Volvulus |
AXR
"bird-beak" appearance air-fluid levels could also be normal UPPER GI SERIES shows abnormal location of the ligament of Treitz |
|
|
Tx
Malrotation With Volvulus |
SURGERY
- emergent surgical repair when volvulus is gastric - surgery or endoscopy when volvulus is intestinal MGMT NG tube insertion to decompress the intesting IV fluids |
|
|
Post-surgical Complications of Malrotation
|
postsurgical adhesions can lead to obstruction and volvulus at any point in life
|
|
|
What is the most common GI emergency in neonates?
|
necrotizing entercolitis
|
|
|
Necrotizing Enterocolitis
Seen in what patient population? |
premature infants
but can occur in full-term infants |
|
|
Clinical Presentation
Necrotizing Enterocolitis |
present within first few days or weeks of life
feeding intolerance delayed gastric emptying abdominal distention bloody stools |
|
|
Complications
Necrotizing Enterocolitis |
intesitnal perforation
peritonitis abdominal erythema shock |
|
|
Diagnosis
Lab Results Necrotizing Enterocolitis |
LABS ARE NONSPECIFIC
hyponatremia metabolic acidosis leukopenia/leukocytosis w left shift thrombocytopenia coagulopathy DIC with prolonged PT/aPTT + D-Dimer |
|
|
Diagnosis
Imaging Necrotizing Enterocolitis |
AXR (ABDOMINAL XR)
- dilated bowel loops - *pneumatosis intestinalis* - portal venous gas - abdominal free air - take serial abdominal plain films q6hrs US helps in discerning free air, areas of loculation or walled-off abscesses, bowel necrosis |
|
|
What is pneumatosis intestinalis?
|
intramural air bubbles representing gas produced by bacteria within the bowel wall
|
|
|
Surgical Indications
Necrotizing Enterocolitis |
perforation
(free air under diaphragm) worsening radiographic signs on serial abdominal plain films |
|
|
Surgical Procedure
Necrotizing Enterocolitis |
ileostomy with mucous fistula
reanastomosis later |
|
|
MEDICAL MANAGEMENT
Necrotizing Enterocolitis |
NPO
orogastric tube for gastric decompression fluids lytes TPN IV abx |
|
|
Complications
Necrotizing Enterocolitis |
intestinal strictures
short-bowel syndrome |
|
|
What is short-bowel syndrome?
|
a malabsorption disorder caused by the surgical removal of the small intestine
sx usually do not develop unless more than 2/3 of short bowel are removed some cases are congenital short bowel, you're born with it |
|
|
What is pathognomonic for NEC in neonates?
|
pneumatosis intestinalis on plain films
|
|
|
Bruton's agammaglobulinemia
Mode of Inheritance and Patient Population |
X-linked recessive B-cell deficiency
found only in boys |
|
|
Bruton's agammaglobulinemia
Clinical presentation and When do sx begin? |
recurrent sinopulmonary, GI adn UTIs with encapsulated organisms
after 6 mo of age (when maternal IgG -- transferred transplacentally -- is no longer active) |
|
|
Bruton's agammaglobulinemia
What is the infection risk? |
encapsulated:
Pseudomonas S pneumoniae Haemophilus infections usually happen after 6 mo of age |
|
|
Bruton's agammaglobulinemia
How do you diagnose? |
get quantitative immunoglobulin levels:
- if low, confirm with B and T cell subsets (B cells are absent; T cells are often high) - absent tonsils and other lymphoid tissue |
|
|
Bruton's agammaglobulinemia
Tx |
IVIG
prophylactic abx |
|
|
Common variable immunodeficiency (CVID)
Give a brief description |
combined B and T cell defect
all Ig levels are low (20s and 30s) normal B-cell numbers decreased plasma cells |
|
|
Common variable immunodeficiency (CVID)
When do sx appear? |
around 15-35 yo
|
|
|
Common variable immunodeficiency (CVID)
What infections are these pts at risk of? |
increased pyogenic upper and lower respiratory infections
|
|
|
Common variable immunodeficiency (CVID)
What other diseases are these pts at risk of developing? |
increased risk of lymphoma and autoimmune disease
|
|
|
Common variable immunodeficiency (CVID)
Diagnosis |
get quantitative Ig levels
confirm with B adn T cell subsets |
|
|
Common variable immunodeficiency (CVID)
Tx |
IVIG
|
|
|
IgA Deficiency
Give a brief description |
the most common immunodeficiency
decreased IgA only |
|
|
IgA Deficiency
Clinical Presentation |
usually asymptomatic
(this is a mild disease) may develop recurrent respiratory or GI infections |
|
|
IgA Deficiency
What is anaphylactic transfusion reaction? |
recipient IgE/IgG antibodies directed against IgA
leads to hypotension and shock (ie anaphylactic) |
|
|
IgA Deficiency
Diagnosis |
quantitative IgA
treat infections |
|
|
IgA Deficiency
Tx |
DO NOT GIVE IVIG
(it can lead to production of anti-IgG antibodies) |
|
|
Thymic aplasia
(DiGeorge syndrome) Clinical Presentation and age at onset of sx |
SX
tetany (secondary to hypocalcemia) ONSET first few days of life |
|
|
Thymic aplasia
(DiGeorge syndrome) Increased infection risk of what type? |
increased infections with:
viruses fungi Pneumocystis jiroveci PNA |
|
|
Thymic aplasia
(DiGeorge syndrome) Chest X-Ray Findings |
absent thymic shadow
|
|
|
Thymic aplasia
(DiGeorge syndrome) Diagnosis |
get absolute lymphcyte count
(CBC with% --> low in these pts) mitogen stimulation response delayed hypersensitivity skin testing |
|
|
Thymic aplasia
(DiGeorge syndrome) What is the mitogen stimulation response? |
in patients with no thymus, there are no T-cells, and therefore no response to mitogens
if there is no response, we categorize this as complete DiGeorge syndrome on the other hand, some patients may have some remnant thymic tissue or ectopic thymus tissue and may respond to mitogen and release T cells |
|
|
Thymic aplasia
(DiGeorge syndrome) Describe the delayed hypersensitivity response in this disease? |
patients have no T cells and therefore have no delayed hypersensitivity response
|
|
|
Thymic aplasia
(DiGeorge syndrome) Tx |
bone marrow transplant
IVIG for antibody deficiency PCP ppx ALTERNATIVE thymus transplantation |
|
|
QUICK REVIEW
B-cells make immunoglobulins that are responsible for immunity against what? |
extracellular bacteria
|
|
|
QUICK REVIEW
T cells are responsible for immunity against what? |
intracellular bacteria
viruses fungi |
|
|
Ataxia-telangiectasia
What causes this? |
a DNA repair defect
|
|
|
Ataxia-telangiectasia
Clinical Presentation |
cerebellar ataxia
oculocutaneous telangiectasias |
|
|
Ataxia-telangiectasia
Predisposes to increased risk for what? |
malignancies:
non-Hodgkin's lymphoma leukemia gastric carcinoma |
|
|
Ataxia-telangiectasia
Diagnosis is based on what clinical features? |
MORE OF A CLINICAL DIAGNOSIS
ataxia abnormal control of eye mvmt postural instability telangiectasias |
|
|
Ataxia-telangiectasia
Tx |
no specific tx
may require IVIG depending on severity of Ig deficiency |
|
|
What is ataxia?
|
poor coordination
lack of voluntary muscle coordination |
|
|
What is telangiectasia?
|
small dilated blood vessels near the surface of the skin or mucous membranes
looks like a red spider web |
|
|
Severe combined immunodeficiency
(SCID) Briefly describe what the cause of this disease is. |
severe lack of B and T cells due to a defect in stem cell maturation and decreased adenosine deaminase
|
|
|
Severe combined immunodeficiency
(SCID) Why is this also called the "bubble boy disease"? |
bc children are confined to an isolated, sterile environment
|
|
|
Severe combined immunodeficiency
(SCID) Predisposes to increased infection from what? |
severe, frequent infections with:
bacteria candidiasis opportunistic |
|
|
Severe combined immunodeficiency
(SCID) Tx |
bone marrow or stem cell transplant
IVIG for antibody deficiency PCP ppx |
|
|
Wiskott-Aldrich Syndrome
Mode of Inheritance |
X-linked recessive disorder
seen only in males |
|
|
Wiskott-Aldrich Syndrome
When do sx begin? |
at birth
|
|
|
Wiskott-Aldrich Syndrome
Classical Clinical Presentation |
bleeding
eczema recurrent otitis media |
|
|
Wiskott-Aldrich Syndrome
Quantitative Immunoglobulin and Platelet Levels |
increased IgE/IgA
decreased IgM thrombocytopenia |
|
|
Wiskott-Aldrich Syndrome
Mnemonic WIPE |
Wiskoktt-Aldrich
Infections Purpura (thrombocytopenic) Eczema |
|
|
Wiskott-Aldrich Syndrome
Patients are at increased risk of what malignancies? |
lymphoma/leukemia
|
|
|
Wiskott-Aldrich Syndrome
Patients are at increased risk of what infections? |
S pneumoniae
S aureus H influenzae type b (encapsulated; bc of decreased IgM) |
|
|
What is atopy? Or atopic disorders?
|
someone who is hyperallergic
usually hereditary SX eczema (atopic dermatitis) allergic rhinits (hay fever) allergic conjunctivitis allergic asthma sometimes food allergies |
|
|
Wiskott-Aldrich Syndrome
Tx |
supportive
(IVIG and abx) SEVERE INFECTIONS bone marrow transplantation |
|
|
Wiskott-Aldrich Syndrome
Life Expectancy |
rarely survive to adulthood
|
|
|
Chronic Granulomatous Disease
Mode of Inheritance |
X-linked (2/3)
AR (1/3) |
|
|
Chronic Granulomatous Disease
Whats the mechanism behind this disease? |
defected NADPH oxidase means deficient superoxide production by PMNs and macrophages
can engulf bacteria but cannot kills it |
|
|
Chronic Granulomatous Disease
Clinical Presentation |
chronic skin, lymph node, pulmonary, GI and urinary tract infections
osteomyelitis hepatitis lympadenopathy granulomas of the skin and GI/GU tracts |
|
|
Chronic Granulomatous Disease
Labs |
anema
hypergammaglobulinemia |
|
|
Chronic Granulomatous Disease
Increased risk of infections to what? |
catalase + organisms:
S aureus E coli Candida Klebsiella Pseudomonas Aspergillus |
|
|
Chronic Granulomatous Disease
Diagnosis |
nitroblue tetrazolium test
diagnostic for CGD absolute neutrophil count with neutrophil assays |
|
|
How do you interpret the nitroblue tetrazolium test?
|
it assesses a cell's viability by its redox potential
the higher the blue score, the better the cell is at making reactive oxygen species to kill bacteria |
|
|
Chronic Granulomatous Disease
Tx |
daily TMP-SMX
IFN-gamma can decrease the incidence of serious infection NEWER THERAPIES bone marrow transplantation and gene therapy |
|
|
Leukocyte Adhesion Deficiency
Describe the defect |
defect in the chemotaxis of leukocytes
|
|
|
Leukocyte Adhesion Deficiency
Clinical Presentation |
recurrent skin, mucosal, and pulmonary infections
|
|
|
Leukocyte Adhesion Deficiency
How does this present in newborns? |
omphalitis
(infection of the umbilical cord stump) delayed separation of the umbilical cords |
|
|
Leukocyte Adhesion Deficiency
How do wounds appear in pts with this disease? |
no pus with minimal inflammation
(due to a chemotaxis defect) |
|
|
Leukocyte Adhesion Deficiency
Diagnosis |
extremely high levels of neutrophils because they cannot leave the blood vessel
ie HIGH WHITE COUNT |
|
|
Leukocyte Adhesion Deficiency
Tx |
bone marrow transplantation is curative
|
|
|
Chediak-Higashi syndrome
Mode of Inheritance |
AR
|
|
|
Chediak-Higashi syndrome
What is the defect? |
defect in neutrophil chemotaxis / microtubule polymerizationi
|
|
|
Chediak-Higashi syndrome
Clinical Presentation |
partial oculocutaneous albinism
peripheral neuropathy neutropenia |
|
|
What is oculocutaneous albinism?
|
pigmentation problem
results in fair skin, hair and eyes (ie white hair) greatly increases the risk of having skin cancer |
|
|
Chediak-Higashi syndrome
At increased risk of what kind of infections? |
pyogenic infections:
S pyogenes S aureus Pseudomonas |
|
|
Chediak-Higashi syndrome
Diagnosis |
bone marrow smears:
look for giant granules in neutrophils |
|
|
Chediak-Higashi syndrome
Tx |
bone marrow transplantation
|
|
|
Job's syndrome
What is the defect? |
defect in neutrophil chemotaxis
|
|
|
Job's syndrome
Mnemonic FATED |
Coarse Facies
Abscesses (S aureus) Retained primary Teeth Hype-IgE (eosinophilia) Dermataologic (severe eczema) |
|
|
Job's syndrome
Increased risk of what infections? |
recurrent S aureus infections and abscesses
|
|
|
Job's syndrome
Tx |
penicillinase-resistant abx
IVIG |
|
|
C1 esterase deficiency
(hereditary angioedema) Mode of Inheritance |
AD
|
|
|
C1 esterase deficiency
(hereditary angioedema) What is the defect? |
deficiency of C1 inhibitor
|
|
|
C1 esterase deficiency
(hereditary angioedema) Clinical Presentation |
airway edema
recurrent angioedema lasting 2-72 hrs provoked by stress / trauma can lead to life-threatening |
|
|
C1 esterase deficiency
(hereditary angioedema) Diagnosis |
Total hemolytic complement (CH50) to assess quantity and function of complement
*decreased* |
|
|
C1 esterase deficiency
(hereditary angioedema) Tx |
purified C1 esterase
FFP (bc it contains C1-INH) |
|
|
Terminal complement deficiency
(C5-C9) What is the defect? |
inability to form membrane attack complex (MAC)
|
|
|
Terminal complement deficiency
(C5-C9) Increased risk of what infections? |
recurrent:
Neisseria (meningococcal or gonococcal) |
|
|
Terminal complement deficiency
(C5-C9) What other conditions can this cause? |
lupus
glomerulonephritis |
|
|
Terminal complement deficiency
(C5-C9) Tx |
meningococcal vaccine
abx |
|
|
Do not confuse bruton's agammaglobinulimema with transient hypogammaglobinulinemia of infancy.
How do you tell the difference? |
SIMILARITIES
increased susceptibility to infections at 6 mo of age DIFFERENCES B cells are decreased in Bruton's, whereas those in THI are normal |
|
|
How do you tell the difference between Bruton's and CVID? Both have similar sx.
|
Brutons is found in males around 6 mo of age
CVID is seen in older males and females 15-35 yo and sx are less severe |
|
|
Difference between when onset of sx occur between T and B cell deficiencies.
|
T cell deficiencies occur earlier than B cell
typically around 1-3 mo old |
|
|
Name 3 characteristics of phagocyte deficiencies.
|
1 - mucous membrane infections
2 - abscesses 3 - poor wound healing |
|
|
Complement deficiencies are found in children with what condition?
|
congenital asplenia or splenic dysfunction (ie sickle cell disease)
|
|
|
Untreated Kawasaki disease can lead to what?
|
coronary aneurysms
MI |
|
|
80% of patients with Kawasaki disease are what age?
|
< 5 yo
|
|
|
Kawasaki Disease
3 Phases Describe Phase 1 - Acute Phase - how long it lasts - what are the sx |
lasts for 1-2 weeks
SX F for 5+ days, plus 4 more from this list: - b/l, nonexudative, painless conjunctivitis sparing the limbic area - a polymorphous rash primarily truncal - cervical lymphadenopathy often painful and *unilateral*, with at least 1 node > 1.5 cm - diffuse mucous membrane erythema (eg strawberry tongue); dry, red, chapped lips - erythema of the palms and soles; indurative edema of the hands and feet; late desquamation of the fingertips - other: sterile pyuria, gallbladder hydrops, hepatitis, arthritis |
|
|
Kawasaki Disease
3 Phases Describe Phase 2 - SubAcute Phase - how long it lasts - what are the sx |
lasts for an additional 2-3 weeks
thrombocytosis elevated ESR coronary artery aneurysms |
|
|
Kawasaki Disease
3 Phases Describe Phase 3 - Chronic Phase - when does the chronic phase start - how long does it last |
begins when all clinical sx have disappeared
lasts until ESR returns to baseline |
|
|
Kawasaki Disease
Diagnosis |
echo at time of diagnosis to assess coronary artery aneurysms
|
|
|
Kawasaki Disease
Tx |
high-dose ASA
for inflammation and fever IVIG prevent aneurysms corticosteroids if IVIG refractory low-dose ASA for 6 weeks +coronary aneurysms+ chronic anticoagulation with ASA and other antiplatelets |
|
|
Kawasaki Disease
Mnemonic CRASH and BURN |
Conjunctivitis
Rash Adenopathy (unilateral) Strawberry tongue Hands and feet (red, swollen, flaky skin) BURN (fever > 40C for 5 days) |
|
|
Kawasaki disease and scarlet fever may both present with "strawberry tongue", rash, desquamation of the hands and feet, and erythema of the mucous membranes.
So how do you tell the difference clinically? |
children with scarlet fever have normal lips and no conjunctivitis
|
|
|
Juvenile Idiopathic Arthritis
also known as what? |
juvenile rheumatoid arthritis
|
|
|
Juvenile Idiopathic Arthritis
Clinical Presentation |
"morning stiffness"
gradual loss of motion present for 6 weeks in a pt < 16 yo |
|
|
Juvenile Idiopathic Arthritis
There are 3 basic form. What is pauciarticular (oligoarthritis)? |
this is the most common form
affects 4 or fewer joints (usually weight-bearing) ANA+ RF- involves young females +uveitis (requires slit-lamp exam) NO SYSTEMIC SX |
|
|
Juvenile Idiopathic Arthritis
There are 3 basic form. What is the polyarthritis form? |
5 or more joints
symmetric RF+ is rare (indicates severe disease) RARELY HAVE SYSTEMIC SX |
|
|
Juvenile Idiopathic Arthritis
There are 3 basic form. What is the systemic-onset (Still's Disease) form? |
recurrent high fever
> 39C HSM salmon-colored macular rash RF- and ANA- |
|
|
Juvenile Idiopathic Arthritis
Tx |
NSAIDs
strengthening exercises corticosteroids for carditis 2ND LINE AGENTS immunosuppressive meds (methotrexate, anti-TNF agents like etancercept) |
|
|
Acute Otitis Media
Common Pathogens |
S pneumonia
nontypable H influenzae Moraxella catarrhalis VIRUSES Influenza A RSV Parainfluenza |
|
|
Acute Otitis Media
Clinical Presentation |
F
ear pain crying irritability difficulty feeding difficulty sleeping vomiting diarrhea |
|
|
Acute Otitis Media
Whats one thing children do when they have this? |
tug on their ears
|
|
|
Acute Otitis Media
Diagnosis (4 things on otoscopic exam) |
otoscopic exam
erythematous TMs bulging or retraction of the TM loss of TM light reflex decreased TM mobility (test with an insufflator bulb) |
|
|
Acute Otitis Media
Tx |
high-dose amoxicillin
(80-90 mg/kg/day) x10 days RESISTANT CASES amoxicillin/clavulanic acid |
|
|
Acute Otitis Media
Complications |
TM performation
mastoiditis meningitis cholesteatomas chronic OM hearing loss --> leading to speech and language delay (if recurrent) |
|
|
Acute Otitis Media
Tx for Chronic OM |
tympanostomy tubes
6 mo to 2 years tube inserted into the TM to prevent fluid accumulation |
|
|
What is bronchiolitis?
|
acute inflammation of the small airways
|
|
|
Patient population of bronchiolitis.
|
infants and children < 2 yo
fall and winter mostly |
|
|
What is the most common cause of bronchiolitis?
|
*RSV*
OTHERS parainfluenza influenza metapneumovirus |
|
|
Risk factors for severe RSV.
|
age < 6 mo
males prematurity heart/lung disease immunodeficiency |
|
|
Bronchiolitis
Clinical Presentation |
low-grade F
rhinorrhea cough apnea (young infants) |
|
|
Bronchiolitis
When do sx generally peak? |
by day 3 or 4
|
|
|
Bronchiolitis
Physical Exam |
tachypnea
wheezing intercostal retractions crackles prolonged expiration hyperresonance to percussion |
|
|
Bronchiolitis
What is the earliest and most sensitive vital sign change? |
increased respiratory rate
|
|
|
Bronchiolitis
Diagnosis |
clinical diagnosis
CXR r/o PNA hyperinflation of lungs flat diaphragms interstitial infiltrates atelectasis |
|
|
Bronchiolitis
What is a highly sensitive and specific test for RSV bronchiolitis? |
nasopharyngeal aspirate to test for RSV
has little effect on management tx infants for bronchiolitis whether it comes back + for RSV or not |
|
|
Bronchiolitis
Outpatient Tx |
primarily supportive
fluids nebulizers |
|
|
Bronchiolitis
Inpatient Tx |
contact isolation
hydration O2 trial of aerosolized albuterol continue if effective corticosteroids are not indicated |
|
|
Bronchiolitis
Should you tx with ribavirin? |
this is an antivirual drug that has a controversial role in bronchiolitis tx
used in high-risk infants with underlying heart, lung, or immune disease |
|
|
Bronchiolitis
RSV PPX |
injectable poly or monoclonal antibodies
RespiGam Synagis do this in winter months for high-risk patients < 2 yo or those with hx of prematurity, chronic lung disease or congenital heart disease |
|
|
Bronchiolitis
Complications |
respiratory failure
can be fatal |
|
|
What is croup?
What other name does it go by? |
laryngo-tracheo-bronchitis
acute viral inflammation of the larynx (esp the subglottic space) |
|
|
What causes croup?
|
parainfluenza type 1, 2, 3
1 is most common RSV influenza adenovirus bacterial superinfection causes tracheitis |
|
|
CROUP
Clinical Presentation |
prodomal URI sx, followed by:
low-grade F mild dyspnea inspiratory stridor hoarse voice *barking cough* (usually at night) |
|
|
CROUP
Diagnosis |
clinical impression
based on degree of inspiratory stridor and respiratory distress |
|
|
CROUP
AP Neck Film Findings |
"steeple sign" from subglottic narrowing
this finding is neither sensitive or specific |
|
|
CROUP
What is steeple sign? |
it is an inverted "V" shape on AP neck film
it indicates subglottic tracheal narrowing |
|
|
CROUP
Tx Mild Cases (Outpatient) |
cool mist therapy
fluids |
|
|
CROUP
Tx Moderate Cases |
O2
oral/IM corticosteroids nebulized racemic epinephrine |
|
|
CROUP
Tx Severe Cases |
SEVERE MEANS
respiratory distress at rest inspiratory stridor Hospitalize nebulized racemic epinephrine |
|
|
What are causes of epiglottitis?
|
prior to immunization, Hib
NOW Streptococcus species nontypable H influenzae viruses |
|
|
Epiglottitis
Clinical Presentation |
acute-onset high F (39-40)
dysphagia drooling muffled voice inspiratory retractions cyanosis soft stridor |
|
|
Epiglottitis
Physical Exam |
pts sit with neck hyperextended and the chin protruding
"sniffing dog position" lean forward in a "tripod" position to maximize air entry |
|
|
Epiglottitis
Complications if left untreated |
life-threatening
airway obstruction respiratory arrest |
|
|
Epiglottitis
Diagnosis |
Clinical Impression
In light of potential laryngospasm and airway compromise, DO NOT examine the throat unless an anesthesiologist or otolaryngologist is present |
|
|
Epiglottitis
Definitive Diagnosis |
direct fiberoptic visualization of a cherry-red swollen epiglottis and arytenoids
|
|
|
Epiglottitis
Lateral XR Findings |
swollen epiglottis obliterating the valleculae
"thumbprint sign" |
|
|
Epiglottitis
Tx |
true emergency!
secure the airway before a definitive diagnosis can be made - endotracheal intubation - tracheostomy THEN GIVE IV ABX (CTX or Cefuroxime) |
|
|
Croup
Epiglottitis Tracheitis Which one presents with stridor the most? |
Croup by far
80% have stridor |
|
|
Most common pathogen in:
Croup |
Parainfluenza virus
|
|
|
Most common pathogen in:
Epiglottitis |
H influenzae
|
|
|
Most common pathogen in:
Tracheitis |
S aureus
commonly follows viral URI |
|
|
Fever Severity
Croup Epiglottitis Tracheitis |
Croup
Low Grade Epiglottitis High Grade Tracheitis Intermediate Grade |
|
|
Major Sx
Croup |
barking cough
|
|
|
Major Sx
Epiglottitis |
respiratory distress
toxic appearance inspiratory stridor drooling |
|
|
Which one responds to racemic epinephrine?
|
Croup
the stridor improves |
|
|
Most common cause of bacterial meningitis in neonates.
|
GBS
Listeria E coli |
|
|
Most common cause of bacterial meningitis in infants/children.
|
S pneumoniae
N meningitidis H influenzae |
|
|
Most common cause of viral meningitis in children of all ages.
|
Enteroviruses
|
|
|
Clinical presentation of bacterial meningitis.
|
HA
F nuchal rigidity |
|
|
Clinical presentation of viral meningitis.
|
preceded by a prodromal illness:
F sore throat fatigue |
|
|
Physical Examination
List two manuevers that suggest meningitis. |
Kernig's sign
hurts to straighten the leg when the leg is flexed at the hip Brudzinski's sign pain with passive neck flexion |
|
|
Other physical exam findings in meningitis.
|
INCREASED ICP
papilledema CN palsies petechial rash N meningitidis |
|
|
Other physical exam findings in meningitis in neonates.
|
poor tone
bulging fontanelle vomiting |
|
|
Diagnosis
Meningitis |
Head CT to r/o increased ICP
(risk of brainstem herniation) LP |
|
|
Tx for Neonates
Meningitis |
ampicillin and cefotaxime
or gentamicin acyclovir for herpes encephalitis (or if mother had HSV lesions at time of birth) |
|
|
Tx for Older Children
Meningitis |
CTX and Vanco
|
|
|
Retropharyngeal Abscess vs Peritonsillar Abscess
Which one affects the age group > 10 years of age? |
peritonsillar abscess
|
|
|
Retropharyngeal Abscess vs Peritonsillar Abscess
What is the age group affected in retro? |
6 mo to 6 yo
|
|
|
What causes retropharyngeal abscess?
|
**Group A strep**
S aureus Bacteroides |
|
|
What causes peritonsillar abscess?
|
**Group A strep**
S aureus S pneumoniae anaerobes |
|
|
Retropharyngeal Abscess
Clinical Presentation |
*acute-onset high fever*
sore throat muffled "hot potato" voice trismus drooling |
|
|
Retropharyngeal Abscess
Physical Exam |
cervical lymphadenopathy
mass may be seen in the posterior pharyngeal wall on visual inspection |
|
|
What is trismus?
|
inability to open the mouth
|
|
|
Peritonsillar Abscess
Clinical Presentation |
sore throat
"hot potato" voice trismus drooling |
|
|
Peritonsillar Abscess
Physical Exam |
uvula displaced to opposite side
|
|
|
Preferred position
Retropharyngeal Abscess |
supine with neck extended
(sitting up or flexing neck worsens sx) |
|
|
Diagnosis
Retropharyngeal Abscess |
lateral XR
Contrast CT helps differentiate btw abscess from cellulitis |
|
|
Diagnosis
Peritonsillar Abscess |
usually clinical
|
|
|
Tx
Retropharyngeal Abscess |
aspiration or I&D
abx |
|
|
Tx
Peritonsillar Abscess |
I&D
+/- tonsillectomy abx |
|
|
Why is it harder to recognize meningitis in neonates and young children?
|
they rarely have meningeal signs on exam
|
|
|
Why should you avoid giving ceftriaxone to neonates for meningitis?
|
risk of biliary sludging and kernicterus
|
|
|
What is pertussis?
(whooping cough) |
highly infectious form of bronchitis
|
|
|
What causes pertussis?
|
gram negative bacillus
Bordetella pertussis |
|
|
What vaccine protects against pertussis?
How long does it last? |
DTaP
given in 5 doses as a child immunity dies off by adolescence |
|
|
Who are the primary reservoirs for pertussis?
|
adolescents and young adults
|
|
|
How is pertussis transmitted?
|
aerosol droplets
|
|
|
Describe the 3 stages of pertussis.
|
1 - catarrhal
mild URI sx lasts 1-2 weeks 2 - paroxysmal paroxysms of cough with inspiratory whoop and posttussive emesis lasts 2-3 months 3 - convalescent sx wane |
|
|
Which stage of pertussis is most contagious?
|
catarrhal
(first stage) |
|
|
Which stage do patients usually present to the doctors office?
|
paroxysmal
(second stage - they've already been spreading it) |
|
|
Classic presentation of pertussis in an infant < 6 mo.
|
posttussive emesis
(vomiting after a cough) apnea |
|
|
Pertussis
Diagonsis |
GOLD STANDARD
culture LABS elevated WBC w/ lymphocytosis (> 70%) |
|
|
Pertussis
Tx |
INFANTS < 6 MO
hospitalize MEDS erythromycin x 14 days to patient and close contacts! include day-care contacts |
|
|
VIRAL EXANTHEMS
Cause Erythema infectiosum (Fifth Disease) |
Parvovirus B19
|
|
|
VIRAL EXANTHEMS
Describe Characteristics (Prodrome and Rash) Erythema infectiosum (Fifth Disease) |
PRODROME
none low-grade F or no fever RASH "slapped cheek" pruritic maculopapular erythematous rash starts on the arms and spreads to the trunk and legs worsens with F and sun exposure |
|
|
VIRAL EXANTHEMS
Complications Erythema infectiosum (Fifth Disease) |
Arthropathy
Aplastic crisis esp in children with: -- increased RBC turnover -- sickle cell anemia, hereditary spherocytosis, --decreased RBC turnover -- severe iron deficiency, anemia |
|
|
VIRAL EXANTHEMS
Congenital Infection Complications Erythema infectiosum (Fifth Disease) |
fetal hydrops
death |
|
|
What is hydrops fetalis?
|
edema in at least 2 compartments:
- subcutaneous tissue/scalp - pleura (pleural effusion) - pericardium (pericardial effusion) - abdomen (ascites) |
|
|
What does hydrops fetalis suggest?
|
prenatal heart failure
the edema is secondary to anemia which causes the heart to pump a greater volume of blood to deliver the same amount of oxygen |
|
|
VIRAL EXANTHEMS
Causes Measles |
Paramyxovirus
|
|
|
VIRAL EXANTHEMS
Characterstics (Prodrome and Rash) Measles |
PRODROME
low-grade fever Cough, Coryza, Conjunctivitis Koplik's spots on buccal mucosa after 1-2 days RASH erythematous maculopapular rash spreads from head to toe |
|
|
VIRAL EXANTHEMS
Complications Measles |
COMMON
OM PNA laryngothtracheitis RARE subacute sclerosing panencephalitis |
|
|
What is subacute sclerosing panencephalitis?
|
measles complication
no cure but can be managed by meds CLINICAL PRESENTATION measles before 12 asymptomatic for 6-15 yrs! then gradual, progressive psychoneurological deterioration, consisting of personality change, seizures, myoclonus, ataxia, photosensitivity, ocular abnormalities, spasticity, and coma |
|
|
VIRAL EXANTHEMS
Cause Rubella ("3-day measles") |
Rubella virus
|
|
|
VIRAL EXANTHEMS
Characteristics (Prodrome and Rash) Rubella ("3-day measles") |
PRODROME
asymptomatic or tender generalized lymphadenopathy (clue posterior auricular lymphadenopathy) RASH erythematous, tender, maculopapular rash that also spreads from head to toe |
|
|
Difference between Measles and Rubella.
|
children with rubella often have only a low-grade fever and do not appear as ill
in adolescents may see polyarthritis |
|
|
VIRAL EXANTHEMS
Complications Rubella |
encephalitis
thrombocytopenia |
|
|
VIRAL EXANTHEMS
Congenital Manifestations Rubella |
congenital anomalies:
PDA deafness cataracts MR |
|
|
VIRAL EXANTHEMS
Cause Roseola infantum |
HHV-6 and -7
|
|
|
VIRAL EXANTHEMS
Characteristics (Prodrome and Rash) Roseola infantum |
PRODROME
acute onset of high fever > 40C no other sx for 3-4 days RASH maculopapular rash appears as fever breaks begins on trunk and quickly spreads to th face and extremities lasts < 24 hrs |
|
|
VIRAL EXANTHEMS
Cause Varicella (Chickenpox) |
varicella-zoster virus (VZV)
|
|
|
VIRAL EXANTHEMS
Characteristics (Prodrome and Rash) Varicella |
PRODROME
mild fever anorexia malaise (all precede the rash by 24 hrs) RASH generalized, pruritic, "teardrop" vesicular periphery lesions at different stages of healing appears on face and spreads to rest of body, spares palms and soles contagious from 24 hrs before eruption until lesions crust over |
|
|
VIRAL EXANTHEMS
Complications Varicella |
progressive varicella with meningoencephalitis, pneumonia and hepatitis in the immunocompromised
skin lesions may develop secondary bacterial infections Reye's syndrome (associated with ASA use) |
|
|
What is Reye's syndrome?
|
potentially fatal
(brain and liver damage) STAGE 1 rash on palms and soles F / vomiting / HA confusion STAGE 2 encephalitis / stupor hyperactive reflexes STAGE 3-5 coma sz |
|
|
VIRAL EXANTHEMS
Cause Varicella zoster |
VZV
|
|
|
VIRAL EXANTHEMS
Characteristics (Prodrome and Rash) Varicella zoster |
PRODROME
reactivation of varicella infection starts as pain along an affected sensory nerve RASH pruritic "teardrop" vesicular rash in a *dermatomal* distribution uncommon unless pt is immunocompromised |
|
|
VIRAL EXANTHEMS
Complications Varicella zoster |
encephalopathy
aseptic meningitis pneumonitis TTP guillain-barre syndrome cellulitis arthritis |
|
|
VIRAL EXANTHEMS
Cause Hand-Foot-and-Mouth disease |
Coxsackie A
|
|
|
VIRAL EXANTHEMS
Characteristics (Prodrome and Rash) Hand-Foot-and-Mouth disease |
PRODROME
F anorexia oral pain RASH oral ulcers maculopapular vesicular rash on hands and feet and sometimes on the buttocks |
|
|
What does "exanthem" mean?
|
widespread rash
|
|
|
Whats the purpose of APGAR scoring?
|
assess need for neonatal resuscitation
|
|
|
Describe APGAR scoring.
|
APGAR (0, 1, 2 in each cateogry)
taken at 1 and 5 min after birth APPEARANCE blue/pale, pink trunk, all pink PULSE 0, < 100, > 100 GRIMACE W/STIMULATION 0, grimace, grimace and cough ACTIVITY limp, some, active RESPIRATORY EFFORT 0, irregular, regular |
|
|
Describe the indication based on the APGAR scoring.
|
8-10
no resuscitation needed 4-7 possible need for resuscitation 0-3 resuscitate immediately |
|
|
In general, what two general mechanisms lead to neonatal jaundice?
|
increased hemolysis
decreased excretion |
|
|
Physiologic or Pathologic?
conjugated hyperbilirubinemia (direct) |
always pathologic
|
|
|
Physiologic or Pathologic?
unconjugated hyperbilirubinemia (indirect) |
may be physiologic or pathologic
|
|
|
What is kernicterus?
|
a complication of unconjugated hyperbilirubinemia
irreversible bilirubin deposition in the basal ganglia, pons and cerebellum occurs when > 25-30 mg/dL can be fatal |
|
|
Risk factors for kernicterus.
|
prematurity
asphyxia sepsis |
|
|
Whats the differential for conjugated hyperbilirubinemia?
|
EXTRAHEPATIC CHOLESTASIS
(biliary atresia, choledochal cysts) INTRAHEPATIC CHOLESTASIS (neonatal hepatitis, inborn errors of metabolism, TPN cholestasis) Dubin-Johnson Rotor's TORCH |
|
|
Whats the differential for unconjugated hyperbilirubinemia?
|
physiologic jaundice
hemolysis breast milk jaundice increased enterohepatic circulation (eg GI obstruction) disorders of bilirubin metabolism hemolysis sepsis Crigler-Najjar Gilbert's |
|
|
Physical Exam
Neonatal Jaundice |
signs hepatic or GI dysfunction
(abdominal distention, delayed passage of meconium, light-colored stools, dark urine) infection hemoglobinopathies (cephalohematomas, bruising, pallor, petechiae, hepatomegaly) |
|
|
Clinical Presentation
Kernicterus |
lethargy
poor feeding high-pitched cry hypertonicity sz (jaundice may follow a cephalopedal progression as bilirubin increases) |
|
|
Diagnosis
Lab Tests for Indirect Hyperbilirubinemia Neonatal Jaundice |
CBC
peripheral blood smear blood type mother/infant (for ABO or Rh incompatibility) Coomb's test bilirubin levels |
|
|
Diagnosis
Imaging studies if you suspect cholestasis Neonatal Jaundice |
US and/or HIDA scan
|
|
|
Diagnosis
Lab Tests for Direct Hyperbilirubinemia Neonatal Jaundice |
LFTs
bile acids blood cultures sweat test tests for aminoacidopathies alpha1-antitrypsin deficiency |
|
|
Diagnosis
Neonate who is jaundiced, febrile, hypotensive, and tachypneic. |
most likely sepsis
needs NICU monitoring |
|
|
Tx
Neonatal Jaundice |
treat underlying condition
(ie infection) UNOCNJUGATED HYPERBILIRUBINEMIA phototherapy (mild) exchange transfusion (severe > 20) IF PRETERM INFANT start phototherapy at a lower threshold (10-15 mg/dL) CONJUGATED phototherapy not indicated and can lead to skin bronzing |
|
|
Respiratory distress syndrome is also known as what?
|
hyaline membrane disease
|
|
|
What causes respiratory distress syndrome?
What is the pathogenesis? |
surfactant deficiency
leads to: poor lung compliance alveolar collapse atelectasis |
|
|
Risk factors for respiratory lung disease.
|
maternal DM
male gender 2nd born of twins |
|
|
Clinical Presentation
Respiratory Distress Syndrome |
presents in the first 48-72 hrs of life
usually in preterm infants |
|
|
Physical Exam
Respiratory Distress Syndrome |
RR > 60
progressive hypoxemia cyanosis nasal flaring intercostal retractions expiratory grunting |
|
|
CXR Findings
Respiratory Distress Syndrome |
ground-glass appearance
diffuse atelectasis air bronchograms |
|
|
CXR Findings
Transient tachypnea of the newborn |
retained amniotic fluid results in prominent perihilar streaking in interlobular fissues
resolves with O2 adminitration |
|
|
CXR Findings
meconium aspiration |
coarse, irregular infiltrates
hyperexpansion pneumothoraces |
|
|
Diagnosis and CXR Findings
Congenital pneumonia |
nonspecific patchy infiltrates
neutropenia tracheal aspirate gram stain |
|
|
Tx
Respiratory Distress Syndrome |
CPAP or intubation and mechanical ventilation
administer artificial surfactant |
|
|
Tx for mothers before giving birth
Respiratory Distress Syndrome |
for preterm deliveries < 30 weeks:
corticosteroids if > 30 weeks: assess need for steroids with L:S ratio and presence of phosphatidylglycerol |
|
|
How do you assess fetal lung maturity?
|
L:S ratio is a marker of fetal lung maturity
perform an amniocentesis to obtain amniotic fluid L:S > 2 means fetal lungs are mature L:S < 1.5 is not mature and has a high risk of getting RDS |
|
|
Whats another way to assess fetal lung maturity?
|
phosphatidylglycerol is found in pulmonary surfactant
do amniocentesis > 0.3 of phosphatidylglycerol indicates fetal lung maturity |
|
|
Complications
RDS |
persistent PDA
bronchopulmonary dysplasia retinopathy of prematurity barotrauma from PPV intraventricular hemorrhage NEC |
|
|
What other defects are associated with a tracheoesophageal fistula?
|
esophageal atresia
VACTERL Vertebral Anal Cardiac Tracheal Esophageal Renal Limb |
|
|
Clinical Presenation
tracheoesophageal fistula (in utero and after birth) |
polyhydramnios in utero
increased oral secretions inability to feed gagging aspiration pna respiratory distress |
|
|
Diagnosis and Confirmatory Test
tracheoesophageal fistula |
CXR showing an NG tube coiled in the esophagus identifies esophageal atresia
presence of air in the GI tract CONFIRMATION bronchopscopy |
|
|
Clinical Presentation
Congenital diaphragmatic hernia |
respiratory distress
(from pulmonary hypoplasia and pulm HTN) |
|
|
Physical Exam
Congenital diaphragmatic hernia |
bowel sounds over the left hemithorax
sunken abdomen! |
|
|
Diagnosis and Confirmatory Test
Congenital diaphragmatic hernia |
US in utero
confirmed by postnatal CXR |
|
|
What is gastroschisis?
|
herniation of the intestine only lthrough the abdominal wall next to the umbilicus (usually on the right)
usually with no sac (the GI tract is exposed!) |
|
|
Clinical Presentation
(in utero and after birth) gastroschisis |
polyhydramnios in utero
often premature |
|
|
What conditions are associated with gastroschisis?
|
GI stenoses or atresia
|
|
|
Tx
gastroschisis |
surgical emergency!
single-stage closure (possible in only 10% of cases) |
|
|
What is an omphalocele?
|
herniation of abdominal viscera through the abdominal at the umbilicus into a sac covered by peritoneum and amniotic membrane
|
|
|
Clinical Presentation
(in utero and after birth) omphalocele |
polyhydramnios in utero
often premature |
|
|
What is omphalocele also associated with?
Name one specific syndrome. |
other GI and cardiac defects
Beckwith-Wiedemann syndrome and trisomies |
|
|
Tx
omphalocele |
C-section can prevent sac rupture
if sac is intact, postopne surgical correction until the patient is fully resuscitated keep the sac covered/stable with petroleum and gauze intermittent NG suction to prevent abdominal distention |
|
|
What is duodenal atresia?
|
complete or partial failure of the duodenal lumen to recanalize during gestational weeks 8-10
|
|
|
Clinical Presentation
(in utero and after birth) duodenal atresia |
polyhydramnios in utero
bilious emesis within hours after the first feeding |
|
|
What other conditions is duodenal atresia associated with?
|
Downs and other cardiac/GI anomalies
(eg annular pancreas, malrotation, imperforate anus) |
|
|
Diagnosis
duodenal atresia |
AXRs show the "double bubble" sign (air bubbles in the stomach and duodenum) proximal to the site of atresia
|
|
|
Tx
duodenal atresia |
surgical repair
|
|
|
When is the onset of physiologic jaundice?
|
about 72 hrs after brith
|
|
|
What is the onset of pathologic jaundice?
|
in the first 24 hrs of life!
|
|
|
Bilirubin normally increases at what rate in physiologic jaundice?
|
less than 5 mg/dL/day
|
|
|
Bilirubin increases at what rate in pathologic jaundice?
|
> 0.5 mg/dL/hr
or > 6 mg/dL/day |
|
|
Peak bilirubin level in physiologic jaundice.
|
< 14-15
|
|
|
Peak bilirubin level in pathologic jaundice.
|
> 15
|
|
|
Direct bilirubin makes up what percentage of total in physiologic jaundice?
|
< 10% of total
|
|
|
Direct bilirubin makes up what percentage of total in pathologic jaundice?
|
> 10%
|
|
|
How long does it take to resolve physiologic jaundice?
|
within 1 week for term infants
2 weeks in preterm infants |
|
|
How long does it take to resolve pathologic jaundice?
|
persists beyond 1 week in term infants
> 2 weeks in preterm infants |
|
|
Is cerebral palsy inherited?
|
NO!
|
|
|
What is cerebral palsy?
|
nonhereditary and nonprogressive d/o of movement and posture
|
|
|
What causes cerebral palsy?
|
perinatal neurologic insult
in most cases though its unknown |
|
|
Risk factors for cerebral palsy?
|
low birth weight
intrauterine exposure to maternal infection prematurity perinatal asphyxia trauma brain malformation neonatal cerebral hemorrhage |
|
|
Describe the two categories of cerebral palsy.
Start with pyramidal (spastic). |
spastic paresis of any or all limbs
accounts for 75% of cases MR in 90% of cases |
|
|
Describe the two categories of cerebral palsy.
Now how about extrapyramidal (dyskinetic). |
damage to extrapyramidal tracts
abnormal mvnts worsen with stress and disappear during sleep have trouble standing, sitting or walking |
|
|
Describe the 3 subtypes of dyskinetic/extrapyramidal CP.
|
ATAXIA
difficulty coordinating purposeful mvmts CHOREOATHETOID non-smooth mvnts involuntary grimacing/tongue thrusting muscles alternate between loose/flexed DYSTONIC uncontrollable jerking, writhing, posturing |
|
|
CP may lead to other conditions in life. What are they?
(this is also how they may present) |
sz disorders
behavioral d/o hearing/vision impairment learning disabilities speech deficits |
|
|
Physical Exam
Cerebral Palsy |
affected limbs:
hyperreflexia pathologic reflexes (eg Babinski) increased tone/contractures weakness underdevelopment toe walking scissor gait hip dislocations scoliosis |
|
|
Diagnosis
Cerebral Palsy |
clinical impression
US to identify intracranial hemorrhage or structural malformations MRI is diagnostic in older children EEG for sz |
|
|
Tx
Cerebral Palsy |
no cure for CP
special ed physical therapy braces surgical release of contratures SPASTICITY diazepam dantrolene baclofen (baclofen pumps and rhizotomy may alleviate severe contractures) |
|
|
What is rhizotomy?
|
a neurosurgical procedure that selectively destroys problematic nerve roots in the spinal cord to relieve spasms
|
|
|
What is the most common presenting sx of cerebral palsy?
|
delayed motor development
|
|
|
At what ages are febrile seizures prevalent?
|
6 mo to 5 yo
|
|
|
Risk factors for febrile sz.
|
rapid rise in temp
hx of febrile sz in a close relative |
|
|
Clinical Presentation
Febrile Sz |
sz usually during onset of fever
may also be the first sign of an underlying illness (eg OM, roseola) |
|
|
What are simple febrile sz?
|
short duration < 15 min
generalized tonic-clonic sz only 1 sz in a 24-hr period high F > 39C *F onset within hrs of a sz* |
|
|
What are complex febrile sz?
|
long-duration > 1 min
can be a focal sz multiple sz in a 24 hr period *low-grade F for several days before sz onset* |
|
|
Diagnosis
Febrile Sz |
find any sources of infection
LP if suspect CNS infection r/o ICP FOR FIRST-TIME SIMPLE FEBRILE SZ: no other workup/labs are necessary |
|
|
What is the workup if febrile sz occur earlier than 6 mo?
|
if child is > 18 mo, no workup is required
but if less than 6 mo, ened a sepsis workup CBC UA blood/urine/CSF cx |
|
|
Tx
Simple Febrile Sz |
ANTIPYRETICS
acetaminophen, no ASA (risk of Reyes) *antipyretics does not reduce the recurrence of febrile sz* |
|
|
Tx
Complex Febrile Sz |
EEG
MRI chronic anticonvulsant may be necessary (eg diazepam or phenobarbital) |
|
|
What are the complications of febrile size (both simple vs complex)?
|
SIMPLE
risk of recurrence 30% in first year COMPLEX may lead to full on epilepsy developmental delay (esp if +fam hx or have an abnormal neurological exam) |
|
|
Leukemia is associated with what other conditions?
|
Trisomy 21
Fanconi's anemia prior radiation SCID congenital bone marrow failure |
|
|
Clinical Presentation
Leukemia (mostly ALL) |
abrupt in onset
initial sx are nonspecific (anorexia, fatigue) bone pain with limp refusal to bear weight fever (from neutropenia) |
|
|
Physical Exam
Leukemia (mostly ALL) |
fever (from neutropenia)
aneima ecchymoses petechiae hepatosplenomegaly |
|
|
Physical Exam if brain mets
Leukemia |
HA
vomiting papilledema |
|
|
AML can present with what type of tumor?
|
chloroma
a greenish soft-tissue tumor on the skin or spinal cord |
|
|
Diagnosis
Leukemia |
CBC
WBC can be low, normal, or high coag studies peripheral blood smear **shows high number of blasts --> lymphoblasts are found in 90% of cases** |
|
|
Confirmatory Diagnosis
Leukemia |
BONE MARROW ASPIRATE
for immunophenotyping --> TdT assay and a panel of monoclonal antibodies to T and B cell antigens) GENETIC ANALYSIS DIAGNOSTIC IF: BM is hypercellular with increased lymphoblasts!!! |
|
|
How do you r/o mets in leukemia?
|
CXR
|
|
|
Tx
Leukemia |
chemo
(induction, consolidation and maintenance phases) |
|
|
Whats a complication of chemotherapy?
|
TUMOR LYSIS SYNDROME
hyperkalemia hyperphosphatemia hyperuricemia |
|
|
Leukemia is associated with what other conditions?
|
Trisomy 21
Fanconi's anemia prior radiation SCID congenital bone marrow failure |
|
|
Clinical Presentation
Leukemia (mostly ALL) |
abrupt in onset
initial sx are nonspecific (anorexia, fatigue) bone pain with limp refusal to bear weight fever (from neutropenia) |
|
|
Physical Exam
Leukemia (mostly ALL) |
fever (from neutropenia)
aneima ecchymoses petechiae hepatosplenomegaly |
|
|
Physical Exam if brain mets
Leukemia |
HA
vomiting papilledema |
|
|
AML can present with what type of tumor?
|
chloroma
a greenish soft-tissue tumor on the skin or spinal cord |
|
|
Diagnosis
Leukemia |
CBC
WBC can be low, normal, or high coag studies peripheral blood smear **shows high number of blasts --> lymphoblasts are found in 90% of cases** |
|
|
Confirmatory Diagnosis
Leukemia |
BONE MARROW ASPIRATE
for immunophenotyping --> TdT assay and a panel of monoclonal antibodies to T and B cell antigens) GENETIC ANALYSIS DIAGNOSTIC IF: BM is hypercellular with increased lymphoblasts!!! |
|
|
How do you r/o mets in leukemia?
|
CXR
|
|
|
Tx
Leukemia |
chemo
(induction, consolidation and maintenance phases) |
|
|
Whats a complication of chemotherapy?
|
TUMOR LYSIS SYNDROME
hyperkalemia hyperphosphatemia hyperuricemia |
|
|
How do you treat tumor lysis syndrome?
|
fluids
diruetics allopurinol urine alkalinIzation reduction of phosphate intake CORTICOSTEROIDS ARE CONTRAINDICATED BC THEY CAN PRECIPITATE TUMOR LYSIS SYNDROME |
|
|
Neuroblastomas are derived from what kind of cells?
|
neural crest
|
|
|
What other conditions are associated with neuroblastomas?
|
neurofibromatosis
Hirschsprung's disease N-myc oncogene |
|
|
Clinical Presentation
Neuroblastomas |
most children at < 2 yo
> 70% have distant mets nontender abdominal mass may cross the midline Horner's syndrome HTN cord compression from a paraspinal tumor |
|
|
Physical Exam
Neuroblastomas |
50% have mets at diagonsis
SIGNS OF: bone marrow suppression proptosis hepatomegaly subcutaneous nodules opsoclonus/myoclonus |
|
|
What is opsoclonus?
|
uncontrolled eye movement
rapid, involuntary, multivectorial (horizontal and vertical), unpredictable, conjugate fast eye movements without intersaccadic intervals |
|
|
Diagnosis
Neuroblastomas |
CT
FNA of tumor histologically appears as: small, round, blue tumor cells with a characteristic rosette pattern elevated 24-hr urinary catecholamines (VMA and HVA) OTHERS CBC, LFTs, coag panel, BUN/Cr |
|
|
Tx
Neuroblastomas |
local excision
chemo radiation |
|
|
Age at which you see a wilms' tumor.
|
2-5 yo
|
|
|
What is wilms tumor associated with?
|
Beckwith-Wiedemann syndrome
Neurofibromatosis WAGR syndrome |
|
|
What is Beckwith-Wiedemann syndrome?
|
hemihypertrophy, macroglossia, visceromegaly
|
|
|
What is WAGR syndrome?
|
Wilms tumor
Aniridia Genitourinary abnorm MR |
|
|
Clinical Presentation
Wilms Tumor |
asymptomatic, nontender, smooth abdominal mass
**does not cross the midline** abdominal pain |
|
|
Physical Exam
Wilms Tumor |
F
HTN hematuria |
|
|
Diagnosis
Wilms Tumor |
CBC, BUN, Cr, UA
abdominal US to detect mass CT abdomen and chest to find mets |
|
|
Tx
Wilims Tumor |
local resection
nephrectomy chemo radiation |
|
|
Whats the embryonic origin of Ewing's sarcoma?
|
neuroectoderm
associated with chromosome 11:22 translocation |
|
|
Whats the embryonic origin of osteosarcoma?
|
osteoblasts (mesenchyme)
|
|
|
Patient population of Ewing's sarcoma.
|
Caucasian male adolescents
|
|
|
Patient population of osteosarcoma.
|
male adoelscents
|
|
|
Clinical Presentation
Ewing's Sarcoma |
local pain and swelling
SYSTEMIC SX F anorexia fatigue |
|
|
Clinical Presentation
osteosarcoma |
local pain and swelling
systemic sx are rare |
|
|
Location of Ewing's sarcoma.
|
midshaft of long bones
(femur, pelvis, fibula, humerus) |
|
|
Location of osteosarcoma.
|
metaphyses of long bones
distal femur proximal tibia proximal humerus mets to lungs in 20% |
|
|
Diagnosis
Ewing's sarcoma |
X-Ray
"onion skin" periosteal reaction leukocytosis increased ESR |
|
|
Diagnosis
osteosarcoma |
X-RAY
"sunburst" lytic bone lesion increased alk phos chest CT to r/o pulm mets |
|
|
Tx
Ewing's sarcoma |
local excision
chemo radiation |
|
|
Tx
osteosarcoma |
local excision
chemo |
|
|
What is leukocoria?
|
abnormal white reflection from the retina of the eye
|
|
|
What does leukocoria suggest?
(3 things) |
retinoblastoma
congenital cataracts retinopathy of prematurity |
|
|
PREVENTIVE CARE IN PEDIATRICS
Water should be no more than what temperature? |
< 48.8C or 120 F
|
|
|
PREVENTIVE CARE IN PEDIATRICS
How should babies sleep? |
on their backs
no stuffed animals or toys in the crib TO DECREASE SIDS |
|
|
PREVENTIVE CARE IN PEDIATRICS
Describe how car safety seats should be placed. |
they should be REAR FACING and placed in the BACK OF THE CAR
seats can face forward if child is > 1 yo or weighs > 20 lb |
|
|
PREVENTIVE CARE IN PEDIATRICS
When should solids be introduced? |
> 6 mo
introduce gradually and one at a time |
|
|
PREVENTIVE CARE IN PEDIATRICS
When should cow's milk be introduced? |
> 12 mo
|
|
|
PREVENTIVE CARE IN PEDIATRICS
When should you use ipecac syrup? |
ipecac syrup is an emetic
NOT RECOMMENDED for accidental poisoning call poison control |
|
|
Strabismus is normal in pediatrics patient up until a certain age. What age is that?
|
normal up until 3 mo
|
|
|
What are you trying to prevent when trying to treat strabismus?
|
amblyopia
suppression of retinal images in a misaligned eye leading to permanent vision loss |
|
|
When should the red reflex be checked?
|
right at birth
leukocoria is a white reflex and is abnormal |
|
|
When should hearing be screened?
|
right before discharge after birth
|
|
|
How is hearing screened?
|
otoacoustic emissions
or auditory brainstem response |
|
|
What are contraindications to vaccines in general?
|
severe allergy to a vaccine component
encephalopathy within 7 days of a prior pertussis vaccination |
|
|
What are contraindications to vaccines in IC and pregnant patients?
What exceptions can be made for HIV patients? |
AVOID LIVE VACCINES
oral polio varicella MMR HIV PATIENTS may receive MMR and varicella |
|
|
What are contraindications to the MMR and influenza vaccine?
|
allergies to eggs
|
|
|
Under what conditions should you exercise precaution when giving vaccines, but are not contraindications?
|
current illness
(with or without F) prior reactions to pertussis (F > 40.5C) shock-like state persistent crying for > 3 hrs within 48 hrs of vaccination sz within 3 days of vaccination |
|
|
What are not contraindications to vaccination?
|
mild illness
low grade F current abx therapy prematurity pneumococcal vaccine should be given to high-risk groups (sickle cell disease, splenectomy, immunodeficient) |
|
|
What is the recommended screening for lead?
|
12 and 24 mo
for patients living in high-risk areas (pre-1950s) universal screening is not recommended |
|
|
Clinical Presentation
Lead Poisoning |
irritability
HA hyperactivity or apathy anorexia *intermittent abdominal pain* constipation intermittent vomiting *peripheral neuropathy* (wrist or foot drop) |
|
|
Lead Poisoning
What are sx of acute encephalopathy? |
increased ICP
vomiting confusion sz coma |
|
|
Diagnosis
Lead Poisoning |
fingerstick test as an initial screen
serum lead level CBC / BLOOD SMEAR microcytic, hypochromic anemia basophilic stippling |
|
|
What is basophilic stippling?
|
small dots at the periphery of RBCs
|
|
|
In what conditions do you see basophilic stippling?
|
lead/arsenic poisoning
sideroblastic anemia alpha/beta thalassemia |
|
|
Tx
Leading Poisoning |
IF < 45 ug/dL AND ASYMPTOMATIC
retest at 1-3 mo remove sources of lead IF 45-69 ug/dL chelation therapy --> inpatient EDTA or outpatient oral succimer DMSA IF > 70 chelation therapy --> inpatient EDTA + BAL (IM dimercaprol) |

