![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
153 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
primary hyperparathyroidism presentation |
often presents as asymptomatic hypercalcemia found on routine testing, can present with acute symptoms, more often there is a slower onset of manifestations such as... |
|
|
|
there are 2 major groups of adrenergic receptor antagonists |
alpha blockers, which act on peripheral receptors to decrease systemic vascular resistance (used to treat catecholamine overload in pheochromocytoma, interaction between MAOis and other drugs or food cocaine intoxication, amphetamine overdose, clonidine withdrawal) ßBs, in CVD pts |
|
|
|
Differential diagnosis DDx of hypercalcaemia |
PTH-mediated: Primary hyperparathyroidism, Familial hypocalciuric hypercalcaemia, Tertiary hyperparathyroidism, Ectopic PTH production by a tumour |
PTH-independent: secretion of PTH related peptide by tumor cells, increased calcitriol, bone metastases, Granulomatous diseases, Vitamin D intox, drugs: thiazides, lithium, vit A, hyperthyroidism, immobil., vit A toxicity, CRF |
|
|
management of primary hyperparathyroidism |
Medical management: 1) Parathyroidectomy is always a valuable option (normalizes serum Ca2+ and PTH, lowers fracture risk even in asymptomatic pts) 2) in pts (older pts and those where surgery is inappropiate) oestrogen, bisphosphonates, raloxifene,and cinacalcet
options for select patients and those who do not meet parathyroidectomy guidelines include bisphosphonates and oestrogen replacement (both provide skeletal protection) and the calcimimetic cinacalcet, which can reduce serum calcium and parathyroid hormone values |
|
|
|
Markers of bone turnover |
e.g. AP, urinary hydroxyproline secretion, and urinary N-telopeptide |
|
|
|
causes of hypocalcemia |
common: VitD deficiency (UV or diet issues), VitD deficiency as a result of malabsorption, Hypoparathyroidism (surgery or autoimmune destruction), Renal disease |
rare: PTH or VitD resistance, AD hypocalcemia, hypomagnesemia, sclerotic metastases etc... |
|
|
hypocalcemia etiology (resource: MTB) |
|
others: VitD deficiency, fat malabsorption, low albumin states (total calcium decreases, however no decrease in free calcium levels) |
|
|
hypocalcemia presentation and dx |
signs of neuronal hyperexcitability in hypocalcemia:
|
EKG shows prolonged QT + arrhythmias might be present slit lamp exam: early cataracts might be visible |
|
|
etiology/causes of hypercortisolism (Cushing syndrome) |
|
|
|
|
presentation of hypercortisolism + dx |
|
1) establish dx of hypercortisolism: best initial test (BIT) is the 24h urine cortisol, alternatively 1 mg ov dexamethasone suppression test (should normally suppress morning cortisol levels)--> CAVE: false+ results 2) establish cause/source of hypercortisolim: ACTH testing = bit; once ACTH is increased and there is no dexamethasone suppression: do MRI, if MRI shows not clear picture of pituitary do a sampling of the inferior petrosal sinus |
|
|
CAVE: false+ results on 1mg ov dexamethasone suppression testing... |
depression, alcoholism, obesity |
|
|
|
effects of hypercortisolism |
hyperglycemia, hyperlipidemia, hypokalemia (anti-insulin effects and aldosterone-like effects), metabolic alkalosis (excretion of H+ ions), leukocytosis (demargination of WBCs) |
|
|
|
chronic hypoadrenalism |
aka Addison disease CAVE: acute adrenal insufficiency (AI) or adrenal crisis constitute different severities of the same disease! |
etiology: autoimmune destruction (80%), infection (TB), adrenoleukodystrohy, metastases to the adrenal glands acute disease: due to hemorrhage, surgery, sudden removal of chronic high-dose prednisone |
|
|
adrenal crisis presents typically with... |
profound hypotension, fever, confusion, coma |
dx test will show: hypoglycemia, hyponatremia, hyperkalemia, high BUN, metabolic acidosis, eosinophilia is common in hypoadrenalism |
|
|
1° hyperaldosteronism |
Primary aldosteronism (PA or Conn’ syndrome) = mc 2° form of HTN, with an est. prev. ranging between 6% and 20% in pts with resistantHTN, CAVE: aldosterone-renin ratio (ARR) for screening = BIT |
The most common form of PA are idiopathicbilateral hyperplasia (IHA) and aldosterone-producingadenoma (APA), accounting for more than 90% ofclinical cases |
|
|
TTP and HUS? |
these two diseases are often considered one and the same except for presenting symptomatology, both present with the classic pentad: microangiopathic hemolytic anemia (with schizstocytes on blood smear), RF, F, altered mental status (ams), thrombocytopenia |
CAVE: PT and PTT are normal!!! CAVE: in TTP ams is more predominant (approx. 90% of pts prresent with confusion and somnolence, only 2% of TTP pts present with RF...), whereas in HUS the predominant symptom is acute anuric RF (98%)!!! CAVE: a further clue for HUS: pts will present with exposure to |
|
|
Evan syndrome |
is the combination of autoimmune hemolytic anemia and idiopathic thrombocytopenic purpura (ITP) |
|
|
|
ITP |
immune thrombocytopenic purpura, formerly ka: idiopathic thrombocytopenic purpura Medical options for front-line drug therapy are corticosteroids, IV immunoglobulin, and IV Rh anti-D. Second and third line therapy includes monoclonal Abs and thrombopoirtin receptor agonist. |
results only in (isolated) persistent thrombocytopenia (peripheral platelet count of less than 150 x109/L) and is usually seen in a female patient with a previous viral infection or drug exposure can occur in children and adults |
|
|
ITP presentation |
Many pts with ITP are asymptomatic. Physical exam is mostly + for cutaneousmanifestations as petechiae, ecchymoses and bruising, 1/4 of pts present with epistaxis, hematuria isless frequent |
Fatal bleeding occurs in 0.9% upon initial presentation |
|
|
flumanezil |
its use in benzo overdose is controversial given the AEs (seizures and acute benzo withdrawal) |
CAVE: the only clear indication is post-anesthesia in a patient who is not on chronic benzos! |
|
|
Flumazenil |
has a very rapid onset of action after parenteral administration, and competitively antagonizes the sedating effects of a wide range of benzos (midazolam, diazepam and lorazepam) at the GABA A receptor |
|
|
|
some differentials of lower GI bleed in elderly patients beyond the sixth decade of life |
Lower gastrointestinal bleeding (LGIB) defined as bleed originating distal to the ligament of Treitz colon cancer, diverticulosis, AVM, hemorrhoids, |
|
|
|
haematochezia causes in different age groups (according to Billingham) |
adolescents and young adults: Meckel's diverticulum, IBD, Polyps adults to 60 yrs of age: Diverticula, IBD, Neoplasms adults older than 60 yrs: AVM, Diverticula, Neoplasms |
haematochezia is the passage of fresh blood through the anus |
|
|
differentials for ST-segment elevation on an ECG include the following: |
|
these drugs can precipitate an acute MI in healthy pts due to coronary vasospasm |
|
|
Mirena® |
is a levonorgestrel-releasing intrauterine system (IUD) consisting of a T-shapedpolyethylene frame (T-body) with a steroid reservoir |
indications: Mirena is indicated for intrauterine contraception for up to 5 years |
|
|
MM dx algorhythm (according to Kaplan Q bank) |
|
ddx would include: MM, MGUS, primary amyloidosis, lymphoproliferative disorders such as NHL and Waldenström's macroglobulinemia (the dx is therefore confirmed by mean sof BM!!!) |
|
|
Rett syndrome (RTT) |
a severe neurodevelopmental disease that affects approximately 1 in 10,000 live female births and is often caused by mutations in Methyl-CpG-binding protein 2(MECP2) |
|
|
|
acalculous cholecystitis |
presence of cholecystitis symptoms: F, leukocytosis, thickened gallbladder with pericholecystic fluid in the abscence of gallstones accounts for 5-10% of inc of cholecystitis |
precipitating factors: multiple blood transfusions, prolonged ventilator dependence, hypovolemia, abscence of alimentary nutrition, narcotic use |
|
|
Appropriate management of acute cholecystitis depends on the severity of disease: |
Mild acute cholecystitis is optimally treated with early laparoscopic cholecystectomy |
Moderate acute cholecystitis — which is defined by a leukocyte count >18,000 per mm3, duration >72 hours Severe acute cholecystitis is characterized by organ dysfunction, and initial conservative management with antibiotics is recommended |
|
|
Percutaneous cholecystostomy is performed on ... |
Percutaneous cholecystostomy is performed on patients who present with sepsis or when medical management alone fails in patients who are poor candidates for surgery |
|
|
|
incretins |
the 2 best studiedincretins, glucose-dependent insulinotropic polypeptide(GIP) and glucagon-like peptide-1 (GLP-1), exert their insulinotropicactions through distinct G-protein-coupled receptorshighly expressed on islet b cells |
|
|
|
thiazolidinediones (TZDs) |
= glitazones, provide no clear benefit over the other hypoglygemic medications; they are relatively contraindicated as they can cause fluid overload and precipitate CHF |
rosiglitazone and pioglitazone are oral antidiabetic agents with insulin sensitising activity for the treatment of type 2 diabetes |
|
|
nateglinide and repaglinide |
are both stimulators of insulin release in a similar manner to sulfonylureas (however have no sulfa content) |
|
|
|
alpha glucosidase inhibitors |
acarbose and miglitol are both agents that block glc absorption in the bowel; they add about a half point decrease in HbA1c |
AEs: flatus, diarrhea, abd pain |
|
|
anaphylactic reactions resulting from non-IgE-mediated mechanisms |
Exercise, aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), opiates, and radiocontrast agents can also cause anaphylaxis |
|
|
|
most common causes of IgE-mediated anaphylaxis are: |
foods, particularly, peanuts, tree nuts, shellfish and fish, cow’s milk, eggs and wheat; medications (most commonly penicillin), and natural rubber latex. |
|
|
|
Signs and symptoms anaphylaxis |
Skin: Urticaria (hives), Angioedema (swelling), Erythema (flushing), Pruritus (itching) Gastrointestinal:N/V/D/Abdominal pain |
Respiratory: Upper airway: Nasal congestion, Sneezing, hoarseness, Cough, Oropharyngeal or laryngeal edema • Lower airway: dyspnea, Bronchospasms, Wheezing, Chest tightness Neurologic:• Light-headedness• Dizziness• Confusion Oral:• Itching• Tingling or swelling of the lips, tongue or palate Cardiovascular:• Hypotension• Dizziness• Syncope• Tachycardia |
|
|
Asthma: |
a disease in which the tracheobronchal tree is hyperreactive to stimuli, resulting in variable, reversible airway obstruction |
greater incidence in men, greater incidence in african american, 50% ofcs develop by age 17 and 2/3 by age 40 |
|
|
ED tx of asthma |
BIOMES ß agonist nebulizers, ipratropium, oxygen, magnesium sulfate, epinephrine, steroids (inhibiting the late inflammatory response) |
outpatient treatment |
|
|
angioedema |
is sudden swelling of face, tongue, eyes, airway often idiopathic, may be also due to C1 esterase deficiency |
|
|
|
dx and tx hereditary angioedema |
hereditary angioedema: sudden facial swelling, stridor with absence of pruritus and urticaria (best initial test is for decreased levels of C2 and C4 + deficiency for C1 esterase) |
tx: FFP or ecallantide, long-term tx with androgens: danazol, stanazol, CAVE: ensure airway protection first!!! |
|
|
HIPEC |
hyperthermic intraperitoneal chemotherapy (hipec). |
Well-selected peritoneal surface mmalignancies (psms) patients can clearly be treated with cytoreductive surgery (crs) and hipec. |
|
|
neurogenic bladder |
The neurogenic urinary bladder is defined as a dysfunctional bladder associated with a known neurological injury, which can be spinal cord injury (SCI), multiple sclerosis (MS), spina–bifida, etc. |
widely accepted that antimuscarinics are the safest and most effective class of drugs that works for neurogenic detrusor overactivity (NDO) and that antibiotics offer best results in the treatment and prevention of UTIs |
|
|
the 2 most important hypertensive disorders of pregnancy |
Preeclampsia is defined as progressively worsening high BPin pregnancy that occurs in the setting of proteinuria (≥300 mgof protein in a 24-hour urine specimen), it maybe of early onset (before 37 weeks’ gestation) or late onset(after 37 weeks) |
CAVE: Eclampsia is preeclampsia that progresses toseizures |
|
|
complications (compl) of preeclampsia |
HELLP (hemolysis, elevated liver enzymes,or low platelets), DIC,aRF, MI, pulmonaryedema, and stroke may occur!!! |
|
|
|
Recognized risk factors for pregnancy-induced hypertension include |
obesity, age >40y , chronic HTN,personal or family history of preeclampsia or gestationalHTN, nulliparity, multiple pregnancy, preexisting vasculardisease, collagen vascular disease, diabetes, andrenal disease. |
|
|
|
treatment of HTN in pregnancy... |
The American College of Obstetricians and Gynecologistsrecommends tx of severe HTN and suggestslabetalol as 1° line tx (it recommends avoidanceof atenolol, angiotensin-converting enzyme inhibitors, andangiotensin receptor blockers) |
In addition to pharmacological control of HTN, use of magnesium sulfate for seizure prophylaxis is wellestablished and has been demonstrated in randomized trialsto decrease risk of stroke in women with severe high BP inpregnancy and eclampsia |
|
|
signs of mg toxicity in preeclampsia tx setting |
mg2 sulfate is used for seizures and 2° BP ctrl (phenytoin or diazepam for refractory cases), watch for s/s of mg toxicity!!! |
->hyporeflexia or loss of deep tendon reflexes, respiratory depression, bradydysrhythmias |
|
|
What is MELAS? |
MELAS (mitochondrial encephalomyopathy, lactic acidosis, and strokelike episodes) the most common Multisystem mitochondrial disorders that cause encephalomyopathy |
caused by a mutation in the mitochondrial DNA, with an estimated prevalence of 8 to 236 cases per 100,000 persons, it is a polygenic disorder.. |
|
|
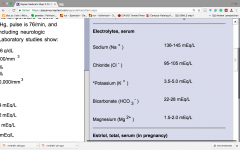
electrolyte levels (lab values) |
|
|
|
|
Neuroysticercosis |
is the mc helminthic infection of the nervous system, and a leading cause of acquired epilepsy worldwide |
occurs when humans become intermediate hosts of T. solium by ingesting its eggs from contaminated food or, most often, directly from a taenia carrier by the fecal-to-oral route |
|
|
groups of individuals suffering from Neuroysticercosis |
Almost 90% of neurocysticercosis patients diagnosed in the US and Europe are Latin American immigrants |
|
|
|
pt after MI... benefits of administration of an ACEi or ARB? |
they prevent cardiac remodeling by decreasing:
|
prescription of ACEis or ARBs in pts with CVD (post MI) with an EF < 40% is ass/w increased survival (currently class Ia recommendation) |
|
|
urticaria |
is a form of allergic reaction that causes sudden swelling of the superficial layers of the skin, can be caused by insects/medications, urticaria can also be caused by physical agents (pressure, cold, vibration) |
treatment: 1) antihistamines: hydroxizine, diphenhydramine, fexofenadine, loratidine, or cetirizine, ranitidine 2) leukotriene receptor antagonists: montekulast or zafirkulast |
|
|
allergic rhinitis presentation |
recurrent episodes of
|
|
|
|
Primary immunodeficiency (PI) diseases (PIDs) may be recognized due to |
sinopulmonary or gastrointestinal tract infections, organabscesses, autoimmunity, or systemic signs, such as fever orfailure to thrive |
sinopulmonary infection: chronic sinusitis, bronchitis, otitis media, pneumonia... |
|
|
Primary immunodeficiency disorders (PIDs) |
heterogeneous group of disorders; except for IgA deficiency, PIDs are rare; estimated prev in the US is approx 1:1200 live births |
|
|
|
->Disorders of adaptive immunity -->combined (B- and T-cell) immunodeficiency disorders (CIDs) |
Wiskott-Aldrich syndrome, Ataxia telangiectasia, DiGeorge syndrome |
|
|
|
->Disorders of innate immunity -->Phagocyte defects |
CGD, Hyper IgE syndrome, Leukocyte adhesion deficiency |
|
|
|
CVID |
common variable immunodeficiency is a heterogenous disorder characterized by markedly reduced serum concentrations of IgG, low levels of IgA and/or IgM, poor or absent responses to immunization |
CAVE: males and females are equally affected, later age of onset (>10y), ass/w recurrent sinopulmonary infections, autoimmune and granulomatous disease, GI complications and increased risk for malignancies (lymphoma and gastric cancer), also ass/w bronchiectasis |
|
|
other manifestations of CVID can include: |
|
|
|
|
clue to CVID (ddx XLA) |
CVID: decreased output of B lymphocytes, with a normal nr of B cells as well as normal amounts of lymphoid tissue such as nodes, adenoids, tonsils |
CAVE: XLA (X-linked Bruton's agammaglobulinemia is ass/w a decrease or an absence of tonsils, adenoids, or lymph nodes (Nll), spleen |
|
|
Job's syndrome |
aka hyperimmunoglobulinemia E or hyper-IgE syndrome originally characterized by recurrent cold staphylococcal abscesses, pneumonia, eczema, hyperextensibility, and extreme elevation of IgE levels |
additional features are: scoliosis, pathologic fractures, pneumatoceles, delayed dental deciduation, coronary-artery aneurysms, brain lesions, and Chiari's malformations |
|
|
Wiskott-Aldrich syndrome |
Thrombocytopenia with bleeding and bruising; eczema; recurrent bacterial and viralinfections; autoimmune disease |
|
|
|
Chronic granulomatous disease |
Severe infection; abscesses with granuloma formation |
CGD is diagnosed by tests that measure neutrophil superoxide production via the NADPH oxidase complex: the dihydrorhodamine (DHR) test has largely replaced the NBT test, the oldest and most recognized diagnostic test for CGD |
|
|
for which infections or odd combination of infections one has to look in CGD? |
|
|
|
|
physical findings specific to Grave's disease |
|
other s/s such as alopecia areata, hyperreflexia, lid lag and stare, remor, weakness are seen in any causes of hyperthyroidism |
|
|
AG |
anion gap calculated as follows: AG = serum Na - (serum bicarbonate + serum Cl-), normal 10-14 |
|
|
|
allergic rhinitis s/s (=clinical findings or clues) |
classic flare-up nasal symptoms: rhinorrhea, sneezing, eye irritation: itchy eyes conjunctival erythema, tearing pruritus |
no lymphadenopathy |
|
|
treatment allergic rhinitis |
|
in Mild, frequent or persistent(>4 weeks); OR, Moderate to severe, intermittent--->INS+/- oral histamine |
|
|
Wernicke encephalopathy (WE) |
devastating acute or subacute neurological disorder due to thiamine (Vitamin B1) with it is associated Korsakoffamnestic syndrome |
treatment consist of giving IV or IM thiamine along with mg sulfate before loading with glucose |
|
|
s/s Wernicke encephalopathy |
|
Management of acute intoxication is supportive: Thiamine, folate, IV fluids. “Banana bag” consists of 1 L of D5NS with 100 mg thiamine, 1 mg folate, and 1 amp of multivitamin (which turns bag yellow). |
|
|
Amyotrophic lateral sclerosis (ALS) aka Charcot disease |
is a fatal motor neuron disorder characterized by progressive loss of the UMNs and LMNs at the spinal or bulbar level, sporadic in 90–95% |
incidence rate remains at 2.7/100,000, The mean age of onset of ALS varies from 50 to 65 years with the median age of onset of 64 years old |
|
|
1) UMN findings in ALS include: 2) LMN findings in ALS include |
1) weakness, spasticity, hyperreflexia 2) weakness, atrophy fasciculations |
|
|
|
Syringomyelia |
involves the development of a fluid-filled cavity = syrinx within the SC, leads to progressive myelopathy can be communicating or non-communicating with the CSF pathways |
CAVE: the communicating type is ass/w Arnold-Chiari malformation, whereas the non-communicating type is ass/ SCI |
|
|
Syringobulbia |
is a condition in which the medulla is affected by the development of a fluid-filled cavity or syrinx within it s/s: dysphagia, nystagmus, pharyngeal and palatal weakness, asymmetric weakness and atrophy of the tongue and sensory loss involving primarily pain and temperature sensation (in the distribution of the trigeminal nerve) |
|
|
|
mixed connective disease |
High titers of auton-antibodies against U1 small nuclear ribonucleoprotein particle (U1-snRNP) are a sine qua non for the diagnosis of MCTD, w:m = 10:1, mcc in the 2.-3. decade of life |
additionally distinct clinical features include Raynaud's phenomenon (RP), "puffy hands," arthritis, myositis, pleuritis, pericarditis, interstitial lung disease (ILD), and pulmonary HTN (PH) CAVE ddx: hand deformities may be seen and photodistributed cutaneous eruptions may occur (ddx RA and SLE) |
|
|
CREST syndrome |
a scleroderma variant, characterized by calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, telangiectasias |
characterisitc auto-antibody see: anti-centromere autoantibody |
|
|
Achalasia |
it's a relatively rare neurodegenerative motility disorder of the E resulting in loss of peristalsis and LES relaxation particularly during swallowing due to degeneration of the myenteric nerve plexus of the oesophageal wall |
carries a risk of complications, including aspiration pneumonia and oesophageal cancer, seemingly slightly higherrates amongst females dx: Barium swallow demonstrating typical “bird’s-beak” appearance of the lower oesophageal sphincter in achalasia |
|
|
Achalasia dx |
|
Endoscopy is not accurate in thediagnosis of achalasia. However, it is still necessary to excludea carcinoma at the lower end of the oesophagus |
|
|
scenario: AIDS pts with small bowel diarrhea + negative stool studies and normal colonoscopy, ruling out CMV infection... |
Cryptosporidiosis usually caused by C. hominis and parvum, results in typical small bowel-type D/secretory = watery D with malabsorption with weakness, wl in HIV pts, more common in AIDS pts, especially those with a CD4+ T cell count of <100/mm3 |
BIOPSY will show cysts in the tips of the villi |
|
|
DOC in treating Mycoplasma pneumonia? |
is a macrolid antibiotic (azithromycin) or a new fluoroquinolone (levofloxacin) |
|
|
|
Explain the term "atypical" pneumonia |
atypical due to its gradual onset, lack of high fevers and rigors, there is nonproductive cough
|
|
|
|
Mc pathogens identified from recent studiesof mild (ambulatory) CAP were |
S. pneumoniae, M. pneumoniae,C. pneumoniae, and H. influenzae |
Mycoplasma infection was most common among patients <50y without significant comorbid conditions or abnormal VS |
|
|
ddx vaginal discharge? |
candidiasis, bacterial vaginosis (thin, greyish-white discharge with fishy odor without inflammation), trichomoniasis, physiologic discharge |
|
|
|
ICH |
Intracerebral hemorrhage ICH is defined as the spontaneous extravasation of blood into the brain parenchyma. Non-traumatic forms of ICH account for 10% to 30% of all stroke hospital admissions |
|
|
|
Acute spontaneous cerebellar hemorrhage |
ataxia, dysarthria, vomiting, dizziness, and coma |
|
|
|
schizoaffective disorder |
present with a major mood episode (major depressive or manic) with delusions or hallus for >2w |
|
|
|
Whiteley et al., 2006:
CSF opening pressure |
We prospectively recorded CSF opening pressure in 242 adults whohad a lumbar puncture with concomitant measurement of weight and height.The 95% reference interval for lumbar CSF opening pressure was 10 to 25 cmCSF
|
|
|
|
NPH |
NPH is one of the reversible causes of dementia and typically presents with: enlarged ventricles, with nomal opening pressure + triad of cognitive dysfunction (new-onset dementia), bladder incontincence and gait abnormality (ataxia) |
dx: commonly misdiagnosed, CT or MRI and then LP (will be dx and confirmative = treatment -> Miller-Fisher test) tx: VPS |
|
|
Normal results in adults |
|
consider this in relation to other findings (exam + imaging + CSF cultures) |
|
|
Chronic use of some drugs that may lead to LVH? |
anabolic steroids, tacrolimus and hydroxychloroquine, can cause LVH although they rarely result in a left ventricular wall thickness ≥1.5 cm |
|
|
|
arterial switch procedure? |
arterial switch operation has become the standard surgical procedure for treatment of complete transposition
|
|
|
|
posterior infarct |
Posterior infarction accompanies 15-20% of STEMIs, usually occurring in the context of an inferior or lateral infarction (isolated only approx. 3-11%) |
CAVE: posterior myocardium is not directly visualised by the standard 12-lead ECG
confirmation with ST elevation and Q waves in V7-9 |
|
|
how to spot a posterior infarct |
reciprocal changes of STEMI are sought in the anteroseptal leads V1-3. Posterior MI is suggested by the following changes in V1-3: |
|
|
|
BCS |
Budd-Chiari syndrome is characterized by occlusion of the hepatic venous outflow tract that may occur from the terminal branches of the hepatic venules to the level of the right atrium |
CAVE: + in the absence of right heart failure, constrictive pericarditis, or sinusoidal obstruction syndrome
|
|
|
HOCM |
formerly ka idiopathic hypertrophic subaortic stenosis (IHSS) echocardiogram will typically reveial a thickened ventricular septum + systolic anterior motion of mitral valve (SAM), further findings: brisk carotid upstroke + often exhibits bisferiens pulse + typical harsh systolic murmur (which in contrast to simple AS does not radiate into the neck in HOCM pts) |
CAVE:
|
|
|
PSC |
Primary sclerosing cholangitis (PSC) a chronic cholestatic liver disease with infl and fibr of small/large bile ducts = one of the archetypal autoimmune liver diseases alongside autoimmune hepatitis and primary biliary cirrhosis (PBC). |
IBD (worse activity than usual, backwash ileitis and rectal sparing) coexists in 60–80% of pts, with a 10x increased risk of CRC compared with the general population |
|
|
SJS vs TEN |
SJS and TEN are life-threatening, delayed type hypersensitivity reactions; there is substantial overlap in terms of clin, radiol and histopathol findings; main differentiation point is area of epidermal separation on the body surface: Epidermal separation <10% of the body surface in SJS, >30% of the body surface in TEN and in 10–30% of the body surface in SJS/TEN ovelap |
estimated mortality rate has been reported to be 1–5% for SJS and 25–30% for TEN |
|
|
presentation SJS |
usually begins with fever, sore, throat and fatigue; ulcers and other lesions begin to appear in mucous membranes conjunctivitis can be appreciated in 30% of children |
|
|
|
common etiologies/offending agents in SJS |
|
|
|
|
drugs mcc impl in TEN |

|
|
|
|
DHH |
Developmental dysplasia of the hip affects 1-3% of all newborns; it ranges from mild acetabular dysplasia with a stable hip to a frankly dislocated hip with a dysmorphic femoral head and acetabulum
|
Limited hip abduction (<60°) in 90° of hip flexion may be the most sensitive sign for detecting a dislocated hip in neonates
|
|
|
rfs for developmental hip dysplasia |
limited fetal mobility (first born infant, breech, Large for gestational age, Oligohydramnios, Breech presentation), family histor, female sex (4x more common) |
|
|
|
Carcinoid tumors def |
neuroendocrine tumors derived from enterochromaffin orKulchitsky cells, which are widely distributed in the body, inc: 2/10^5 |
mcc affected sites: GIT (about 65%), bronchopulmonary tract (BPT) (about 25%), in about 10% ofcs, the primary tumor site remains unknow overall 5-year survival rate for all carcinoid tumors(regardless of site or stage) ranges from 70%–80% Urinary 5-HIAA, the breakdown product of serotonin, hasbeen the gold standard for diagnosis |
|
|
Slipped Capital Femoral Epiphysis |
is an orthopedic emergency!!! classical clinical picture: obese or tall/lanky boy in his early teens, who is limping (cannot rotate his leg internally and when sitting his toe of the affected limb is pointin towards the unaffected limb) |
Presents with: thigh pain,referred knee pain (20%), painful limphip tenderness,limited ROM (internal rotation and abduction) of the hipflexion of the hip leads to obligatory external rotation |
|
|
rfs SCFE |
rfs: adolecence,African American,age 11-13, endocrinopathies (e.g. hypothyroidism, renal osteodystrophy) |
Complications chondrolysis, AVN (30% of uncorrected cases) of femoral head,late degenerative arthritis (may need total hip arthroplasty) |
|
|
ddx: Kaposi's sarcoma |
|
|
|
|
FSGS
|
Focal segmental glomerulosclerosis = mc glomerular cause of ESRD in the US + mcC of nephrotic syndrome in adults; Proteinuria may be in the nephrotic or subnephrotic range |
can be associated with IV drug use (heroin)HIVDMsickle cell anemi, more common in African american (typically young black male, with HTN) |
|
|
common GI disorders ass/w chest pain |
|
|
|
|
rfs for CAD |
|
|
|
|
ischemic pain (MI) described as... +ddx? |
dull or sore pain; squeezing or pressure-like sharp (knife-like) or point-like lasting for a few seconds |
3 features that tell you that the pain is not ischemic in nature: changes with respiration (pleuritic)/changes with position of the body/changes with touch to the chest wall (tenderness), i.e. ischemic pain is not tender/positional/pleuritic in nature |
|
|
characterisitcs of ischemic pain |
|
|
|
|
IBS |
irritable bowel syndrome is the mcc diagnosed gastrointestinal condition, abd pain or discomfort, with altered bowel habits, in the absence of any other disease to cause these sorts of symptoms. |
ddx: diarrhea NOT in the nights!!! |
|
|
indications for intubation of a burn patient |
any sign of airway compromise during the primary assessment: dyspnea/resp distress, hoarseness, wheezing or cough, stridor, hypoventilation, mental status changes, burns or soot inside the patients mouth or nose CAVE: even patients who are well initially can rapidly deteriorate. |
approx 20-30% of burn trauma pts have concomittant inhalation injury (mortaility increases from 3-10 to 20-30%) |
|
|
Citrobacter koseri |
= gram- bacillus which belongs to the family of Enterobacteriaceae; although rare in the newborn, it has a strong neurotropism in this age group (->meningitis/brain abscesses) |
resistant to ampicillin!!! tx: 4-6w tx with 3. or 4. gen cephalosporins AND an aminoglycoside (e.g. gentamycin and cefotaxime) |
|
|
Infantile spasms |
Infantile spasms (IS; West syndrome) is a severe form of epilepsy of early infancy |
presents with myoclonic-tonic seizures (spasms) that may be characterized by flexor, extensor, or mixed movements, a distinct EEG pattern of hypsarrhythmia, and psychomotor delay/arrest |
|
|
when asynchronous cardioversion 8defibrillation) is done? |
Vfib or pulseless VT |
|
|
|
rosacea |
characterized by facial flushing, erythema, papules and pustules, telangiectasias |
has been classified into the following 4 subtypes according to its s/s that often occur together: erythematotelangiectatic, papulopustular, phymatous and ocular. |
|
|
Chronic venous insufficiency |
altered venous hemodynamics being transmitted to the microcirculation leading to ankle edema, itching, skin changes like pigmentation, stasis dermatitis, hair loss, lipodermatosclerosis and eventually venous ulceration |
c disease entity affecting about 10-20% individuals with a significant impact on quality of life |
|
|
A-a gradient |
alveolar PO2 (PAO2) - systemic arterial PO2 (PaO2) |
normal A-a gradient = 15 mm Hg (~Age/4 +4) equilibration of O2 across alveolar gas and pulmonary capillary blood pulmonary capillary blood becomes systemic arterial blood increases with age hypoxemia → ↑ A-a gradient |
|
|
cluster headache (1) def |
reviously termed migrainous neuralgi is a 1° headache disorder classified with similar conditions known as trigeminal autonomic cephalalgias, m:f ratio varies betw 2.5:1-3.5:1.4, typically in 3.-5. decade |
typified by recurrent attacks of unilateral pain, which are very severe and usually involve the orbital or periorbital region innervated by the V1 division of CNV |
|
|
cluster headache (2) Characteristic signs and symptoms |
Characteristic s/s of activation of the cranial autonomic pathways accompany the pain on the same side: lacrimation, conjunctival injection, nasal congestion or rhinorrhoea (or both), ptosis or miosis (or both), and periorbital oedema |
†A partial Horner’s syndrome may persist to a lesser degree between attacks. |
|
|
How long does an attack last? + How often do individual attacks occur? |
attacks should last between 15 and 180 minutes, although on rare occasions they can last longer it varies from one attack every 48 hours to eight separate attacks in 24 hours, although less frequent attacks may occur at the beginning and end of bouts |
|
|
|
antimicrobials empirically used in HAP not ass/w ventilators or ICU... |
levofloxacin, ceftriaxon, ciprofloxacin, amp/sulb, piperacillin/taz, ertapenem |
pts with rfs for MDR organisms need broader coverage |
|
|
Acinetobacter baumannii |
a troublesome opportunistic pathogen in hospitals, involved in various nosocomial infections (skin and soft tissue infections, RTIs, meningitis, endocarditis, and UTIs) |
Morb/mort associated with A. baumannii infections are high (ca. 8-23% for the in-hospital and 10-43% for the ICU) |
|
|
A. baumanii tx |
1° line: imipenem 2° line: polymyxine B |
carbapenems (imipenem, meropenem, or doripenem) remain one of the most options . Unfortunately, increasing carbapenem resistance is creating therapeutic challenges, especially considering that most A. baumannii strains that are resistant to the carbapenems are also resistant to the majority of other antibiotics (except the polymyxins or tigecycline). |
|
|
the polymyxins include... |
colistin or polymyxin E and polymyxin B |
|
|
|
minoxidil
|
MOA: direct arteriolar vasodilator, CU: androgentic alopecia, severe HTN |
|
|
|
PDE5i
|
sildenafil, vardenafil, tadanafil MOA: Inhibition of PDE5 leading to prolonged SMC relaxation |
CU: erectile dysfunction, pulmonary HTN, BPH (tadanafil only) AEs: flushing, headache, dyspepsia, cyanopia (blue-tinted Vision), CAVE: risk of life-threatening Hypotension with concomittant nitrate use |
|
|
Tamsulosin
|
Alpha1 Antagonist used to treat BPH by inhibiting SMC contraction, selective for Alpha 1A, D receptors (found on prostate) vs vascular alpha1B receptors
|
|
|
|
antiandrogens
|
finasteride, flutamide, ketoconazole, spironolactone
|
|
|
|
Meniere's disease hallmarks..
|
As long as this page is open your copy/paste functionality has been disabled4.
|
|
|
|
Kawasaki disease (KD) |
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is an acute necrotising vasculitis of the medium- and small-sized vessels |
It occurs most often in babies and children, aged 6 months to 5 years and the male-to-female ratio ranges from 1.5–1.8 to 1 |
|
|
Donovaniosis (1) |
aka granuloma inguinale et: causative agent: Klebsiella granulomatis s/s: non-tender ulcerated lesion, with sharp edges and beefy-red granulation tissue (significant amount of velvety granulation tissue) and clean, Nll can become enlarged and tender |
dx: gram stain or Wright stain of tissue preparations (will reveal intracellular cystic inclusions tx: TMP-SFX, or doxy |
|
|
Donovaniosis (2) causative agent |
causative agent: intracellular gram-negative bacterium Klebsiella granulomatis (formerly known as Calymmatobacterium granulomatis) |
|
|
|
Chancroid |
definitive diagnosis of chancroid requires the identification of H. ducreyi on special culture media; No FDA-cleared PCR test for H. ducreyi is available in the US |
classic s/s: painful genital ulcer with ragged edges + tender suppurative inguinal adenopathy |
|
|
Lymphogranuloma |
Lymphogranuloma venereum (LGV) is caused by C. trachomatis serovars L1, L2, or L3 |
mc clinical manifestation of LGV among heterosexuals is tender inguinal and/or femoral lymphadenopathy that is typically unilateral CAVE: Rectal exposure in women or MSM can result in proctocolitis mimicking IBD |
|
|
spinal stenosis |
refers to as narrowing of the nerve roots in the neuranl foramina or central spinal canal |
|
|
|
symptoms commonly attributed to LSS |
classic = neurogenic claudication, also referred to as pseudoclaudication Neurogenic claudication refers to leg symptoms encompassing the buttock, groin, and anterior thigh, as well as radiation down the posterior part of the leg to the feet. In addition to pain, leg symptoms can include fatigue, heaviness, weakness and/or paresthesia, but also nocturnal leg cramps and neurogenic bladder symptoms may occur Symptoms more commonly bilateral and symmetrical. |
|
|
|
pharmacologic tx pof diabetic gastroparesis |
Metoclopramide , a dopamine D2-receptor antagonist, is the only US FDA-approved medication for the treatment of gastroparesis for no longer than a 12-week perio; alternatively: domperidone, motilin agonists, including erythromycin |
|
|
|
standard for diagnosis of gastroparesis |
Gastric emptying scintigraphy of a solid-phase meal is considered as the standard for diagnosis of gastroparesis, as it quantifies the emptying of a a physiologic caloric meal. |
|
|
|
cardiac tamponade presentation |
pulsus paradoxus (ddx RV MI), muffled/distant heart sounds, distented neck veins/JVD, venous pressure elevated, varaible degree of shock |
|
|
|
Clinical and laboratory features of HCL (prevalence). |
splenomegaly 60–70% Hepatomegaly 40–50% Abdominal lymph node enlargement 10% (By means of CT) |
Anaemia: Hb < 100 g/l 70% Thrombocytopenia 80% White blood cell count: < 5 × 109/l 65%..neutropenia, monocytopenia, hairy cells in peripheral blood |
|
|
AEs: Rifampin |
1) increases hepatic clearance of a variety of drugs (reducing effectiveness) 2) urine/tears/sweat get red-orange 3) chemical hepatitis |
|
|
|
AEs: ethambutol |
ass/w optic neuritis, can also affect red-green discrimination |
|
|
|
AEs: INH (isoniazide) |
hepatitis, PNP, sideroblastic anemia |
|
|
|
‘hungry bone syndrome’ (HBS) |
has been coined to the profound (serum calcium <2.1 mmol/l) and prolonged (longer than 4th day post-operatively) hypocalcaemia follows ollows parathyroidectomy for severe hyperparathyroidism |
|
|
|
drugs tha can cause rhabdomyolysis |
|
|
|
|
classic triad of symptoms of rhabdomyolysis |
consists of myalgia, weakness, and tea-colored urine |
|
|
|
Potential complications of rhabdomyolysis include... |
compartment syndrome and acute kidney injury as well as hypovolemia (sequestration of fluids in the muscles), DIC (late), hyperkalemia, hyperphosphatemia, hypocalcemia (early and late) |
|
|
|
postdate pregnancy |
defined as pregnancy that continues beyong 40 weeks (280 days) postconception |
|
|
|
criteria for LTOT in COPD pts |

|
|

