![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
284 Cards in this Set
- Front
- Back
|
From what embryonic lineage are keratinocytes derived (endoderm, mesoderm, ectoderm)?
|
• Ectoderm.
• Keratinocytes make up the vast majority (~90%) of cells found in the epidermis. |
|
|
What skin diseases result from filaggrin mutations?
|
• Filaggrin mutations are responsible for one of the most common forms of skin scaling diseases/icthyosis: icthyosis vulgaris, a relatively mild form of skin scaling that presents in the first year of life.
• Individuals are predisposed to atopic dermatitis (eczema) |
|
|
What is the name for the final stage of differentiation of keratinocytes, where they undergo a unique apoptosis marked by systematic destruction of the nucleus and nearly all organelles and macromoluecules beyond the cross-linked keratin bundles?
|
Corneocytes, which become enveloped by a specialized and highly cross-linked membrane (cornified envelope) and are held together by insoluble lipids (lamellar membrane)
|
|
|
What is the name of the layers of the epidermis, from top to bottom?
|
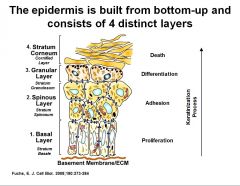
• Stratum corneum
• Stratum granulosum • Stratum Spinosum • Stratum Basale |
|
|
Which layer(s) of skin have the keratin 1/10 subtype? What about Keratin 5/14?
|
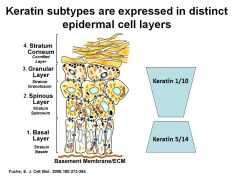
Keratin 1/10 – Granular and Spinous layers
Keratin 5/14 – Basal layer |
|
|
What causes intra-epidermal blistering?
|
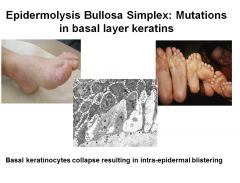
The collapse of basal keratinocytes
|
|
|
What is the function of the Langerhans cells?
|
• Langerhans cells are bone-marrow derived antigen presenting cells (APCs) that are primarily in the suprabasal layers.
• They are critical for processing and presenting antigens to T lymphocytes and thus play an important role in the immunological responsiveness of the skin. |
|
|
What is the major component of the lamina densa of the basement membrane?
|
Collagen IV
|
|
|
What is the major protein component of the dermis, and what type(s) of that component predominate?
|
Collagen, types I and III (interstitial type)
|
|
|
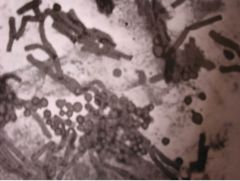
What gram positive bacterium colonizes sebaceous follicles and contributes to acne?
|
Propionibacterum acnes
|
|
|
What’s the difference between eccrine and apocrine glands?
|
Although both are sweat glands and are composed of a secretory coil and secretory duct, eccrine ducts secrete their products directly at the skin surface whereas apocrine sweat ducts are in direct communication with the hair follicle canal.
|
|
|
What is the major cell type of the hypodermis?
|
Adipocytes
|
|
|
What is the pathophysiologic basis for bullous pemphigoid?
|
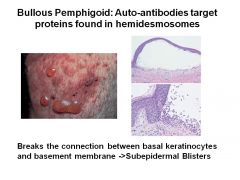
• Auto-antibodies target proteins found in hemidesmosomes.
• Breaks the connection between basal keratinocytes and basement membrane -> subepidermal blisters |
|
|
Can you describe the differential expression of desmoglein subtypes in the epidermis?
|
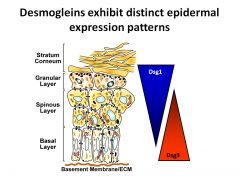
(see image)
|
|
|
Pemphigus vulgaris and foliaceus patients possess autoantibodies against distinct desmogleins. Which disease has autoantibodies against which desmogleins?
|
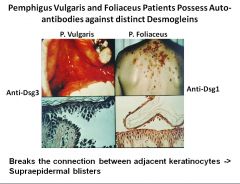
P. vulgaris – Anti-Dsg3
P. Foliaceus – Anti-Dsg1 |
|
|
The stratum corneum has been likened to “bricks and mortar,” what are the bricks, and what is the mortar?
|
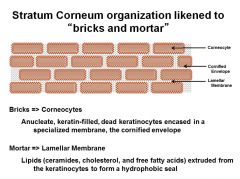
Bricks = corneocytes
Mortar = Lamellar membrane |
|

What causes Cutis Laxa?
|
Mutations in elastin gene producing amorphous elastin
|
|
|
What is the most common papulosquamous disorder?
|
Psoriasis
|
|
|
What is the pathogenesis of Lichen Planus?
|
CD8+ cells in the epidermis and dermis induce the apoptosis of keratinocytes.
|
|
|
What papulosquamous disorder has the classic “Christmas tree” pattern?
|
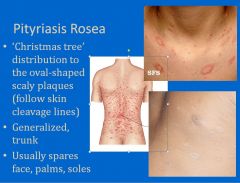
Pityriasis Rosea
|
|
|
What layer of skin does the pathology of papulosquamous disorders occur?
|
Epidermis
|
|
|
How would you characterize “inverse” psoriasis?
|
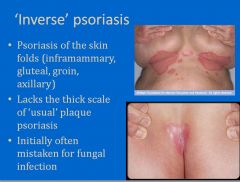
Happens in skin folds; doesn’t have the usual scales of psoriasis
|
|
|
What type of infection is Guttate psoriasis associated with?
|
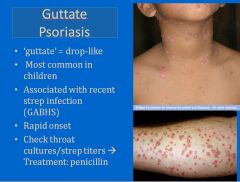
GABHS
|
|
|
What meds can trigger psoriasis?
|
• Oral steroids
• Lithium • Beta-blockers • Anti-malarials • Interferon |
|
|
What psoarisis variant is triggered by genitourinary infection and goes by the mneumonic “can’t see, can’t pee, can’t climb a tree?”
|
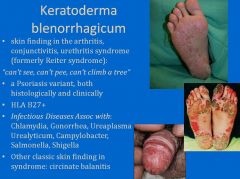
Keratoderma blenorrhagicum
|
|
|
What nail changes occur in psoriasis?
|

• Pitting
• Onycholysis (lifting up of the nail) • Onychodystrophy (thickening, discoloration) |
|
|
Which papulosquamous disorder causes “sausage digit” (i.e., one finger or toe is swollen)?
|

“Sausage finger/toe” occurs in psoariatic arthritis
|
|
|
What is the special type of phototherapy used for psoriasis?
|
Narrow band UVB (peak emission at 311-312 nm)
|
|
|
What are treatments for psoriasis?
|
• Topical corticosteroids
• Vitamin D derivatives (calcipotriene, calcitriol) • regulate maturation by affecting cell responsivness to Ca++ • Calcineurin inhibitors (tacrolimus/pimecrolimus) • good for face/genital locations • Salicylic Acid = a keratolytic • breaks up thick scale • Others: tazarotene, tars, anthralin – anthralin directly inhibits IL-6, IL-8, TNF-α but irritating and stains clothes |
|
|
What are the 4 Ps of Lichen planus?
|

1. Pruritic
2. Planar 3. Purple 4. Polygonal papules |
|
|
What are Wickham striae?
|

Wickham striae are fine, net-like lacy white lines in the mucosa of patients with Lichen planus. The mucosa is affected in 50% of Lichen planus patients.
|
|
|
What is the treatment for pityriasis rosea?
|
None needed, self limited. However, consider checking RPR (ddx syphilis)
|
|
|
Where does scabies classically appear?
|

• Webspaces of the hands and feet.
Also: • Axillae, periumbilical • Groin/genital regions • Ankles, wrists (under socks/watches) |
|
|
What is the pathogenesis of mycosis fungoides?
|

Infiltration of malignant clone of atypical T cells, mainly CD4+ helper cells into the skin
|
|

What viral infection has a skin manifestation described as “dew drops on a rose petal (vesicular rash)?”
|
Varicella Zoster Virus (Chicken pox)
|
|
|
What causes the hypopigmentation in pityriasis versicolor/tinea versicolor?
|
Production of dicarboxylic acids, including azelaic acid, which competitively inhibit tyrosinase.
|
|
|
What’s the most common cause of impetigo?
|
Staph aureus
|
|
|
What’s the Tzanck smear test commonly used for?
|
To diagnose the presence of Herpes (HSV-1,2)
|
|
|
What’s the most common viral complication of patients with atopic dermatitis?
|

Eczema herpeticum
|
|
|
Between Chickenpox (VZV) and Smallpox, which has the centripetal (trunk>extremities) vs. centrifugal (extremities>trunk) eruption pattern?
|
• Chickenpox (VZV) - centripetal (trunk>extremities)
• Small pox - centrifugal (extremities>trunk) |
|
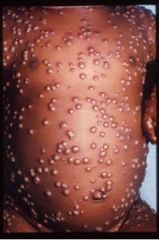
Can you describe the genome of the virus that causes this characteristic pustular rash?
|
Smallpox: DS-linear DNA virus (largest DNA virus) with an envelope
|
|

Can you describe the genome of the virus that causes this characteristic appearance and “purpuric stocking and glove eruption” in young adults? Also, what are potential complications of the disease?
|

• Parvovirus B19
• SS-linear (smallest DNA virus); no envelope • Complications: o Arthritis (adults) o Aplastic crisis (sickle cell disease) o Hydrops fetalis (RBC destruction in fetus) |
|
|
What are the 3 fungi that are most causative of tinea corporis?
|
• T. rubrum
• M. canis • T. mentagrophytes |
|
|
What fungus produces the grapelike custers of round yeast and short true hyphae/”spaghetti and meatballs” appearance in a KOH prep?
|
Malassezia furfur
|
|
|
What’s the most common cause of skin infection in babies?
|
Group B Strep
|
|
|
A mutation in what protein increases the risk of developing atopic dermatitis or atopic dermatitis and asthma?
|
Filaggrin
|
|
|
What type of allergic reaction is contact dermatitis?
|
Contact dermatitis is a delayed-type, type IV hypersensitivity reaction. (T-cell mediated inflammatory reaction characterized by erythema, scaling, xerosis, and vesiculation, occurring at the site of challenge with a contact allergen in sensitized individuals).
|
|

Can you describe the genome of the virus that causes this scaly, rough papule on the skin surface?
|
• Verruca vulgaris - wart (HPV type 2)
• DS-circular, no envelope |
|
|
Which HPV types cause condyloma acuminata (anogenital warts)?
|
• HPV 6,11
• “Low risk” |
|

What virus(es) cause hand, foot, and mouth disease?
|
• Coxsackie virus A16
• Enterovirus 71 |
|
|
What are nevi?
|
Nevi are focal proliferations of differentiated melanocytes. Atypical nevi are strong predictors of melanoma.
|
|
|
What’s the risk of the U.S. of developing melanoma?
|
1 in 58 (2007)
|
|
|
What factors determine prognosis of melanoma?
|
• Breslow’s thickness **most important**
• Mitotic rate • Ulceration of the lesion (presence associated with poor survival) • Staging |
|
|
What’s the 5-year survival rate of someone with stage IV melanoma?
|
15%
|
|
|
What are the resection margins for the different lesion sizes in melanoma?
|
• 0.5 cm for in situ lesions
• 1-2 cm for lesions up to 2 mm Breslow thickness • 2 cm for lesions thicker than 2 mm |
|
|
What’s the only chemotherapy agent approved by the FDA for melanoma treatment, and what is its response rate?
|
Dacarbazine; response rate = 25%
|
|
|
What protective effects do darker skin people have from the sun?
|
Darker people have more absorption of harmful rays by melanin
|
|
|
Where do Africans and Asians tend to get melanomas?
|

Africans and Asians get melanomas on palms and soles
|
|
|
What proportion of melanomas develop with no pre-existing lesion (de novo)?
|
70%
|
|
|
What point mutation is associated with melanoma?
|
• Point mutation in the Braf gene called V600E dimer
• Glutamate(E) is substituted for valine at position 600 in the DNA resulting in a BRAF mutation • Up-regulates the MAPK pathway and increases cell proliferation • Vemurafenib targets this mutation |
|
|
What drug for the treatment of melanoma is targeted against T regulatory cells that dampen the immune response?
|
Anti-CTLA-4 Ipilimumab is supposed to boost the immune system by targeting T regulatory cells. Note, you have to combine drugs when treating melanoma.
|
|
|
What are the spectra for UVA, UVB, and UVC?
|
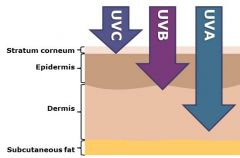
• UVA (400-320 nm)
• UVB (320-290 nm) • UVC (290-200 nm) |
|
|
Which spectrum of UV light is primarily responsible for sunburn, and delayed tanning?
|
The sunburn (redness, blisters) response is primarily mediated by UVB radiation which also causes delayed tanning.
|
|
|
Which spectrum of UV light is primarily responsible for immediate tanning?
|
UVA (and over time it’s responsible for photoaging as well).
|
|
|
What type of mutations are associated with squamous cell carcinoma (SCC) and basal cell carcinoma (BCC)?
|
Mutations in p53 are found in squamous cell carcinomas (SCCs), PTCH mutations are implicated in basal cell carcinoma (BCC).
|
|
|
How does sunlight exposure vary one’s risk for squamous cell carcinoma (SCC) versus basal cell carcinoma (BCC)?
|
Interestingly, for SCCs, the pattern of UV exposure is lifelong, chronic UV radiation; however, intermittent intense periods of burns are more important for BCC development.
|
|
|
What is the most common type of skin cancer?
|
Basal cell carcinoma (BCC) is the most common type of skin cancer. (>1M cases/yr)
|
|
|
What surgical margins are necessary to cure basal cell carcinoma(BCC)?
|
Studies have shown that margins of 4-6 mm may be required to achieve cure of BCCs.
|
|
|
What are examples of physical blockers as far as UV protection goes?
|
Physical blockers such as titanium dioxide and zinc oxide provide broad spectrum protection against UVA and UVB.
|
|
|
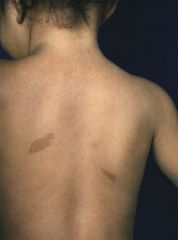
What is the treatment of choice for dermatofibrosarcoma protuberans?
|
Dermatofibrosarcoma protuberans (DFSP) is a rare fibrohistiocytic tumor of the skin. It is a locally aggressive sarcoma that even with proper treatment has a high rate of local recurrence. This tumor favors the trunk and proximal extremities and presents as a firm brown to dark red nodule that slowly grows in size. It is frequently mistaken for a keloid, hypertrophic scar or an inflamed cyst. Mohs micrographic surgery or wide resection is the treatment of choice.
|
|
|
What is the treatment of choice for Merkel cell carcinoma (MCC)?
|
Merkel cell carcinoma (MCC) is a rare neuroendocrine tumor that has a predilection for the head and neck in older adults. It presents as a rapidly growing violaceous to pink nodule. MCC is an aggressive neoplasm with high rates of both local recurrence and distant metastasis. Surgical resection is the mainstay of treatment for MCC though radiation and/or chemotherapy are frequently used as adjuncts.
|
|
|
What are the genetic syndromes that can predispose someone to non-melanoma skin cancer (NMSC)?
|
The risk of NMSC is particularly increased in patients with:
• xeroderma pigmentosum (XP) – defunct nucleotide excision repair • nevoid basal cell carcinoma syndrome (NBCCS or Gorlin syndrome) - mutation in PTCH • oculocutaneous albinism (OCA) – partial or complete loss of melanin, removing protection from photoaging and photocarcinogenesis |
|
|
What is the effect of UV exposure on the immune system and how does it contribute to the photocarcinogenesis process?
|
• UV light has both pro-inflammatory and immunosuppressive effects on the skin. Immunosuppression due to UV light involves not only skin exposed to UV but also unexposed skin. Local immunosuppressive effects involve depletion of Langerhans cell and cell function as well as activation of immunosuppressive cytokines. Systemic immunosuppressive effects involve activation of T-regulatory cells and immunosuppressive cytokines.
• Photocarcinogenesis due to UV radiation is mediated by two effects of UV radiation: DNA damage and immunosuppression. • UV exposure results in DNA damage, some of which will escape the cells’ damage response pathways – cell cycle arrest, apoptosis, DNA repair machinery, immune surveillance - and cause formation of mutations. Malignant transformation requires accumulation of mutations in key genes. |
|
|
What are the two most common biopsy methods in dermatology?
|
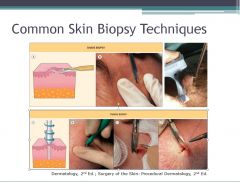
• The two most common methods of skin biopsy are a shave biopsy or punch biopsy.
• . Many methods of skin biopsy are available for sampling skin tissue. These include: shave, punch, curettage, incisional or excisional biopsies. |
|
|
What are four risk factors for NMSC development?
|
Risk factors for NMSC development include:
• UV exposure • pigmentary phenotype • exposure to ionizing radiation • chemical exposure • human papilloma virus infection (HPV) • immunosuppression, especially due to solid organ transplants o SCCs have a much greater increase in incidence in transplant patients over the general population (40-250 times more), but BCC (5-10 times more) and melanoma incidences are also increased in solid organ transplant patients. |
|
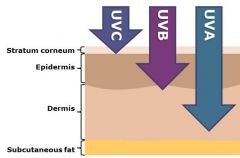
What is the mechanism of photocarcinogenesis mediated by UVA vs. UVB?
|
Direct DNA damage is thought to be mediated by UVB while UVA exposure results in indirect DNA damage mediated by reactive oxygen species.
|
|
|
Which NMSC is notable for not metastasizing often?
|
• Basal cell carcinoma (BCC)
• <0.5% metastasis |
|
|
What are typical histories for basal cell carcinoma (BCC) and squamous cell carcinoma (SCC)?
|
• BCC History:
o “Started as a pimple but didn’t go away and is getting bigger” o Bleeds or crusts, then heals, then bleeds again • SCC History: o Rough red bump or spot that continually enlarges o Can bleed or ulcerate o May appear and grow rapidly |
|
|
If a patient says that they have a flat red scaly patch in sun-exposed areas (e.g. head, neck) that comes and goes, what skin disease would you consider, and why would quick treatment be indicated?
|

• Actinic Keratoses
• Must be treated, because 1-5% can progress to squamous cell carcinoma. • Treatment: cryotherapy with liquid N2, topical medications, photodynamic therapy |
|
|
If a patient says that they have a scaly red plaque in sun-exposed areas (e.g. head, neck) that slowly grows, what skin disease would you consider?
|
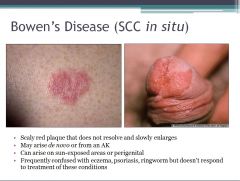
Bowen’s disease
|
|
|
What are indications for the Mohs procedure (MMS)?
|
• Recurrent tumor
• Positive margins • High risk for recurrence o Infiltrative BCC/SCC o Sclerosing BCC/SCC o Perineural spread o Location within scars o Rare aggressive tumors: sebaceous Ca, AFX, MAC, Paget’s disease, DFSP, LM, angiosarcoma • Poorly defined margins • > 2cm diameter • Immunosuppressed patient • Previous XRT treatment in area • Tissue conservation o H-zone of face, eyelids, ears, nose, lips, digits, nails, genitalia • Embryologic fusion planes o Periorbital, nasal, lips, ears, retroauricular sulcus, melolabial folds |
|
|
What is a macule/patch?
|
• A macule is a flat (non-palpable) color change of the skin < 1 cm
• A patch is the same as a macule but > 1 cm |
|
|
What is a papule/plaque?
|

• A papule is a raised lesion of the skin < 1 cm ( the profile can be flat topped, round, dome-shaped)
• A plaque is same as a papule but > 1 cm |
|
|
What is a vesicle/bullae?
|

• A vesicle is a lesion within the skin filled with CLEAR serous fluid < 1 cm
• Bullae > 1 cm |
|
|
What is a nodule?
|

A nodule is a lesion confined to the dermis > 1 cm
|
|
|
What is a pustule?
|

A pustule is a pus-filled papule ( raised lesion of the skin < 1 cm)
|
|
|
What is a keloid?
|

A keloid is a fibrotic (scarring process) that extends beyond the borders of the original defect.
|
|
|
In what skin condition is methotrexate used?
|
Psoriasis and other inflammatory conditions.
|
|
|
What oral retinoid is taken as prophylaxis against squamous cell carcinoma (SCC)?
|
Acetretin is an oral retinoid; it’s taken as a chemoprophylaxis, because it reduces # and frequency of squamous cell cancers
|
|
|
What is the hallmark of true urticarial (“hives”)?
|
Lesions should come and go over minutes/hours-->evanescent nature.
|
|
|
What’s the difference between Stevens-Johnson Syndrome and toxic epidermal necrolysis?
|

SJS features mucosal changes with up to 10% epidermal detachment vs more than 30% in toxic epidermal necrolysis.
|
|
|
What are 3 commonly implicated drugs in SJS/TEN?
|
1. TMP-SMX (Bactrim)
2. Phenytoin (Dilantin) 3. Phenobarbital |
|
|
What’s the difference between vellus vs. terminal hair?
|
Vellus hair is short, fine, light colored, whereas terminal hair is thicker, longer, colored.
|
|
|
Where are sebaceous glands most prominent?
|
Sebaceous glands are almost always found in association with hair follicles and are most prominent on the face, scalp, and upper trunk.
|
|
|
A 17 year old female presents with malaise, fatigue, fever, arthralgias, leukocytosis, elevated ESR and severe cystic acne with ulceration, purulent drainage, and eschar formation. What would you prescribe to her?
|
Should prescribe systemic glucocorticoids followed by oral retinoid; the patient has acne fulminans.
|
|
|
What symptoms are associated with polycystic ovarian syndrome (PCOS)?
|
• Oligomenorrhea (few menses)
• Hirsutism (increased terminal hairs in androgen-dependent areas of face and body) • Other signs of androgen excess (e.g., deepening voice, muscular habitus, female pattern androgenetic alopecia) |
|
|
What’s the first-line treatment of mild to moderate acne?
|
Topical retinoids target the microcomedo (initial lesion of acne) and are the first-line treatment of mild to moderate acne.
|
|
|
What medication is used to treat moderate to severe inflammatory acne?
|
Systemic antibiotics (most often tetracyclines) are indicated for the treatment of moderate to severe inflammatory acne.
|
|
|
What is rosacea?
|
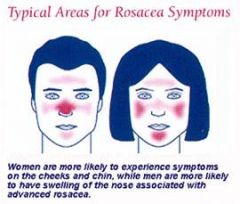
Rosacea is a chronic inflammatory disorder affecting the blood vessels and pilosebaceous units of the face. It’s characterized by increased reactivity, instability of capillaries leading to flushing, blushing, and telangiectases.
|
|
|
What is/are distinguish feature(s) between acne and rosacea?
|
• Unlike acne, comedones are NOT present in rosacea.
• Rosacea tends to occur in middle-aged, white patients (affects women>men) • Acne involves full face +/- trunk, whereas rosacea has a predilection for the central one third of face o Medial cheeks o Nose o Glabella o Chin • In rosacea, patients often complain of stinging, burning, increased sensitivity/irritability of skin • Rosacea has ocular symptoms (50% of pts have symptoms like photophobia, gritty sensation, frequent tearing, dry eyes, eyelid crusting (blepharitis), conjunctivitis) |
|
|
What are exacerbating factors for rosacea?
|
• Sun exposure, wind exposure
• Alcohol • Spicy foods, Hot liquids • Emotional stress |
|
|
What is hidradenitis supparativa?
|
Hidradenitis supparativa is an inflammatory and scarring process affecting the apocrine sweat glands. Proposed theory of pathogenesis involves keratinous plugging of the apocrine duct and hair follicle with resulting dilation of the apocrine duct and follicle and subsequent bacterial overgrowth.
|
|
|
What is the pathogenesis of acne vulgaris?
|
• Androgenic stimulation increases the size and secretory activity of sebaceous glands with corresponding increase in sebum production.
• Keratinocytes proliferate rapidly and become abnormally adherent (sticky). They block the outlet of the follicle, leading to impaction (blockage of the duct) and accumulation of sebum and keratinocyte debris • The accumulation of sebum and keratinocyte breeds the overgrowth of propionibacterium acnes, an anerobic gram(+) rod that inhabits the sebaceous glands and follicles. P. acnes binds Toll-like receptor 2 and produces pro-inflammatory mediators (IL-1, IL-8, TNF-alpha), which are chemotactic for neutrophils and other inflammatory cells • Proinflammatory cytokines (as well as free fatty acids) produced by P. acnes induce a sterile inflammatory response. Distention of the follicle can result in follicle wall rupture, releasing sebum, FFAs, bacteria, keratin into the dermis, which further incites inflammation and induces a foreign body response. Significant inflammation can lead to clinical scarring. |
|
|
What is acne congloblata?
|
Acne congoblata is severe cystic acne with trunk > face involvement.
|
|
|
What are some of the more prominent drugs that cause acne?
|
Certain medicines that may cause acneiform eruptions include anticonvulsants (phenytoin), antibiotics (isoniazid), anti-hypertensive medications, anxiolytics, steroids, hormonal agents (OCP’s), immunosuppressants (cyclosporine), chemotherapeutic agents such as tyrosine kinase inhibitors, lithium
|
|
|
What mites are known to inhabit hair follicles on humans and can be isolated from scrapings of pustular rosacea skin?
|
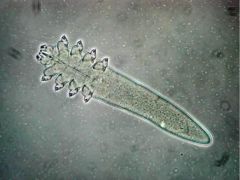
Demodex mites
|
|
|
What skin condition is associated with increased amounts of cathelicidin?
|
Rosacea. Cathelicidins serve a critical role in mammalian innate immune defense against invasive bacterial infection. Rosacea symptoms are exacerbated by factors that trigger innate immune responses, such as the release of cathelicidin antimicrobial peptides.
|
|
|
How would you treat periorificial dermatitis?
|
• Avoid topical corticosteroids!
• Topical agents – Metronidazole – Erythromycin, clindamycin – Sodium sulfacetamide/sulfur – Azelaic acid • Oral antibiotics – Doxycycline, minocycline, tetracycline – Erythromycin |
|
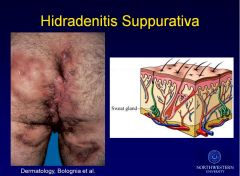
What are the top risk factors for hidadrenitis supparativa?
|
Hidradenitis supparativa is an inflammatory and scarring process affecting the apocrine sweat glands.
• Females >> Males, 4% reproductive age females – Females – axillae – Males – perianal, buttock involvement • Risk factors – Obesity – Family history of nodulocystic acne, HS (26%) – Follicle occlusion with secondary apocrine obstruction – Secondary bacterial infection – Tobacco use |
|
|
What does retiform mean?
|
Retiform means the bleeding into the skin follows outlines of blood vessels, branching like a tree, reticulate, net-like.
|
|
|
If purpura is palpable, what general information does that convey about the disease etiology?
|
Palpable purpura is indicative of immune or immune-complex mediated process.
|
|
|
What are disease etiologies for non-palpable purpura?
|
• Vessel weakness = non-retiform
o Ehlers-Danlos o Solar Purpura o Amyloidosis • Vessel occlusion = retiform o Bacterial or cholesterol emboli o Calciphylaxis o Fungi/aspergillus |
|
|
What diseases/conditions are most commonly associated with pyoderma gangrenosum?
|
Between 50-70% of patients with PG have antecedent or coincident associated disease or condition. Most common:
• Inflammatory bowel disease (ulcerative colitis and Crohn’s disease, 20-30%) • Arthritis (20%) • Hematologic disease (CML, hairy cell leukemia, myelodysplasia, and monoclonal gammopathy, 15-25%) o Monoclonal gammopathy often composed of IgA |
|
|
What is solar purpura?
|

Solar purpura is a chronic sun-induced degradation of collagen around blood vessels leading to easy fragility of the blood vessels to external trauma (as simple as someone scratching)
|
|
|
What are 4 of the 11 criteria for diagnosing lupus?
|

See image
|
|
|
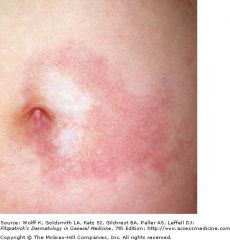
What is the most common type of cutaneous lupus, and what is the first line treatment for it?
|
• Discoid lupus; it represents a distinct, chronic subtype of lupus in which the disease is confined to the skin. A small percentage of those with discoid lupus can go on to develop systemic lupus (5%).
• First line treatment is intralesional triamcinolone injections, antimalarials |
|
|
Which disorder is associated with anti-Ro (SS-A) antibodies?
|
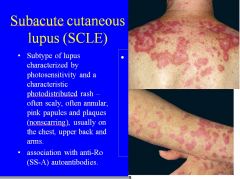
Subacute cutaneous lupus (SCLE)
|
|
|
What auto-antibodies are associated with systemic sclerosis? What are physical manifestations of the disease?
|
Anti-scl-70 autoantibodies are associated with systemic sclerosis.
Physical manifestations include: • Raynaud’s phenomenon • Sclerodactyly • Bird-like facies (can’t open mouth) • Dyspigmentation |
|
|
In the context of skin disorders, what is morphea?
|
Morphea is a skin-only form of scleroderma, aka. “localized scleroderma.”
|
|
|
Exposure to what chemical causes nephrogenic systemic fibrosis?
|
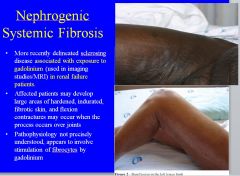
Gadolinium
|
|
|
What is sarcoidosis?
|
• Sarcoidosis is a systemic granulomatous disease of unknown etiology, which may affect virtually any organ in the body, commonly presenting in the skin.
• It’s characterized by non-caseating epithelioid granulomas. • Most common skin lesion: pink, skin-colored to reddish brown papules and plaques, especially on the face – periocular and perinasal |
|
|
What is lupus pernio?
|
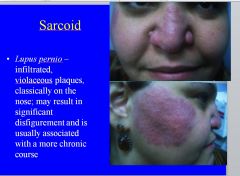
Lupus pernio is a skin manifestation of sarcoidosis. It’s characterized by infiltrated, violaceous plaques classically on the nose.
|
|
|
What is erythema nodosum (EN)?
|
• A panniculitis (inflammation in the subcuticular fat) that occurs as a reactive process, with associations reported with several systemic diseases, infections, and medications, but some cases are idiopathic
• Characterized by tender nodules, usually in the legs, especially in the extensor aspects, often with overlying erythema. Most common in young adults, especially women. |
|
|
What is clubbing (the skin-related definition)?
|

Clubbing refers to the soft tissue swelling around the terminal distal phalanx – the loss of the normal angle between the nail and the nail bed.
|
|
|
What are possible associated diseases in patients with alopecia areata?
|
Alopecia areata is thought to be an systemic autoimmune disorder in which the body attacks its own anagen hair follicles and suppresses or stops hair growth.[2] For example, T cell lymphocytes cluster around affected follicles, causing inflammation and subsequent hair loss. It's associated with:
• Autoimmune thyroid disease • Vitiligo • Diabetes • Atopic dermatitis |
|
|
What’s the pathogenesis of vitiligo?
|
• Vitiligo is an acquired autoimmune disorder of the skin in which destruction of melanocytes leads to well-demarcated patches of depigmentation.
• Affects up to 2% of the world’s population. Most commonly affected areas include the head and neck areas, bony prominences and dorsal hands. |
|
|
What joints does pseudomonas aeruginosa commonly attack in humans?
|
• Pseudomonas aeruginosa commonly attacks fibrocartilaginous joints such as the pubic symphysis, sternoclavicular, and sacroiliac joints.
• Commonly infects IV drug abusers. |
|
|
What pathogen most commonly causes septic arthritis in neonates, the elderly and immunocompromised individuals?
|
E. coli causes septic arthritis in neonates, the elderly, IV drug users, and immunocompromised hosts.
Also affects drug users. |
|
|
H. influenzae has been supplanted by another pathogen as the most common pathogen causing septic arthritis in children. What is that pathogen?
|
Kingella kingae
|
|
|
Which is more likely to result in disseminated gonoccal infection (DGI): symptomatic infection or asymptomatic mucosal infection?
|
Asymptomatic mucosal infection is much more likely to result in DGI than symptomatic infection and may have been sexually contracted days to months before dissemination.
|
|
|
What classic triad do patients with disseminated gonococcal infection (DGI) present with?
|
1. Dermatitis
2. Tenosynovitis (usually involving fingers, hands, wrists) a. Inflammation of the fluid-filled sheath that surrounds a tendon, producing the following symptoms: i. Pain ii. Swelling iii. Difficulty moving a particular joint where the inflammation occurs 3. Migratory polyarthalgia or polyarthritis |
|
|
What’s the vector for Lyme disease?
|
Lyme disease is caused by the spirochete Borrelia burgdorferi and transmitted by the Ixodes tick. B. burgdorferi is endemic to the northeastern and upper Midwest U.S. where white-tailed deer (preferred host for adult tick) are prevalent.
|
|
|
What pathogen causes the most common form of viral arthritis in the U.S.?
|
Parvovirus B19; typically presents as an acute, symmetrical polyarthritis of the proximal interphalangeal and metacarpophalangeal joints associated with morning stiffness and resembling rheumatoid arthritis.
|
|
|
What are risk factors for septic arthritis?
|
• Abnormal joint
• Immunosuppression • DM • Malignancy • Chronic renal failure • IV drug abuse • Previous intraarticular steroid injection |
|
|
What protein on S. aureus allows it to adhere to cartilage?
|
MSCRAMMs (microbial surface components recognizing adhesive matrix molecules)
|
|
|
What is the ddx for fibromyalgia?
|
• Hypothyroidism (check TSH)
• Polymyalgia rheumatica (check ESR) • Hypercalcemia (check serum Ca) • Hyperparathyroidism (check PTH) • Vitamin C (others?) |
|
|
What are the criteria for diagnosing fibromyalgia?
|

• Pain in 4 quadrants (bilateral and both upper and lower)
• Axial skeletal pain (C-, T-, or L-spine or anterior chest) • Pain in at least 11 of the 18 tender points |
|
|
What non-pharmacologic therapies are helpful for those with fibromyalgia, and in which group of fibromyalgia patients do non-pharmacologic therapies hold the greatest benefit?
|
• Patient education (particularly helpful for catastrophizers)
• Improved sleep hygiene (usually with Rx help) • Gentle aerobic and strengthening exercise • Cognitive Behavioral therapy • Massage therapy? |
|
|
What medicines help in treating fibromyalgia?
|
– Low-dose tricyclics
• Amitriptyline (Elavil, Endep) • Cyclobenzaprine (Flexeril, Cycloflex, Flexiban) – Serotonin-norepinephrine reuptake inhibitors (SNRI’s) • Milnacipran (Savella), Duloxetine (Cymbalta) • Venlafaxine (Effexor), tramadol (Ultram; also a m-opioid) – Serotonin-specific reuptake inhibitors (SSRI’s) • Fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft) – Anticonvulsants (GABA agonists) • Gabapentin (Neurontin, Gabarone) • Pregabalin (Lyrica) Note, the FDA has approved 3 agents (pregabalin, duloxetine, and milnacipran) |
|
|
What adverse effects do you have to watch out for in milnacipran, a treatment for fibromyalgia?
|
• Since it’s an SNRI (reuptake inhibitor of serotonin and norepinephrine), have to watch out for serotonin syndrome.
• Elevated blood pressure by 10-15 mm Hg in 10% of patients • Suicidality |
|
|
What is the definition of a strain?
|
Tearing/pulling of muscle or tendon
|
|
|
What is the definition of a sprain?
|
Tearing or pulling a ligament (attaches bone to bone)
|
|
|
What’s the difference between a closed fracture and open fracture?
|
For a closed fracture, the skin is intact, but in an open fracture the skin is violated, and there’s a risk of infection or occult tissue damage.
|
|
|
What is a reduction (in the context of orthopedic surgery)?
|
Reduction is the process of putting a bone or joint back in its place. It could be an open reduction, where an incision is made, and the bone is exposed.
|
|
|
What is fixation (in the context of orthopedic surgery)?
|
Fixation is to hold the bone in place.
|
|
|
In terms of imaging, what would you want to do for any long bone fracture?
|
For any long bone fracture, you would want an x-ray of a joint above and a joint below the fracture.
|
|
|
How is open fracture treated?
|
• Irrigation
• Debridement • Stabilization/fixation To • Reduce infection risk • Explore wound • Cut out necrotic tissue |
|
|
What is compartment syndrome, and how is it treated?
|
• Compartment syndrome is a limb and life threatening condition where there’s increased pressure in an enclosed compartment (arm, leg, belly). If the pressure is not released, the patient could get ischemia or permanent tissue damage.
• Compartment syndrome could be caused by o Injury o Fracture o Vascular injury o Crush o Snake bite o Burns • The appropriate treatment is fasciotomy |
|
|
What are the 5 Ps ofcompartment syndrome?
|
1. Pain
2. Pallor 3. Paralysis 4. Pulselessness 5. Parathesias You’re too late if you see all 5 |
|
|
What are the most common cancers that metastasize to bone, and in the bone, wheres the most common site of metastasis?
|
• Breast
• Lung • Thyroid • Kidney • Prostate (BLT with Kosher Pickle) Bone most common site is spine. |
|
|
What is the pathogenesis of osteogenesis imperfecta?
|
Osteogenesis imperfecta is characterized by a deficiency in synthesis of Type I collagen. Tissues affected/composed of Type I collagen: bone (multiple fractures that heal with excess callus), joints (joint laxity and secondary osteoarthritis), eyes (blue sclera due to choroidal veins showing through a thin sclera), ears (hearing defects), and dentin of teeth (dentinogenesis imperfect; DI).
|
|
|
How are menopause and osteoporosis related?
|
• During menopause, estrogen deficiency results in upregulation of IL-1, IL-6, and TNF-alpha and down-regulation of osteoprotegrin (OPG), a molecule produced by osteoblasts that blocks RANK:RANK-L interaction. (RANK:RANK-L interaction activates osteoclast-related genes.)
• The production of these molecules results in osteoclastogenesis and the loss of 35% of cortical and 50% of trabecular bone in 30-40 years. |
|
|
What is the pathogenesis of Rickets/Osteomalacia?
|
• Rickets: Vitamin D Deficiency results in the inability to calcify the zone of hypertrophy in the developing growth plate or to calcify osteoid formed throughout life during the remodeling process. Chondrocytes do not die and are not replaced by bone. In children with rickets, the growth plate becomes wide and irregular.
• Osteomalacia: once the growth plate closes, vitamin D deficiency makes it so that newly-formed osteoid fails to calcify, and the bones become weak. |
|
|
In which part of the bone do osteosarcomas generally develop?
|
Generally, osteosarcomas develop in the metaphysis of long bones of the young. OS in older patients presents more often in craniofacial bone or axial skeleton and usually is associated with a predisposing bone condition (e.g., Paget’s disease of bone, fibrous dysplasia, or prior radiotherapy).
|
|
|
Can you describe the pathogenesis of rheumatoid arthritis?
|
(1.) Activated CD4-“T” cells stimulate synoviocytes & macrophages to produce pro-inflammatory molecules (TNF, IL-1, TGF-beta & IL-6) which induce synoviocytes & chondrocytes to produce proteases resulting in damage to articular cartilage (arthritogen is possibly an infectious organism, collagen, proteoglycans, or citrullinated proteins such as fibrin).
(2.) RANKL promotes osteoclastogenesis resulting in bone erosions/osteoporosis. (3.) “B” cells produce antibodies (RF & anti-CCP) that cause immune complex-mediated tissue damage. (4.) Activation of vascular adhesion molecules promoting migration of inflammatory cells into joint. |
|
|
A palisaded granuloma is found in 75% of patients with what disease?
|

Rheumatoid arthritis
|
|
|
Which myositis has a male predominance, slow progression, distal or asymmetric weakness and a predilection for quadriceps more than hip muscles as well as finger flexor involvement?
|
Inclusion body myositis
|
|
|
Can you use corticosteroids for inclusion body myositis?
|
No; corticosteroids have only demonstrated anecdotal efficacy for inclusion body myositis, and that’s probably just for the initial phase which may have an inflammatory component.
|
|
|
What is a DMARD, and what is the first line DMARD for rheumatoid arthritis?
|
A DMARD is a disease-modifying antirheumatic drug (DMARDs), and the first line DMARD for rheumatoid arthritis is methotrexate; methotrexate is the gold standard for moderate to severe RA.
|
|
|
What drugs can be used to treat patients with milder rheumatoid arthritis?
|
Sulfasalazine and hydroxychloroquine can be used to treat patients with milder rheumatoid arthritis.
|
|
|
Which form of arthritis spares the DIP joint as well as thoracolumbar spine?
|
Rheumatoid arthritis
|
|
|
What are classic symptoms of rheumatoid arthritis?
|
• Usually insidious onset symmetric polyarthritis (>3 joints)
• Joint swelling • Eventual decreased range of motion • Morning stiffness >1 hour • Stiffness after rest (gelling) • Pain and swelling worse in the morning • Pain in the balls of the feet upon first ambulating in the morning |
|
|
What’s the difference between Swan-neck and Boutenniere’s deformities?
|
• Swan neck
o Flexion at DIP, hyperextension of PIPs • Boutenniere o Flexion at PIP and hyperextension of DIP |
|
|
What is the proposed mechanism of action of methotrexate in treating rheumatoid arthritis?
|
• Originally thought to suppress lymphocyte proliferation but possibly mechanism is anti-inflammatory.
– Inhibits neovascularization – Inhibits neutrophil activation and adherence – Inhibits IL-1 and IL-8 production by mononuclear cells – Inhibits TNF production by T cells |
|
|
What laboratory tests are highly specific for lupus (SLE)?
|
• Anti-dsDNA
• Anti-sm |
|
|
What are predictors of a lupus (SLE) flare?
|
• Predictors of flare (in some but not all cases):
— New evidence of complement consumption — Rising anti-dsDNA titers — Increased ESR — New lymphopenia |
|
|
What are the leading causes of mortality in patients with lupus (SLE)?
|
Leading causes of mortality are:
• heart disease • malignancy • infection |
|
|
What clinical symptoms would make you want to put lupus in the differential?
|
• Rash
• Arthritis • anemia • Thrombocytopenia • Serositis • Nephritis • Seizures • Psychosis |
|
|
What is the mechanism of action of NSAIDs?
|
NSAIDs inhibit the formation of prostaglandins by blocking cyclooxygenase, which converts arachidonic acid into prostaglandins.
|
|
|
How do prostaglandins amplify pain?
|
• In inflammatory or in injury states, prostaglandin formation is upregulated, either in the periphery or the CNS or both.
• In the periphery, COX2 is upregulated, increasing PGE formation, and it is believed the binding of PGE to nociceptive (pain) nerve endings causes them to lower their firing thresholds so that touch induces pain. • In the CNS, prostaglandin formation is upregulated, allowing the CNS to transmit, modulate, and amplify pain transmission. That’s why NSAIDs can reduce pain even in the lack of inflammation (e.g., headaches). |
|
|
Can you concisely explain the role of prostaglandins in the following organs: stomach, kidney, uterus, platelets, endothelium, CNS/periphery?
|
• Stomach: forms mucus, improves blood flow, prevents autodigestion
• Kidney: maintain blood flow in low-flow states, involved in Na+/H2O balance • Uterus: contraction of uterine muscle, many functions related to reproduction • Platelets: thromboxane enables platelets to clump and form clots • Endothelium: prostacyclin causes vasodilation and inhibits platelet adherence • CNS and periphery: enhances pain transmission |
|
|
Why should you be careful about the use of NSAIDs in asthmatics?
|

Blocking COX can increase the formation of Leukotrienes, which can precipitate bad asthmatic attacks in 10% of asthmatics.
|
|
|
Why do NSAIDs sometimes cause ulcers? What can you use to stave off this concern?
|
• PGs protect the stomach lining by facilitating the production of the mucous layer. Therefore, blocking PGs with NSAIDs can lead to ulcers.
• Misoprostol can be given to help protect the gastric lining, because it increases the formation of mucus (unfortunately, it can also cause diarrhea). |
|
|
Why can’t you give NSAIDs to people with low kidney flow/function?
|
In decreased perfusion states, PGs dilate the afferent blood vessels. If you block PGs, this dilation will not occur, and you could possibly get an infarct and renal failure. Therefore, do not give NSAIDs to people with low kidney flow/function.
|
|
|
Do COX2 inhibitors like celecoxib have any effect on platelet function?
|
No; COX2 inhibitors don’t bother platelets.
|
|
|
What tests should you periodically run on someone who’s taking NSAIDs?
|
Need to:
• Check stool guaiac for GI bleeding • Check BP • Check renal function tests • Check LFTs |
|
|
What drug should be avoided in children who have recently had a viral illness?
|
Aspirin/ASA. Can cause Reye’s syndrome (fulminant liver failure). Absolutely avoid!
|
|
|
Can you name all the NSAIDs he mentioned in lecture?
|
• Ibuprofen: Over the counter use limited to 7 days of 600mg/day but prescription goes to 2400mg/d. Cheap
• Naproxen: bid dosing, OTC 7 day use at 220mg bid, prescription is 750 bid peak. Cheap, like ibuprofen • Indocin/indomethacin- used more for gout, closing patent ductus in neonates • Diclofenac- some more hepatotoxicity, possibly more hypertension and hence more CV toxicity than ibuprofen, naproxen and other NSAIDs, available topically • Nabumetone: The only nonacidic NSAID, gets absorbed then converted to acid. Big deal. • Ketorolac: best used IV • ASA: Weak analgesic, but great cardioprotection and stroke protection via plt inhibition • Meloxicam/Mobic: The books keep saying it’s COX2 selective. It’s not. Don’t use it before surgery. • Celebrex: The only COX2 surviving, no platelet effect, better GI tolerance. Does not interfere with aspirin cardioprotection, unlike all other NSAIDs |
|
|
What are 3 of the most important pro-inflammatory cytokines identified in rheumatoid arthritis?
|
1. IL-1
2. IL-6 3. TNF-alpha |
|
|
In which pediatric vasculitis should you be wary of currant jelly stools?
|

HSP
|
|
|
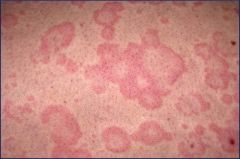
What is the rash like in Systemic Onset Juvenile Idiopathic Arthritis (sJIA)?
|

The rash in sJIA is an evanescent, maculopapular, salmon pink rash
|
|
|
What are clinical signs in Systemic Onset Juvenile Idiopathic Arthritis (sJIA)?
|
• Arthritis can be minimal at onset, any joint, increases in severity over time for many
• High spiking quotidian fever: to 39 deg C or above, 1-2x daily w/ rapid return to normal or below • Rash: evanescent, maculopapular, salmon pink rash • Serositis: pericarditis, pleuritis • Generalized lymphadenopathy • Hepatosplenomegaly – one or both |
|
|
What potentially serious complication can occur in Systemic Onset Juvenile Idiopathic Arthritis (sJIA), and what are its symptoms?
|
• You can get macrophage activation syndrome (MAS), characterized by: spiking fevers, enlarging liver and spleen, hemorrhage, CNS dysfunction
• Lab data: decreased Hb, platelets, WBCs. Increased tryglycerides. Decreasing ESR. Hypofibrinogenemia, elevated D-dimers, very high ferritin • Rx: cyclosporine, first IV then PO and corticosteroids |
|
|
What are available treatments for Systemic Onset Juvenile Idiopathic Arthritis (sJIA)?
|
1. Corticosteroids PO and IV in addition to NSAIDs
2. Methotrexate (immunosuppressive) 3. Biologic: TNF, IL-1, IL-6 antagonists 4. Treat steroid-related osteopenia w/ Ca++ and vit D |
|
|
How would you differentiate the rash in juvenile dermatomyositis from that of other pediatriac vasculitides?
|

Look for Gottron papules and heliotrope rash in juvenile dermatomyositis (JDM)
|
|
|
What are the diagnostic criteria for juvenile dermatomyositis (JDM)?
|
• Rash
• Symmetric proximal muscle weakness • Elevated muscle enzymes • Characteristic EMG changes • Characteristic muscle biopsy findings: necrosis, perifascicular atrophy, perivascular mononuclear infiltrate |
|
|
How would you differentiate the immunological basis of an autoinflammatory disease vs an autoimmune disease?
|
Autoinflammatory diseases are a perturbation of innate immunity (neutrophils and macrophages) whereas autoimmune diseases are perturbations of adaptive immunity (B cells, T cells, T regulatory cells).
|
|
|
What is the definition of osteoarthritis?
|
Osteoarthritis is the softening, fibrillation, ulceration, and loss of articular cartilage, with osteophyte formation, sclerosis, and eburnation of subchondral bone, resulting from both mechanical and biologic events that destabilize the normal coupling of degradation and synthesis of articular chondrocytes and extracellular matrix.
|
|
|
How do you differentiate osteoarthritis from rheumatoid arthritis?
|
Osteoarthritis is a deterioration of cartilage and overgrowth of bone often due to “wear and tear.” Rheumatoid arthritis is the inflammation of a joint’s connective tissue, such as the synovial membranes, which leads to the destruction of the articular cartilage.
|
|
|
What are the risks for osteoarthritis in the following individuals: recreational athlete, non-elite athletic person, elite athlete?
|
• Recreational – no increase in risk
• Non-elite athletic – probably no increase in risk, unless injury occurs • Elite athletic, i.e., competitive at national level – increase in risk |
|
|
What are atypical joints for osteoarthritis to appear in, for which you must consider secondary OA?
|
• MCP
• Wrist • Elbow • Shoulder • Ankle |
|
|
What is scleroderma renal crisis (SRC), and what are major risk factors for SRC?
|
• Scleroderma renal crisis occurs when medium-sized arteries are injured, resulting in malignant HTN, hyperreninemia, microangiopathic hemolytic anemia and rapidly progressive renal failure. It develops in up to 15% of patients with dcSSc, almost always within the first 4 years of disease.
• Major risk factors include: o Extensive and advancing skin involvement o Large joint contractures and tendon friction rubs o Presence of autoantibodies to RNA polymerase III |
|
|
How is Raynaud’s disease treated in scleroderma patients?
|
Vasodilators are used to treat Raynaud phenomenon, including:
• CCBs • Nitrates • ARBs and ACE inhibitors • ET-1 receptor blockers, • PDE-5 inhibitors, etc. |
|
|
What cytokines and growth factors are important in the fibrosis process of scleroderma?
|
• TGF-beta
• CTGF • PDGF • Wnt • Endothelin-1 (ET-1) Each of these promote the synthesis of collagen, proteoglycans, fibronectin, fibrillin, tenascin and elastin. Progressive buildup of these molecules results in fibrosis. |
|
|
What ANA immunofluorescence (IF) distribution pattern is specific for scleroderma?
|
Nucleolar IF pattern
|
|
|
How are the GI (GERD, malabsorption) and lung (fibrosis, PAH) manifestations of scleroderma treated?
|
• GERD – PPI
• Malabsorption – rotating abx, prokinetic agents, hyperalimentation • Fibrosis – Cytoxan • PAH – ET-1 blockers, NO, Prostanoids (epoprostenol, trepostenil) |
|
|
What is the underlying pathophysiology of gout, and what are potential causes?
|
Hyperuricemia is the underlying cause of gout. This can occur due to:
• Diet • Genetic predisposition • Under-excretion of urate, the salts of uric acid (90% of cases) |
|
|
What is the most common presentation of gout?
|

Gout most commonly occurs as a recurrent attack of acute inflammatory arthritis, most commonly affecting the metatarsal-phalangeal joint at the base of the big toe (50% of cases).
|
|
|
What is the first line of treatment for gout?
|
• NSAIDs
• Improvement may be seen within 4 hours • Treatment is recommended for 1-2 weeks |
|
|
What medicines are used for preventing gout episodes?
|
• Allopurinol
• Probenecid • Febuxostat |
|
|
Where does calcific tendinitis most commonly occur?
|
• Shoulder; usually in muscles that abducts and stabilized the shoulder
• Bursitis, impingement syndrome |
|
|
What stain is used to detect BCP (basic calcium phosphate) crystals from aspirate samples?
|
Alizarin red stain
|
|
|
What are the 2 most common sites of chondrocalcinosis in CPPD (Calcium Pyrophosphate Dihydrate Deposition Disease) patients? Chondrocalcinosis refers to radiographic calcification in hyaline and/or fibrocartilage. It is commonly present in patients with CPPD crystal deposition disease but is neither absolutely specific for CPPD nor universal among affected patients.
|
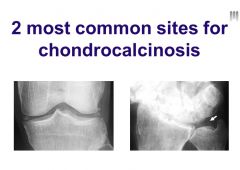
Most common sites for chondrocalcinosis are within the knee and the wrist
Can see calcification particularly within the menisci in the knee |
|
|
What’s the association between osteoarthritis (OA) and chondrocalcinosis? Chondrocalcinosis refers to radiographic calcification in hyaline and/or fibrocartilage. It is commonly present in patients with CPPD crystal deposition disease but is neither absolutely specific for CPPD nor universal among affected patients.
|
People with OA more commonly have chondrocalcinosis; there’s some association between the two
|
|
|
What foods should be avoided for those who have gout?
|
• Meat
• Shellfish • Ethanol (esp. beer) • Soft drinks and high fructose syrup |
|
|
What drugs should be avoided in those with gout?
|
• Thiazide
o Thiazide cause increased resorption of solutes at the proximal tubule, including uric acid, so thiazide diuretics can increase the concentration of uric acid • Cyclosporine o Decreases renal excretion of uric acid • Low-dose ASA (<1g/day) o Decreases renal excretion of uric acid |
|
|
How do you determine whether someone with gout is an underexcreter or overproducer?
|
You can collect urine levels of uric acid and creatinine for 24 hours, and:
• > 1000 mg overproducer – kidneys are working fine • < 1000 mg underexcretor – kidneys not working fine |
|
|
What drugs would you use to prevent a gout attack in an overproducer of uric acid?
|
Xanthine oxidase inhibitors can be used to treat those with overproducing individuals and individuals with renal disease:
• Allopurinol • Febuxostat |
|
|
What are all the seronegative spondyloarthropathies?
|
• Psoriatic arthritis
• Ankylosing spondylitis • Inflammatory bowel disease • Reactive arthritis Remember PAIR. |
|
|
What HLA (surface antigen) is associated with reactive arthritis?
|
HLA-B27
|
|
|
What is Enthesopathy/enthesitis?
|

Enthesopathy/enthesitis is inflammation of tendon sheaths/ at tendon insertions into bone
|
|
|
What’s the most common oral manifestation of reactive arthritis?
|

Erosion of the hard palate is the most common oral manifestation of reactive arthritis.
(Can also get oral ulcers.) |
|
|
Broadly, what are the 2 types of arthritis, and what are examples of each type?
|
• 2 types of arthritis: inflammatory v. noninflammatory
• OA is the classic non-inflammatory arthritis • RA and these serognegative spondyloarthropathies are inflammatory arthritis |
|

Which seronegative spondylarthropathy is associated with the pencil-in-a-cup radiographic finding?
|
Psoriatic arthritis
|
|
|
What is ankylosing spondylitis?
|
• Systemic inflammatory arthritis with both axial and peripheral involvement
• May have extra-articular manifestions • Strongly associated with HLA-B27 (~90%) • Animal data suggests this may be pathogenic via molecular mimicry (B27 transgenic rat model) • ~80% male |
|

Which seronegative spondylarthropathy is associated with the “dagger” radiographic finding?
|

Ankylosing spondylitis
|
|
|
What seronegative spondylarthropathy is associated with the following history: Inflammatory back pain gets better with exercise and worse with rest, and it feels bad at night; more commonly seen in young people?
|

Ankylosing spondylitis
|
|
|
What are the criteria for failure to thrive (FTT)?
|
• Failure to thrive is when growth in a child’s growth is below age-and gender-based standards. Criteria:
• Weight or height < 3rd percentile • Weight-for-height < 5th percentile • Weight <80-85% of the median (50th percentile) • Weight or height drop of two major percentile of channels from the child’s previous measurements • Weight loss of >=10 % |
|
|
What’s the genome like for rotavirus?
|
Rotavirus has double-stranded segmented RNA genome with no envelope and a nuclear capsid.
|
|
|
What approximate ratio of glucose to Na+ is desirable for rehydration solutions?
|
1-2:1
|
|
|
What are the monosaccharide components of sucrose?
|
Sucrose = glucose + fructose
|
|
|
Is it okay to use juice for rehydration in children?
|
Juice is not appropriate in the treatment of dehydration or management of diarrhea.
|
|
|
What are some factors that are important for the evaluation of undernutrition in a child?
|
• Mother/child interaction
• Formula preparation • Adequacy of breast feeding • Head circumference sparing -NOT type of standard infant formula provided |
|
|
What are important clinical parameters to assess in a child with acute encephalopathy?
|
• pH
• lactate value • electrolyte concentrations • liver function • glucose status Ammonia should be measured for any ill child who has unexplained lethargy or vomiting. The presence of ketones in the urine may also be important. |
|
|
What are acute clinical signs of encephalopathy in a baby?
|
• Poor sucking
• Drowsiness or irritability • Poor tone • Abnormal cry • Vomiting |
|
|
What is the pathogenesis of Maple Syrup Urine Disease (MSUD)?
|
MSUD has abnormal metabolism of branched-chain amino acids (e.g., Ile, Val, Leu)
|
|
|
What is the pathogenesis of phenylketonuria (PKU)?
|
• Deficiency of phenylalanine hydroxylase (PAH)
• Phenylalanine (PHE) (substrate) cannot be converted to tyrosine (product) and is restricted in diet • TYR becomes conditionally essential and therefore needs to be supplemented (in medical formula) • Unrestricted, PHE accumulates in the blood and is toxic to brain myelination and growth • Classic PKU = PHE level of 20 mg/dL or greater at diagnosis |
|
|
Why do patients with undiagnosed PKU present with “fair” hair and skin tone?
|
Fair hair and skin tone is due to tyrosine
|
|
|
In what trimester do high levels of Phenylalanine have their greatest bad effects in maternal PKU?
|
In the first trimester
|
|
|
What is maternal PKU?
|
• An elevated maternal level of PHE that causes damage to a developing fetus.
• Elevated maternal serum PHE levels may cause spontaneous abortion, microcephaly, mental retardation, congenital cardiac anomalies, and intrauterine growth retardation (IUGR). |
|
|
What urea cycle deficiencies are not identified with newborn screening, why, and how are they treated?
|
Not identified on newborn screening:
1) Ornithine transcarbamylase deficiency* 2) Carbamyl phosphate synthetase I deficiency* • OTC and CPS are harder to identify, because they’re in the mitochondria • For CPS, they give high doses of citrulline; for OTC they give high doses of citrulline or arginine |
|
|
What transporter is responsible for the uptake of glucose in the liver?
|
Glucose transporter-2 (GLUT-2) is responsible for hepatic uptake of glucose.
|
|
|
What is Wilson’s disease, and how is it treated?
|
• Wilson’s disease is a genetic abnormality related to copper excretion. Normally absorbed copper accumulates in hepatocytes that are unable to excrete copper in the bile.
• Treatment involves chelation or the use of zinc in efforts to increase loss via the GI tract by sequestering absorbed copper in enterocytes that regularly slough off and are shed in the stool. |
|
|
What are the 3 factors for prioritizing patients for liver transplants (the MELD score)?
|
1. Prothrombin time (PT)
2. Creatinine 3. Bilirubin |
|
|
What should you try first in terms of treatment/management in a patient with a long prothrombin time (PT)?
|
Anytime you have a pt w/ a long PT, give them a course of vit K and see if it gets better
|
|
|
What are the components of metabolic syndrome?
|
• Dyslipidemia
• Insulin resistance • HTN • Abdominal/central obesity |
|
|
What waist circumference cutoffs for men and women are indicative of abdominal obesity?
|
• 35 inches for women
• 40 inches for men =Clinically diagnostic of abdominal obesity |
|
|
How does saturated fat increase LDL levels?
|
Saturated fat, specifically comprised of myristic, palmitic and lauric fatty acids found predominately in meat, high fat dairy, and palm oil, raises LDL-C by decreasing expression and functional activity of hepatic LDL receptors.
|
|
|
What are the only diet-related factors that appear to influence HDL-C favorably?
|
• Physical activity
• Alcohol |
|
|
What are the essential fatty acids?
|
Essential fatty acids
- Poly unsaturated fatty acids (PUFA) - n-6 PUFA - n-3 PUFA |
|
|
What’s the best animal source for omega-3-fatty acids? What’s the best plant source for omega-3-fatty acids?
|
• Salmon (animal)
• Flax-seed oil (plant) |
|
|
What is the definition of glycemic index?
|
The glycemic index represents the blood sugar response to ingestion of a 50g carbohydrate portion of a given food tested expressed as a percent of the response to the same amount of carbohydrate from white bread or pure glucose consumed by the same subject.
|
|
|
What’s the difference between marasmus and kwashiorkor?
|
Marasmus is primary a deficit of calories, characterized by very low body weight and significant wasting of lean body mass due to prolonged and severe energy deficit.
Conversely, the primary nutritional deficit in kwashiorkor is protein. Kwashiorkor is characterized by a diet rich in carbohydrates but extremely low in protein. Patients with kwashiorkor develop: edema, ascites (due to low albumin), fatty infiltration of the liver, a characteristic skin, rash and hair depigmentation |
|
|
What is cachexia?
|
Cachexia is a state of energy deficit coexisting with illness (i.e., it’s starvation complicated by an illness).
|
|
|
How many grams per day of dietary carbohydrates are needed to prevent ketosis?
|
100 g
|
|
|
What hormones are decreased/increased in starvation and weight loss?
|
Decreased:
• Energy expenditure • Leptin • T3 and T4 Increased: • Ghrelin • Muscular efficiency |
|
|
Why does your BMR and protein catabolism increase in cachexia?
|
Increased BMR due to:
• Catecholamines and sympathetic nervous system stimulation • Fever • Inflammation and cytokines Increased protein catabolism due to: • Inflammation and cytokines • Increased cortisol • Insulin resistance |
|
|
What are the criteria for diabetes?
|
1. Glycosylated hemoglobin (HbA1c) >= 6.5 % or
2. Fasting plasma glucose >= 126 mg/dl or 3. Plasma glucose >= 200 mg/dl 2 hours after 75 g glucose tolerance test or 4. Random plasma glucose >= 200 mg/dl in the presence of classic hyperglycemia symptoms |
|
|
What are the criteria for prediabetes?
|
1. Fasting plasma glucose 100-125 mg/dl or
2. Plasma glucose 140-199 mg/dl after glucose tolerance test or 3. HbA1c 5.7-6.4% |
|
|
Can you describe the plate method for basic medical nutrition therapy (MNT) for diabetes?
|
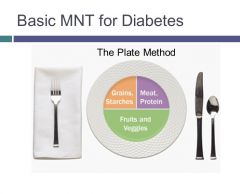
Take a plate, and half of it should be fruits & veggies. ¼ grains and starches and ¼ meat, protein
|
|
|
What are some benefits of a low glycemic index diet?
|
• Reduces postprandial glucose levels in normal individuals and people with diabetes
• Produces modest improvements in HbA1c • May or may not affect insulin sensitivity • May be beneficial for weight management in individuals with insulin resistance • May reduce LDL cholesterol and TG and increase HDL • May reduce markers of inflammation |
|
|
Which food allergies are outgrown vs not outgrown?
|
• Outgrown
o Milk o Eggs o Wheat o Soy • Not outgrown (only 20% of kids will outgrow allergies to these foods) o Peanuts o Tree nuts o Fish o shellfish |
|
|
What is Eosinophilic Esophagitis (EoE)? How is it treated?
|
• EoE is characterized by dense infiltration of eosinophils within the epithelium that may extend into the deeper layers of the esophagus associated with distinctive endoscopic changes and is present in ~10% of adults with dysphagia.
• It’s a male dominant disease (3:1) • EoE is treated with either swallowed inhaled steroids (flovent or oral budesonide) or dietary restriction |
|
|
What are the big 6 food allergens?
|
1. Wheat
2. Soy 3. Milk protein 4. Eggs 5. Nuts/tree nuts 6. Fish/shellfish |
|
|
What is the typical clinical presentation of a child with Eosinophilic Esophagitis (EoE)?
|
w/ eosinophilic syndrome, children classically avoid eating
|
|
|
What haplotype is associated with celiac disease?
|
DQ2/DQ8
|
|
|
What are some non-GI manifestations of celiac disease?
|
• Anemia
– 5-8% adults with non-responsive anemia have CD • Hepatitis – 9% Adults have elevated LFTs • Arthritis • Neurological – Epilepsy with cranial calcifications |
|
|
What are some challenges to the gluten-free diet that can impact quality of life in patients?
|
• Challenges to GF diet that impact QOL include:
1. food labeling/hidden sources, 2. social eating, and 3. extensive travel. |
|
|
What heritable disease is caused by the inability to absorb zinc in the GI tract?
|
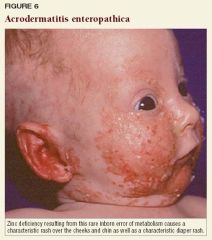
Acrodermatitis enteropathica; the rare disorder is characterized by a particular pustular rash associated with anglular cheilitis, diarrhea, alopecia, and immunodeficiency.
|
|
|
What is the predominant source of zinc in the diet?
|
Animals
|
|
|
What are ways in which zinc deficiency affects the immune system?
|
• Zinc deficiency results in decreased production of serum thymulin, a zinc-containing hormone responsible for stimulating traffic of mature lymphocytes from the thymus.
• Zinc deficiency results in fewer CD4 cells differentiating into the Th1 phenotype. o As a result, macrophages become less effective killing intracellular organisms. o Natural killer T-cells become less effective killing virally-infected cells. |
|
|
What is the physiologic role of vitamin C in the body?
|
• Vitamin C serves as an electron donor for a wide range of essential chemical reactions within the body.
• Supplementation of Vitamin C has resulted in widespread effects, including: o Increased lymphocyte, neutrophil, and monocyte chemotaxis o Increased T-cell proliferation o Enhanced collagen synthesis • Many different types of human cells, particularly immune cells and epithelial cells, take up Vitamin C and recycle it in order to be able to squelch reactive oxygen species • In the absence of adequate Vitamin C and other anti-oxidants, reactive oxygen species accumulate in phagocytic cells and cause oxidative stress |
|
|
What’s the name for the active form of vitamin A?
|
Retinoic acid
|
|
|
What diseases can be treated with zinc?
|
In children in developing countries, Zn treats diarrhea, pneumonia, malaria with reduction in mortality
|
|
|
What populations are at risk for the development of zinc deficiency?
|
• Vegetarians
• The poor in developing countries • Lactating mothers whose babies deplete them of zinc through their milk • Those with genetic mutations that can’t absorb dietary zinc • Those with chronic illness causing malabsorption |
|
|
This storage form of phosphorus, found in grains and legumes, chelates zinc and prevents its absorption. What is it?
|
Phytate
|
|
|
What are typical symptoms of scurvy?
|
Low energy
1) Low energy 2) Vomiting 3) Bleeding gums 4) Aching joints |
|
|
Which vitamin is “the ultimate electron donor?”
|
Vitamin C
|
|
|
What are natural sources of vitamin A?
|
• Sources:
o Dark green leafy vegetables o Animals o Cod liver oil o Other yellow and orange fruits and vegetables |
|
|
What illnesses can be prevented by vitamin A supplementation?
|
• Decreased morbidity and mortality in young children from
o DIARRHEA o MALARIA o HIV o MEASLES |
|
|
What are some physiologic roles for vitamin A in the body?
|
1) Retinoic Acid (RA) is a transcription factor. RA acts in a cell’s nucleus by binding to a retinoic acid receptor protein and a gene’s promoter to induce or suppress transcription.
2) Only certain cells have the enzyme which catalyzes the last step to form retinoic acid (RA), the active molecule. So RA acts locally. 3) Dendritic cells in the gut are stimulated by retinoic acid to activate B cells and to attract T cells to the gut. |
|
|
How are wet and dry beriberi different?
|
• Dry beriberi (sometimes confused with Guillain-Barre syndrome) presents with symptoms of peripheral neuropathy, e.g. wrist/foot drop
• Wet beriberi presents with symptoms of heart failure in addition to neuropathy |
|
|
What are major risk factors for thiamine deficiency?
|
• Alcoholism
• Eating disorders • Gastrointestinal surgery |
|
|
What nutrient deficiency is characterized by the following signs/symptoms: weakness, glossitis (sore, red tongue), angular stomatitis (cracks and sores at the corner of the mouth) and cheilosis (cracks and sores on the lips)?
|
Riboflavin deficiency
|
|
|
What nutritional deficiency is characterized by dermatitis, diarrhea, dementia, and death (high mortality)?
|

Pellagra (niacin deficiency)
|
|
|
How would you clinically distinguish between vitamin b12 deficiency and folate deficiency (using a lab test)?
|
Although both deficiencies result in a build up of homocysteine levels, vitamin B12 (cobalamin) also results in a build up of methylmalonyl-coA (MMA), which can be used to distinguish between the two deficiencies.
(Cobalamin serves as a cofactor for MMA-mutase, catalyzing conversion of MMA to succinyl-coA.) (B12) |
|
|
What’s the pathogenesis of goiter in iodine deficiency?
|

Thyroid gland hyperplasia occurs due to elevated levels of TSH in iodine deficiency, producing a goiter.
|
|
|
What’s the physiologic role for thiamine in the body?
|
• Thiamine diphosphate serves as a cofactor for a number of enzymes involved in carbohydrate and amino acid catabolism, neurotransmitter formation, and DNA formation, including:
o Alpha-ketoglutarate dehydrogenase o Pyruvate dehydrogenase o Transketolase |
|
|
What are typical symptoms of Wernicke-Korsakoff syndrome (cerebral beriberi)?
|
• Ataxia
• Confusion • Impaired memory • Confabulation • Disordered eye motility • Neuropathy |
|
|
What clinical signs are pathognomonic for scurvy?
|

Corkscrew hairs and perifollicular petechiae in scurvy. Perifollicular petechiae (areas of bleeding into the hair follicles) are among the earliest signs and are pathognomonic of scurvy.
|
|
|
What is the most common preventable cause of mental retardation in the world?
|
Iodine deficiency is the most common preventable cause of mental retardation in the world.
|
|
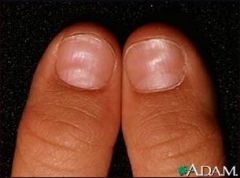
In what nutrient-deficient condition do you see koilonychias (“spoon nails”)?
|
Iron-deficiency
|
|
|
What is the treatment of choice for Merkel cell carcinoma (MCC)?
|
Merkel cell carcinoma (MCC) is a rare neuroendocrine tumor that has a
predilection for the head and neck in older adults. It presents as a rapidly growing violaceous to pink nodule. MCC is an aggressive neoplasm with high rates of both local recurrence and distant metastasis. Surgical resection is the mainstay of treatment for MCC though radiation and/or chemotherapy are frequently used as adjuncts. |
|
|
What is the treatment of choice for dermatofibrosarcoma protuberans?
|
Dermatofibrosarcoma protuberans (DFSP) is a rare fibrohistiocytic tumor of
the skin. It is a locally aggressive sarcoma that even with proper treatment has a high rate of local recurrence. This tumor favors the trunk and proximal extremities and presents as a firm brown to dark red nodule that slowly grows in size. It is frequently mistaken for a keloid, hypertrophic scar or an inflamed cyst. Mohs micrographic surgery or wide resection is the treatment of choice. |

