![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back
|
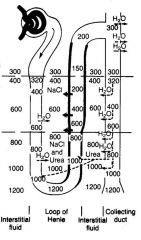
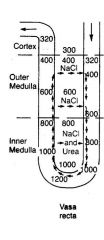
Outlined black area impermeable to water; starts at 300 -> 1200> at top you're down to 150
Salt is being pumped out of ascending loop of henle which accounts for half the concentration of sodium (300 -> 150) |
|
|
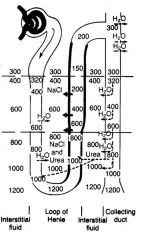
Interstitium; more dilute at top, more concentrated at the bottom
salt and urea gets pumped out into interstitium; why doesn't it diffuse away and equalize gradient? |
|
why doesnt interstitial conc just diffuse away?
|
Vasa recta countercurrent system;
blood comes down and goes up but at every moment a gradient exists to maintain the gradient; 1200 is max concentration; gerbils are much more conc (4000); pee out pellet |
|
|
Aquaporins
|
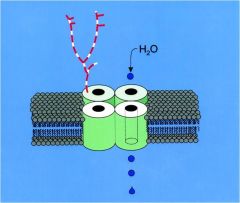
water channels inserted into cell membrane (they can go up or down); facilitate rapid movement of water across membrane
under influence of ADH (from posterior pituitary gland) |
|
|
alternative names for ADH
|
vasopressin or AVP (arginine vasopressin)
|
|
|
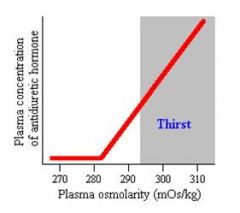
when is ADH released?
|
changes in extracellular fluid osmolality (cells in hypothalamus detect osmolariy)
nonosmotic factors such as physical pain, stress or a drop in bp |
|
|
older people won't get thirst
|
|
|
High sodium levels indicates
|
Not even water, thus Na is conc
|
|
|
Causes of hypotonic water loss
|
Gastrointestinal losses
• vomiting • nasogastric suction • enterocutaneous fistula • diarrhea Renal losses • diuretic use • osmotic diuresis • post obstructive diuresis • non-oliguric acute renal failure |
|
|
Causes of hypotonic water loss
|
Gastrointestinal losses
• vomiting • nasogastric suction • enterocutaneous fistula • diarrhea Renal losses • diuretic use • osmotic diuresis • post obstructive diuresis • non-oliguric acute renal failure |
|
|
osmotic diuresis
|
something you've put in that has a high conc that dilutes the blood
natural one: glucose (out of control diabetic pulls water out of cells) |
|
|
Causes of pure water loss
|
Increased insensible loss
• fever Increased insensible loss with no fluid replacement • inability to obtain water, such as when trapped in a collapsed building, or having suffered a stroke Diabetes insipidus • nephrogenic • hypothalamic |
|
|
Na gain
|
Exogenous
• salt ingestion • intravenous hypertonic saline • intravenous sodium bicarbonate Endogenous • mineralocorticoid excess |
|
|
mineralcorticoid excess
|
make too much of a hormone which causes you to raise minerals (never this)
|
|
|
Hypovolemia urine Na>20 mmol/L
|
kidney dumping out salt; should be trying to hold onto them
|
|
|
Glucocorticoid deficiency
|
you were on steroids and someone forgot to give you more when you came into hospital
|
|
|
SIADH
|
Syndrome of Inappropriate ADH
|
|
|
Urine Na <20 mmol/L
|
Kidney is retaining sodium so it's working fine; must be losing salt EXTRArenally
|
|
|
Key questions
|
Kidney is either trying to hold onto sodium or remove it
Kidney is either trying to hold onto water or remove it Get osms |
|
|
Plasma Osmolality Equation
|
2[Na+] + Glucose/18 + BUN/2.8
|
|
|
Plasma Osmolar Gap Normal
|
Osmolar Gap = Measured mOsm/l - Calculated mOsm/l
Calculated = 2[Na+] + Glucose/18 + BUN/2.8 10-15 mOsm/l |
|
|
substances that increase the osmolar gap
|
Ethanol, ethylene glycol, methanol, acetone, isopropyl ethanol, propylene glycol
|
|
|
What happens to measued sodium levels if lipids or proteins increase too much in plasma?
|
Artifactual hyponatremia (pseudohyponatremia/factitious hyponatremia)
|
|
|
Protein levels of 10 g/dl
|
Exclusively associated with multiple myeloma
|
|
|
Flame photometer
|
In patients with elevated proteins or lipids, Na measured with a flame photometer will have low values
|
|
|
Ion specific electrodes
|
Will give values corrected for waer phase only
|
|
|
How do you treat patients with artifactual hyponatremia?
|
No therapy is needed
|
|
|
Hypo-osmolar Hyponatremia
|
True decrease in plasma sodium
Psychogenic water consumption (poly dyspia) Beer drinkings who eat nothing and become hypoosomoalr -> urine volume increased above normal due to alcohol consumption (carbs in beer become C02 which is blown off an water, so left only w water); they try to excrete as much water as they can but once the urine osmolality reaches its lowest potential vlaue no more water can be excreted and these patients develop edema Osmostat reset: resetting of how we respond to plasma conc which can lead to hypoosolar hyponatrmiea |
|
|
Hypovolemic Hypo-osomolar hyponatremia
|
Water lost from body (Hemorrhage, GI losses, diuretic therapy, primary adrenal insufficiency, 3rd spacing of fluids)
|
|
|
Hypervolemic hypoosomolar hyponatremia
|
Retained water inappropriately (CHF, cirrhosis, nephoritc syndrome, ESRD)
|
|
|
Euvolemic hypoosomolar hyponatremia
|
Myxedema: Different compounds added to compounds that produce edema (GAGs, mucopolysaccharides)
SIADH |
|
|
why does the conc of sodium go up slightly as you go down the proximal tubule
|
some water is reabsorbed with concentration of AA, glucose and bicarbs
|
|
|
osmolarity of intestitial fluid around proximal tubule
|
300 mOsm/l
|
|
|
countercurrent effect
|
the length of the tubule multiplies the horizontal effect
|
|
|
urea recycling
|
urea recycling allows us to concentrate urine at the tip of the ascending portion even though there is no active transport in this part of the nephron
|
|
|
TF/P ratio of 3
|
GT balance = 1/3
|
|
|
osmolarity of the interstitial fluid at the tip of the loop of henle composition
|
made up by urea and sodium
|
|
|
ion movement as you move up ascending limb
|
passive reabsorption of sodium (bc conc of sodium higher in tubular lumne into inteterstitial space down its conc gradient)
passive secretion of urea (bc conc of urea in tubule is lower than interstitium) |
|
|
Two key components of concentrated sodium in thick ascending limb
|
ADH and ACTIVE reabsorption of sodium
|
|
|
Location of 2Cl/Na cotransporter
|
apical membrane of thick ascending cell; energy provided for this from Na/K ATPase pump; when this pump is working effectively it absorbs lots of sodium but water cannot follow bc thick ascending limb is impermeable to water -> this allows water to be osmotically absorbed in collecting duct IF ADH is present due to large Na content in interstitium
|
|
|
what does urea need to get out of collecting duct
|
ADH; if not present the urine will only be 1/2 as concentrated
|
|
|
furosemide
|
blocks 2Cl/Na/K transporter in ascending limb; unable to concentrate interstitial fluid surrounding thick ascending limb; cannot withdraw water from descending limb so fluid at the tip of loop will still be 300 mOsm; as we move up ascending limb nothing happens; we would end up producing an isotonic urine w plasma (300 mOsm)
|
|
|
Which two pumps are critical for our kidneys ability to produce dilute or concentrated urine?
|
2Cl/Na/K pump and Na/K exchanger
|
|
|
If you knock out thick ascnending limb what will urine conc be
|
Low, 300 mOsm
|
|
|
excessive water intake
|
goes into ECF -> descreased plasma conc -> decreased ADH release -> decreased plasma ADH conc -> decreased water reabsorption in kidney -> increased "free water" excretion
|
|
|
primary control effector of ADH release
|
decreased plasma volume; determined by receptors in hypothalamus
decreased venous pressure, venous return and atrial pressure would also lead to increased ADH release |
|
|
Production/storage of ADH
|
Produced in 3rd ventricle of brain in supraoptic nuclei -> stored in posterior pituitary
|
|
|
Primary and secondary stimulus for release of ADH
|
1. Increased ECF concentration
2. a. Increased circulation angiotensin b. decreased pressure in left atrium of heart c. decreased pressure in aortic arch |
|
|
Hypertonic ECF causes what
|
ADH release
this could also be mimicked by hemorrhage or cardiac failure |
|
|
cellcular action of ADH
|
ADH binding -> AC -> cAMP -> AQP2 tranporters in CD = increased free water absorption -> free water returned to ECF -> ECF tonicity decreases -> decreased ADH release
|
|
|
which anatomical site collects the reabsorbed water in descending limb and collecting duct?
|
vasa recta -> renal vein
|
|
|
1. if producing dilute urine (artery vs vein conc)
2. if producing conc urine (artery vs vein conc) |
renal vein must be more conc than renal artery
renal vein must be less conc than renal artery (bc youre absorbing fluid) |
|
|
what is reabsorbed in collecting duct
|
water and urea (as part of the urea recycling system)
|
|
|
free water clearance equation
|
Cosm = Uosm x V / Posm
CH20 = V - Cosm = free water clearance |
|
|
Free water clearance in concentrated urine (above 300 mOsm/l)
|
Negative free water clearance (bc we're absorbing water)
|
|
|
Free water clearance in isomotic urine
|
Free water clearance of 0
|
|
|
Free water clearance in dilute urine (below 300 mOsm/l)
|
will result in a positive free water clearance (bc we're excreting water)
|
|
|
free water clearance definition
|
volume of water that would need to be added to or substracted from each minutes of urines production to make it iso-osmotic with plasma (300)
|
|
|
primary cation in ecf
|
sodium; makes up most of the osmolality
|
|
|
donnon effect
|
proteins in plasma provide negative charge in plasma (more proteins in plasma than interstitial space); VERY slight disequilibrium between the sodium in the plasma and sodium in the interstitium; negative charge of proteins in plasma helps retain some sodium ions in circulating plasma in a conc in excess of what you would see in the interstitial space
|
|
|
main cation in icf
|
potassium (very little sodium); this balance is maintained by Na/K/ATPase pump located on cell membranes
If we destroy this pump we will have significant abnormalities in the function of the heart/nerves/intracellular hydration |
|
|
Intracellular K in acidosis
|
Low; H+ ions move into cell and K move out of cell; can cause hyperkalemia
|
|
|
Intracellular K in alkalosis
|
High; H+ ions move out of cell and K moves into cell; can cause hypokalemia
|
|
|
Intracellular H in acidosis
|
High; H+ ions move into cell and K moves out of cell; can cause hyperkalemia
|
|
|
Intracellular H in alkalosis
|
Low; H+ move out of cell and K moves into cell; can cause hypokalemia
|
|
|
The effect of high or low insulin on intracellular K+
|
Low insulin: K+ leaves cell
High insulin: K+ enters cells (esp. when glucose is present) |
|
|
stop-gap measure to tx hyperkalemia
|
Give potassium and glucose; will drive potassium into cell; however potassium WILL eventually leak back out of cell
|
|
|
effect of high or low aldosterone on intracellular K+
|
Low aldosterone: K+ leaves cell
High aldosterone: K+ enters cell |
|
|
hyperkalemia promotes the release of what to drive it back into cell
|
Insulin, aldosterone, epinephrine (B-agonists)
|
|
|
Potassium levels levels in proximal tubule
|
2/3 of potassium is reabsorbed in proximal tubule, along w/ sodium
|
|
|
potassium transport in low K+ diet
|
Its all reabsorbed
|
|
|
potassium transport in high K+ diet
|
much more is excreted; still 2/3 absorbed in prox tubule, we can secrete much of the filtered load in an attempt to bring the high plasma potassium back to normal
|
|
|
How do loop diuretics and thiazides cause hypokalemia
|
Drugs in the descending loop (furosemide) and distal convoluted tubule (thiazide) inhibit sodium reabsorption; it is later reabsorbed by aldosterone which secretes potassium into the lumen
|
|
|
CHF effect on aldosterone
|
Increased aldosterone; causes Na reabsorption and K secretion; if pt is tx with diuretic MUST watch for hypokalemia since this can compound the hypokalemic efectf
|
|
|
Amiloride
|
Potassium sparing diuretic; inhibits sodium reabsorption in collecting tubules and thus inhibits potassium secretion into lumen
|
|
|
Thiazide
|
Blocks active Na and Cl reabsorption in early distal convoluted tubule
|
|
|
Furosemide
|
Blocks NKCC pump in the ascending loop of Henle
|
|
|
Intercalated cell
|
Alternative to principal cell in the collecting tubules
One of its jobs is to reabsorb K and secrete H+ If the intercalated cell is not working properly we will be unable to properly acidify our urine; this is one of the conditions that will give rise to a renal tubular acidosis |
|
|
RTA Type I
|
Renal tubular acidosis due to damaged intercalated cells (can't secrete H+ into lumen)
|
|
|
RTA Type II
|
renal tubular acidosis type II
decreased bicarb reabsorption in the proximal tubule increased HC03 (and Na+) excretion will result in volume constriction and the increased release of aldosterone. This will increase K+ excretion |
|
|
chronic metabolic acidosis effect on renal potassium
|
Increased renal loss of K+
|
|
|
chronic respiratory acidosis effect on renal potassium
|
increased renal loss of K+ -- due to increased distal delivery of HC03 (high circulating biarb = beyond its transport maximum = distal delivery = potassium losses in body)
|
|
|
chronic metabolic alkalosis effect on renal potassium
|
increased renal excretion of K+ due to decreased amount of hydrogen in cells and increased amount of K; this will increase potassium losses; if plasma bicarb levels are high in chronic metabolic alkalosis we will increase transport maximum, increasing distal Na/bicarb delivery
|
|
|
chronic respiratory alkalosis effect on renal potassium levels
|
increases renal loss of K+ -- usually not severe and not well understood
|
|
|
effects of acidosis on potassium balance
|
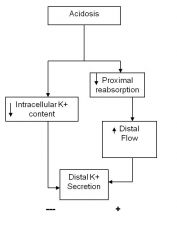
H+ in principal cell, decreased intracellular K+ content, decreased proximal reabsorption
|
|
|
effect of water intake on potassium balance
|
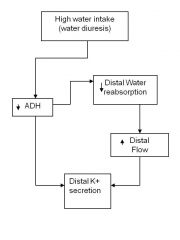
high water intake inhibits ADH which decreases distal potassium secretion; decreased reabsorption of water increases distal flow which could increase the distal excretion of potassium
|
|
|
effect of volume constriction on potassium
|
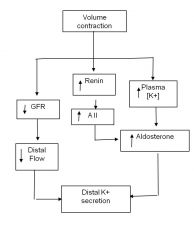
leads to decresaed GFR, decreased GFR, decreases K secretion
BUT also leads to increased Renin, AII, increased Aldosterone -> increased potassium excretion |
|
|
the effect of volume expansion on potassium balance
|
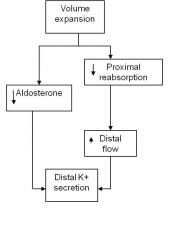
volumee expansion decresaed aldosterone which would decrease K secretion/excretion
it also decresaes proximal reabsorption bc changes GT balance, increase distal flow rate and increase potassium secretion |
|
|
Addisons disease (opposite of cushings)
|
Lack of aldosterone -> sodium and water lost in urine
ppl w addisons have reduced extracellular volume can become hyponatremic, hyperkalemic and mild acidosis |
|
|
tumor related hyponatremia
|
pituitary tumors
SIADH type often in lung, breast, head and neck |
|
|
small cell carcinoma
|
tumors found in lung that lead to production of pseudo-ADH or ACTH
these tumors do not respond to feedback and continue to produce ADH or ACTH regardless of the body fluid volume or concentration |
|
|
SIAD
|
more common in hospital patients and rare in outpatient populations
asymptomatic as long as serum osmols is above 240 msOsm/kg of water mcc of hypotonic (slightly increased plasma volume), euvolemic hyponatremia in children |
|
|
kidney response to CHF
|
release of renin secondary to decresaed perfusion
promotes aldosterone, increased reabsorption of sodium and water in kidney; increased release of ADH to increase water reabsorption tx w drugs to increase cardiac performance and decrease water reabsorption/rid excess water (diuretic) |
|
|
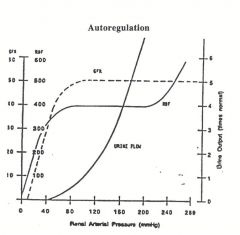
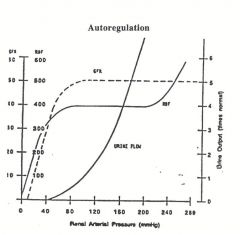
GFR and RBF held pretty constant; (80-160)
there will be an increase in urine formation despite this constant flow; this is called pressure diuresis point: urine flow/excretion of salt increase despite constant GFR and RBF |
|
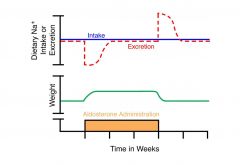
aldosterone escape
|
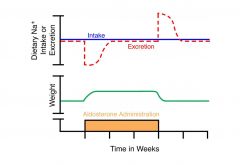
if aldosterone admin exogenously you will see an increase in weight gain bc aldosterone increases sodium/water retention; early phase shortly after administration where excretion of sodium drops (even though intake is constant) - area indicated by hashed line is the amount of sodium retained in the body; along w that sodium is water; therefore plasma sodium conc would not change substantially
after 3-4 days intake/excretion goes back to being equal before aldosterone admin; after we quit giving aldosterone the amount of sodium excreted increases and the extra sodium will be alleviated from body along w water, as noted by the weight returning to normal levels after aldosterone admin stops reasons not well known (maybe naturetic hormone, Na+ regulatory hormone) |
|
|
ANP/BNP effect on GFR
|
increases GFR; increases glomerular pressure by dilating afferent arterioles, constricting efferent arterioles
|
|
|
Angiontensin II in proximal tubule
|
In low concentrations will increase sodium reabosprtion
In high conc. will inhibit reabsorption |
|
|
ANP in prox tubule
|
Inhibits sodium reabsorption via interaction w other hormones
|
|
|
ADH in Loop of Henle
|
Stimulates NKCC transporter; also increases transepithelial NC transport
|
|
|
Paracellin-1 in loop of henle
|
Increases Na+ permeability
|
|
|
PGE2 in DCT
|
Inhibits NC transport
|
|
|
Aldosterone in connecting tubule
|
Stimulates ENaC channels in principal cells
|
|
|
Aldosterone in cortical collecting tubule
|
Aldosterone stimulates ENaC channels
|
|
|
Aldosterone in medullary collecting duct
|
stimulates ENaC channels
|
|
|
Regulation o fK transport in prox tubule?
|
No; no hormones involved; K+ reabsorbed through "pseudosolvent drag" along paracellular pathway
|
|
|
Regulation of potassium transport in loop of henle
|
Active transepithelial K transport across TAL
|
|
|
ADH K transport regulation
|
Activates ENaC increases K+ secretion to inhibit hyperkalemia during dehydration when distal Na delivery is low
|
|
|
AQP2 in DCT
AQP3 in DCT |
On apical membrane (2)
On baseolateral membrane (3) |
|
|
regulation of calcium and phosphate by calcitriol
|

|
|
|
Regulation of calcium balance
|
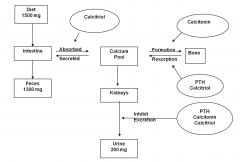
|
|
|
calcium levels in proximal tubule
|
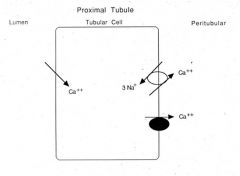
|
|
|
Where is PTH and calcitonin produced?
|
PTH: chief cells of parathyroid
Calcitonin: parafollicular cells of thyroid |
|
|
The Effect of Increased Plasma Phosphate on Bone
|
Plasma phosphate complexes w/ calciu -> decreased serum calcium -> stimulation of PTH -> bone resorption
also decreases calcitriol (since plasma senses enough phosphate) -> less calcium resorption from gut -> further hypocalcemia -> more PTH release weak bones due to increased plasma phosphate |

