![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
185 Cards in this Set
- Front
- Back
|
What are contraindications for PA line?
|
• Vascular access issues.
o The pulmonary arterial catheter goes in through the central venous (IJ, subclavian, or femoral veins). Therefore, any contraindication to venous access (e.g., active bacteremia, coagulopathy, etc.) will be a contraindication for PA line insertion • LBBB o Inserting a PA line can cause RBBB, inducing complete heart block • Acute pulmonary embolism right atrial thrombus, or RV thrombus or mass |
|
|
What is the differential for tall A waves in a PA line pressure tracing?
|
• Tricuspid stenosis
• Pulmonic stenosis • Pulmonary HTN • Cor pulmonale |
|
|
What is the differential for blunting of the Y descent in a PA line pressure tracing?
|
Cardiac tamponade
|
|
|
What is the differential for a prominent X and Y descent in a PA line pressure tracing?
|
• Constrictive pericarditis
• Restrictive cardiomyopathy |
|
|
What is the differential for a prominent C wave in a PA line pressure tracing?
|
1st degree AV block
|
|
|
What is the differential for a prominent C-V wave in a PA line pressure tracing?
|
Tricuspid regurgitation
|
|
|
What is the differential for cannon A waves in a PA line pressure tracing?
|
AV dissociation (can be due to a PVC, complete heart block, AVNRT)
|
|
|
Where in the vascular system is the resistance the greatest?
|
The resistance is greatest in the arterioles. Furthermore, resistance increases with viscosity, length, and radius.
|
|
|
What factors determine preload? Afterload?
|
Preload = EDV, end-diastolic pressure
Afterload = MAP, systemic vascular resistance |
|
|
What are the equations for: 1) MAP 2) Pulse pressure 3) BP 4) CO 5) SV 6) EF 7) Resistance
|
• MAP = (SBP + (2 x DBP))/3
• Pulse pressure = SBP – DBP • BP = CO x TPR • CO = HR x SV • SV = EDV – ESV • EF = SV/EDV • Resistance = pressure / flow |
|
|
What are the primary determinants of SV?
|
• Preload
• Afterload • Contractility • Ventricular mass (greater mass, greater SV) |
|
|
What drugs affect preload?
|
• Venodilators decrease preload
• IV fluids increase preload |
|
|
What drugs affect afterload?
|
• Vasodilators decrease afterload
o Hydralazine, nitroprusside, minoxidil • Vasopressors increase afterload o phenylephrine, vasopressin |
|
|
Can you describe how ventricular compliance is influenced by the following factors: filling volume, wall thickness, ventricular size?
|
• Increased filling volume decreases compliance
• Increased wall thickness decreases compliance • Increased ventricular size increases compliance |
|
|
What are normal values for the pressure in the following areas of the cardiovascular system: RA, RV, PA, PCWP?
|
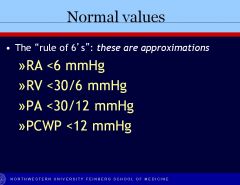
See image
|
|
|
What are normal values for: SV, SI, CO, CI, SVR, PVR?
|
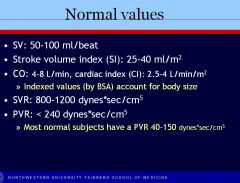
See image
|
|
|
What does the V wave in the PA line pressure wave form represent on an ECG?
|
T wave – ventricular repolarization
|
|
|
What does the C wave in the PA line pressure wave form represent on an ECG?
|
QRS (ventricular depolarization)
|
|
|
What are causes of decreased ventricular compliance?
|
• Increased intrathoracic pressure
• Increased pericardial pressure • Increased pressure or volume of opposite ventricle • Myocardial ischemia • Myocardial disease |
|
|
What are the common hemodynamic profiles in shock for: cardiogenic shock, septic shock, and hypovolemic shock, in terms of RA pressure (CVP), cardiac output, and SVR?
|
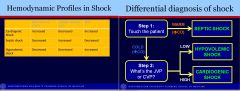
(see table)
|
|
|
What is the “double product?”
|
The double product is (HR x peak systolic BP) and is often used clinically, e.g., in treadmill exercise testing
|
|
|
What is the primary cause of heart attack?
|
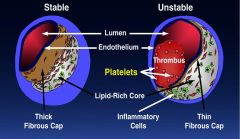
The primary cause of heart attack is the rupture of unstable plaques into vessels that are <70% stenosed and clinically silent.
|
|
|
Can you describe the generation and progression of atherosclerosis?
|
1. Endothelial injury (e.g., oxidized LDL)
2. Monocyte migration, cytokine formation foam cell formation, smooth muscle proliferation, plaque and cap formation 3. Rupture of cap, thrombus formation |
|
|
What are the most important risk factors for stroke (modifiable and nonmodifiable)?
|
• Nonmodifiable
o Age o Sex o heredity • Modifiable o HTN o Cigarette smoking o Hyperlipidemia o Diabetes o Physical inactivity o Obesity |
|
|
What is the definition of angina?
|
Angina is pain or discomfort in the chest or adjacent areas caused by insufficient blood flow to the heart.
|
|
|
How do fibrinolytic agents work?
|
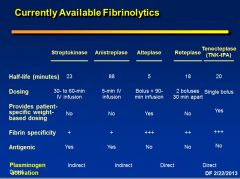
Fibrinolytic agents are a class of drugs known as plasminogen activators, which convert plasminogen into plasmin. Plasmin enzymatically cleaves the fibrin strands, which bind the platelets and red blood cells together within the thrombus, leading to clot dissolution. A naturally occurring serine protease, t-PA is endogenously secreted by the vascular endothelium and helps maintain, along with other hematologic components, a balance between hemostasis and fibrinolysis.
|
|
|
How do statins affect risk of diabetes?
|
• Statins increase risk of diabetes.
• Effect size about 1 in 500 to 1 in 1000 • More likely in older heavier patients. |
|
|
Which statin is not metabolized by the CYP P450 system?
|
• Pravastatin
• CYP 3A4 = LAS – lovastatin, atorvastatin, simvastatin • 2C9 = fluvastatin, less so rosuvastatin, weakly pitavastatin |
|
|
Which statin is the most potent?
|
• Pitavastatin is most potent. After that is…
• Rosuvastatin; has low lipophilicity and high hepatocyte selectivity due to its large polar side chain. Half life of 19 hours, which allows for twice weekly dosing. • Fluvastatin is least potent. |
|
|
What is the mechanism of action for colesevelam?
|
Colesevalam is a bile acid binding gel that binds bile acids in the gut and causes depletion of hepatic cholesterol pools, increasing production of more LDL receptors and thus reducing cholesterol levels in the blood. Bile acid binding sequestrants (older preparations – cholestyramine and colestipol) are among the safest lipid lowering drugs.
|
|
|
Why is Cholestyramine used in digitalis toxicity?
|
Cholestyramine can decrease availability of digoxin tablets by 17-30%.
|
|
|
What is the mechanism of action of niacin?
|
• Niacin is a potent inhibitor of adipose tissue lipolysis (GPCR). It suppresses lipolysis in adipocytes by niacin activating its receptor GPR109A which inhibits lipase, blockingrelease of FFAs.
• Decreases flux of FFA used by liver for VLDL production. • Inhibits VLDL synthesis; see decrease in large TG rich VLDL • Decrease in assemply of apo B containing lipoproteins • See decreased small dense LDL • See increased HDL Apo A-1 o Inhibits hepatic removal o Best drug for raising HDL-c • Reduces Lp(a) – only lipid drug to do this |
|
|
What drug would you use to lower TGs> 500 mg/dL? What are potential side effects of the chosen drug?
|
• Fibrates have major effect on lowering TG levels. Fenofibrate is more potent than gemfibrozil. Also increases HDL if baseline levels are low (5-20%). Used to help prevent pancreatitis.
• Cholelithiasis is a worry with all fibrates; can also cause mild GI symptoms, myositis when combined with statins, must reduce fenofibrate dose with renal impairment • Omega 3 fatty acids are also useful for those with eleated triglycerides in preventing pancreatitis |
|
|
What is the mechanism of action of Omega 3 fatty acids in lipid metabolism?
|
• Omega 3 fatty acids inhibit both hepatic production and utilization of TG rich particles.
• Lower TG in a dose-related fashion • Slightly increase HDL • Don’t use it to lower LDL-c |
|
|
What is ezetimibe, and what is its mechanism of action?
|
Ezetimibe is a cholesterol absorption inhibitor that works by decreasing cholesterol absorption in the intestine; it decreases biliary and dietary cholesterol.
|
|
|
What are major side effects of niacin (nicotinic acid)?
|
• flushing,
• hyperglycemia, • hyperuricemia, can lead to gouty arthritis • upper GI distress, exacerbates peptic ulcer disease • hepatotoxicity |
|
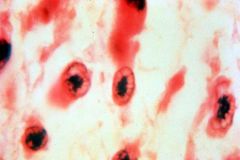
What are these cells, and what are they pathognomonic for?
|
These are Anitschkow cells--activated macrophages--found in Aschoff nodules. They are pathognomonic for rheumatic heart disease. The microscopic lesion of acute rheumatic carditis is the Aschoff nodule, a collection of lymphocytes and histiocytes which is most easily found in the fibrous interstitial septa of the myocardium.
|
|
|
What valves are most commonly affected in rheumatic heart disease?
|
Most of the time it’s mitral that gets affected in rheumatic heart disease, and sometimes also aortic. You probably won’t have aortic valve affected without the mitral valve affected as well.
|
|
|
What’s the most common cause of mitral stenosis?
|

Postinflammatory scarring (likely due to rheumatic heart disease)
|
|
|
Briefly, what’s the pathogenesis of Marfan’s syndrome? What about Ehlers-Danlos syndrome?
|
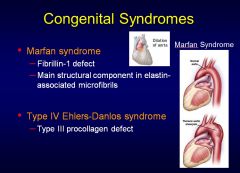
Marfan’s is an inherited connective tissue disorder with a defect in fibrillin. 98% have cardiovascular defects.
Ehlers-Danlos is a congenital defect in type III procollagen. |
|
|
What’s the main cause of sudden death in Wolf-Parkinson-White syndrome?
|
Afib that conducts rapidly over the accessory pathway, degenerating to ventricular fibrillation.
|
|
|
What is the underlying substrate for polymorphic ventricular tachycardia, and what is its mechanism in patients with Long QT syndrome?
|
• Mechanisms for VT may be diverse but are often due to reentry in areas of fibrosis, similar to patients with prior myocardial infarction
• In long QT syndrome, polymorphic VT is likely initiated by triggered activity from early after depolarizations which leads to functional reentry due to dispersion of repolarization. |
|
|
Conceptually, what are 3 strategies for treating rentry?
|
1) Increase the refractory period of the slow conducting tissue that is part of the reentrant circuit
2) Further slow the conduction 3) Suppress the premature beats that often set up the physiology |
|
|
What are examples of drugs that would be used to treat bradycardia?
|
• Atropine
• Epinephrine • Isoproterenol |
|
|
What are the 5 classes of drugs, and what is a representative/prototype drug from each class (include sub-classes)?
|
• Class I – Na+ channel blockers
o Ia – procainamide o Ib – Lidocaine o Ic – Flecainide • Class II – Beta blockers o Metoprolol • Class III – K+-channel blockers o Amiodarone • Class IV – Ca++- channel blockers o Verapamil • Non-classified o Digoxin o Adenosine o Mg++ |
|
|
Can you describe the Na+ channel blocking and K+ channel blocking abilities of the class I drug subclasses?
|
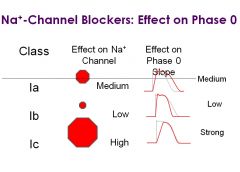
• Na+ Channel blocking
o IB-low o IA-medium o IC-high • K+ channel blocking o IB- none o IC-very low o IA-moderate |
|
|
What are important side effects of procainamide?
|
Procainamide is a class Ia Na+ channel blocker
• Procainamide can cause Lupus in long term therapy, characterized by arthralgia, pleuritis, and pericarditis. Not a real clinical concern since it only occurs with long term administration, and the drug isn’t available PO in the US any longer. However, it may still show up on the boards. • It can cause Torsades de Pointes due to its significant K+ channel blocking activity, prolonging the QT-interval. |
|
|
What are important side effects of quinidine?
|
• Quinidine is a class Ia Na+ channel blocker that can cause cinchonism, CNS toxicity including tinnitus, hearing loss delirium, and psychosis.
• It can cause Torsades de Pointes due to its significant K+ channel blocking activity, prolonging the QT-interval. • It can also cause heart block and faster ventricular response in afib due to vagolytic effects |
|
|
What are important side effects of disopyrimide?
|
• Disopyrimide is a class Ia Na+ channel blocker
• It can cause anti-muscarinic side effects from binding to M2 receptors, including urinary retention, constipation, blurred vision, dry mouth, close-angled glaucoma • It can cause Torsades de Pointes due to its significant K+ channel blocking activity, prolonging the QT-interval. • It can also cause heart block and faster ventricular response in afib due to vagolytic effects |
|
|
What are important side effects of lidocaine?
|
• Lidocaine is a class Ib antiarrhythmic
• It can cause CNS toxicity: confusion, delirium, parasthesias, grand mal seizures |
|
|
What are the major clinical uses of flecainide?
|
• Flecainide is a class Ic antiarrhythmic
• Acute conversison of afib to sinus rhythm • Miantenance of sinus rhythm in afib |
|
|
What are typical side effects of beta blockers?
|
• Bronchospasm
• Depression • Cognitive impairment • Hypotension • Bradycardia • Heart block • Sexual dysfunction in males |
|
|
If a patient were on amiodarone, which lab tests would you be interested in monitoring?
|
• PFTs – can cause pulmonary fibrosis
• LFTs • TFTs – amiodarone is a heavily iodinated compound that also blocks the conversion of T4 to T3. It can cause hypothyroidism and hyperthyroidism • EKG o Can cause sinus bradycardia o Can cause AV block o RARELY causes Torsades de Pointes despite QT prolongation |
|
|
What are the most common side effects of calcium channel blockers?
|
• Constipation and peripheral edema are the most commonly encountered side effects of CCBs.
• Can also get hypotension and some pro-arrhythmic effects (sinus bradycardia, heart block). |
|
|
What is the mechanism of action and therapeutic use for adenosine?
|
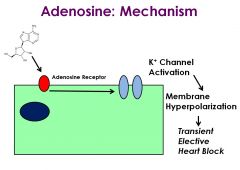
• Adenosine interacts directly with A1 adenosine receptors in the heart, activating K+ channels, indirectly leading to decreases in L-type calcium channel activity and If (the funny current). The net effect is marked hyperpolarization and transient elective heart block.
• It’s used for diagnosis and termination of supraventricular tachycardias (gets rid of QRS complexes so you can see underlying AF or Aflutter) by producing a transient heart block. It’s very effective at terminating reentrant rhythms (e.g., AVNRT, AVRT). |
|
|
What are clinical uses and side effects of digoxin?
|
• Digoxin is used to control ventricular response in atrial fibrillation and atrial flutter, usually in conjunction with a beta-blocker or a CCB
• It can improve contractility in patients with LV systolic dysfunction • Major side effects: disorientation, hallucination, “yellow vision” • Can also cause anorexia, nausea, vomiting • Treatment of digoxin toxicity would include administration of Digibind, anti-digoxin antibody fragments |
|
|
What drugs would be used for rate control in afib and atrial flutter?
|
• Class II – beta blockers – slows conduction through AV node
• Class IV – CCBs – slows conduction through AV node • Digoxin – slows conduction through the AV node |
|
|
What drugs would be used for acute conversion of afib and atrial flutter or maintenance of sinus rhythm in afib or atrial flutter?
|
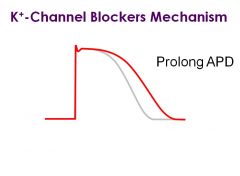
Class Ic – Na+ Channel blockers – slows conduction through Na+ channel block, interfering with reentry
Class III – K+ channel blockers – lengthens AP duration through K+ channel block, interfering with reentry |
|
|
What drugs would be used to suppress symptomatic PVCs, VT in the setting of MI?
|
• Class II – beta blockers can slow conduction in sick (ischemic) tissue
• Class III agents – amiodarone only, interferes with reentry by prolonging repolarization • Class Ib – Na+ channel blockers – lidocaine, mexelitine – interferes with reentry by slowing conduction |
|
|
How would you treat Torsades de Pointes?
|
• Stabilize the electrical membrane with Mg++
• Shorten the prolonged QT interval with isoproterenol and overdrive pacing (pacing the heart rate faster than its native rate). • Electrical cardiovert with phenytoin |
|
|
Where does aortic coarctation occur?
|
It occurs at the level of the ligamentum arteriosum.
|
|
|
What are the 4 components of Tetralogy of Fallot?
|
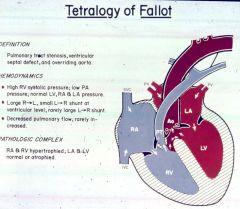
• Infundibular (funnel-shaped) Pulmonary Stenosis
o The outflow tract of the RV, beneath the pulmonary valve, is abnormally formed/developed resulting in stenosis. You get pressure hypertrophy of the RV. • RVH • VSD • Overriding Aorta |
|
|
What are the top 3 main risk factors for vascular disease?
|
• Cigarette smoking
• Diabetes • HTN |
|
|
What are the 3 main PAD symptoms?
|

• Claudication (pain with walking)
• Rest pain (pain at rest) • Tissue loss/ulceration |
|
|
What is the only drug approved for claudication?
|
Cilostazol
|
|
|
What are 3 main symptoms in the clinical presentation of chronic mesenteric ischemia?
|
• Post prandial pain
• Weight loss • Food fear |
|
|
What test is most helpful in diagnosing mesenteric ischemia?
|
CTA; it’s rapid, noninvasive, and you can see the bowel
|
|
|
What are the most common presentations for carotid stenosis?
|
• Asymptomatic
• Transient Ischemic Attack (TIA) • Stroke |
|
|
What’s the difference in the inflammation between atherosclerotic occlusive disease and aneurysmal disease?
|
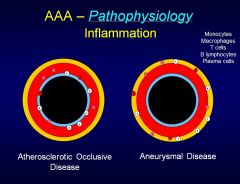
For anureysms, the inflammation is out in the adventitia, while for occlusive disease, the inflammation is in the lumen/intima.
|
|
|
Which MMPs are important for aneurysms?
|
• MMP-2 – elevated in small, stable aneurysms
• MMP-9 – elevated in large, rapidly expanding aneurysms |
|
|
What is the most common etiology for the generation of abdominal aortic aneurysm?
|
Atherosclerotic degenerative disease
|
|
|
What 3 main symptoms are diagnostic for a typical presentation of a ruptured abdominal aortic aneurysm?
|

• Pain
• Hypotension • Pulsatile mass |
|
|
At what diameter of the AAA do you recommend surgical repair?
|
When the aneurysm gets to 5.5 cm diameter—and the risk of rupture exceeds the risk of mortality from surgery—is when you recommend surgical repair.
|
|
|
What are the 2 mainstays of therapy for patients with DVTs?
|
1) Anticoagulation
2) Compression stockings |
|
|
What’s the most common cause of left axis deviation?
|
Left anterior divisional block.
Left posterior divisional block causes right axis deviation. |
|
|
What are the 2 main pathophysiologic mechanisms underlying heart failure symptoms?
|
• Reduced CO
• Elevated filling pressures |
|
|
What do forward failure and backward failure mean?
|
• Forward failure = decreased cardiac output
• Backward failure = increased LV filling pressures |
|
|
What are characteristics of Stage B heart failure?
|
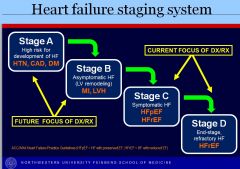
Stage B is asymptomatic HF with some sort of structural defect (e.g., MI, LVH).
|
|
|
What are characteristics of systolic dysfunction?
|
• Implies contractile dysfunction
• Clinically usually manifests as decreased EF • May or may not have signs/symptoms of HF • Does not equal systolic HF |
|
|
What are characteristics of diastolic dysfunction?
|
• Implies slowed relaxation, non-compliant ventricle, or both
• Clinically manifests as increased filling pressures • May or may not have signs/symptoms of HF • Does not equal diastolic HF |
|
|
In which type heart failure do you get concentric hypertrophy? Eccentric hypertrophy?
|
• Concentric hypertrophy – diastolic HF
• Eccentric hypertrophy – systolic HF With systolic heart failure you have lengthening of the myocyte (lower diameter); with diastolic HF, you get thickening of the myocyte |
|
|
Which of the following is not an indication of poor perfusion in HF?
A) Decreased exercise tolerance B) Decreased urine output C) Moderately elevated total bilirubin, alkaline phosphatase D) Cool extremities E) Altered mental status, confusion |
Answer: C) Moderately elevated total bilirubin, alkaline phosphatase
|
|
|
What factors can precipitate acute decompensation in patients with HF?
|
• Increased metabolic demands
o Fever, infection, anemia, tachycardiac, hyperthyroidism, pregnancy • Increased circulating volume (increased preload) o Increased dietary Na+, increased fluid intake, renal failure • Increased afterload o Uncontrolled systemic HTN, pulmonary embolism (increased RV afterload) • Reduced cardiac output o Reduced contractility: myocardial ischemia/infarction, negative inotropes, EtOH o Reduced stroke volume/abnormal heart rate: tachy- and bradyarrhythmias • Medication non-compliance o Most common cause of HF exacerbation/hospitalization |
|
|
Acute pulmonary edema can be a life-threatening situation. How do you treat acute pulmonary edema?
|
• Loop diuretics
• Morphine • Nitrates • Oxygen • Positive pressure ventilation |
|
|
What are the 3 ANCA-associated (pauci immune-associated) vasculitides?
|
1. Wegener Granulomatosis
2. Microscopic Polyangitis 3. Churg-Strauss Syndrome |
|
|
Which vasculitides involve both the lungs and kidneys (alveolar hemorrhage + glomerulonephritis)?
|
• Microscopic polyangiitis (p-ANCA)
• Granulomatosis with polyangiitis (c-ANCA) aka. Wegener’s • Churg-Strauss syndrome (p-ANCA) Others that we aren’t responsible for on the unit 6 exam: • SLE (anti-SM) • Goodpasture’s syndrome (anti-GBM Ab) |
|
|
What two vasculitides that we discussed are associated with mononeuritis multiplex (peripheral neuropathy due to involvement of arteries associated with nerves)?
|
1. Polyarteritis Nodosa
2. Churg-Strauss Syndrome (70%) |
|
|
What vasculitis is associated with young children, fever, conjunctivitis, and desquamative rash?
|
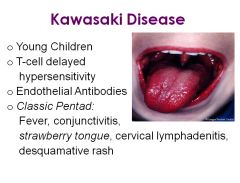
• Kawasaki disease; occurs in children 2-5
• T-cell delayed hypersensitivity • Endothelial Antibodies • Classic Pentad o Fever o Conjunctivitis o Strawberry tongue o Cervical lymphadenitis o Desquamative rash • Untreated: risk of coronary artery ectasia and aneurysms • Treatment = Aspirin 100 mg/kg/day, IVIG **IMPORTANT** |
|
|
What disease is associated with young, heavily smoking males?
|
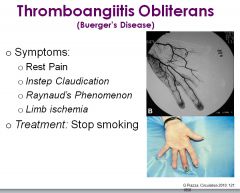
• Thromboangiitis Obliterans (Buerger’s disease)
• Medium-small arteries • Can involve nerve and vein • Very segmental • Tibial and radial arteries most involved • Symptoms o Rest Pain o Instep claudication o Raynaud’s phenomenon o Limb ischemia • Treatment = STOP SMOKING |
|
|
What disease is associated with children less than 10 and palpable lesions on the lower extremities?
|
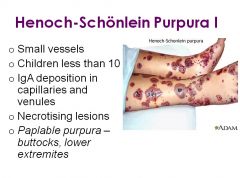
• Henoch-Schonlein Purpura
• Small vessels • Children less than 10 • IgA deposition in capillaries and venules • Necrotising lesions • Paplable purpura – buttocks, lower extremites • Other symptoms o Polyarthralgia w/o arthritis o Abdominal pain o Renal involvement o Often antecedent URI-type illness • Prognosis usually good; usually self-resolving; steroids can help sx |
|
|
Which vasculitides involve the lungs? Kidneys?
|
• Lungs
o Granulomatosis with polyangiitis (Wegner’s granulomatosis) o Microscopicpolyangitis • Kidneys o Microscopic polyangiitis (nephritic syndrome, often RPGN clinically) |
|
|
What epidemiologic populations are affected by Kaposi’s sarcoma?
|
• Classic– elderly Mediterranean men
• Endemic – children in Africa • Transplant-associated – after transplant and immunosuppression • Epidemic – associated with AIDS |
|
|
What vasculitis is associated with patients> 50 years, jaw claudication, and polymyalgia rheumatic (pain or stiffness, usually in the neck, shoulders and hips)? What is the appropriate treatment?
|
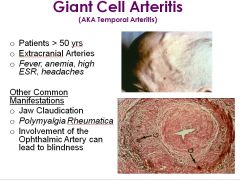
Giant cell arteritis; treat with steroids, which are the mainstay of treatment for temporal arteritis.
|
|
|
What large vessel vasculitis involves the ascending aorta and immediate branches, has constitutional symptoms, and has been described as a “pulseless disease?”
|
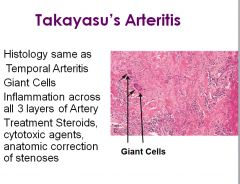
• Takayasu’s Arteritis; associated with Asian women < 50
• Constitutional symptoms • Involves ascending aorta and immediate branches • “Pulseless disease” |
|
|
What disease is associated with PVC manufacturing?
|
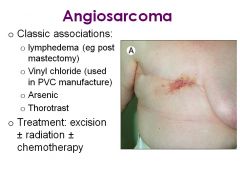
Angiosarcoma (exposure to chemicals such as arsenic or vinyl chloride)
|
|
|
What is microRNA-33’s role in cardiovascular disease?
|
MicroRNA-33 is intronic to the SREBP gene, which codes for a transcription factor critical in the regulation of cholesterol and lipid metabolism. Research suggests that microRNA-33 targeting of ABCA1 diminishes the efflux of cholesterol to HDL. Thus, knockdown of microRNA-33 increases HDL levels (in mice and monkeys).
|
|
|
What artery is most resistant to atherosclerosis (in the context of coronary artery bypass grafts)?
|
The internal mammary artery
|
|
|
How does K+ infusion arrest the heart?
|
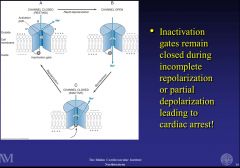
K+ reduces repolarization and stops the inactivation gate of the fast acting Na+ channel, impairing it and resulting in cardiac arrest.
|
|
|
What is distal runoff, and what vessel has the best distal runoff?
|
• Distal runoff is the blood flow in the post stenotic region of a blood vessel
o Distal runoff is an important factor in the success of vaascular grafts o Poor distal runoff promotes thrombosis formation within the graft • Order from best to worst distal runoff’ o 1) LAD o 2)LCX o 3)RCA |
|
|
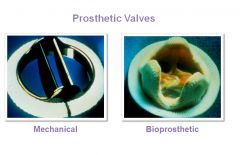
When would you use a tissue valve versus a mechanical valve in surgical repair of valvular disease?
|
Tissue valves are less durable than mechanical valves. For mechanical valves, they need to be on anti-coagulation. If you have an old patient who needs valve replacement, you prefer to give them a tissue valve, because they won’t live long enough to worry about the valve wearing out. A young patient needs a mechanical valve, but they’ll have to live with Coumadin for the rest of their life.
Infective endocarditis is usually treated with an aortic pulmograft from a cadaver. (Cadaveric aortic valve, because there’s no foreign tissue – it’s all human tissue.) |
|
|
What is the most common cause of acute MI?
|
Plaque disruption with thrombus formation is the most common cause of acute MI!
|
|
|
Which of the following is NOT a direct sequelae of an acute myocardial infarction? A) Aneurysm B) Heart Failure C) Arrhythmia D) Aortic Dissection
|
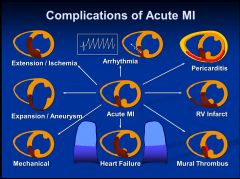
D) Aortic Dissection
|
|
|
What are the 3 criteria for LV enlargement on an ECG?
|
1. S in V1 + R in V5 or V6 > 35 mm
2. R in I + S in III >= 25 mm 3. R in aVL >= 12 mm |
|
|
What are the 4 criteria for RV enlargement on an EKG?
|
1. V1: R wave is larger than S wave
2. V6: S wave is larger than R wave 3. Limb leads: Right axis deviation (axis between 90 degrees and 180 degrees) 4. Usually, right atrial p-wave abnormality is present |
|
|
What is the mechanism of action of nitrates in the treatment of cardiovascular disease?
|
• Mechanism of action—reduce preload, afterload, coronary vasodilation
• Increase in cyclic GMP leads to relaxation of vascular smooth muscle • Preparations o Sublingual—onset in 1 minute; lasts 5-15 minutes o Oral—isosorbide dinitrate short acting (several hours) o Oral—isosorbide mononitrate (short acting and once daily preparations) o Transdermal—patch worn for 12-24 hours; ointment lasts 6 hours • Headaches are a significant side effect |
|
|
What is the mechanism of action of calcium channel blockers in the treatment of cardiovascular disease?
|
• Block calcium channels in vascular smooth muscle, leading to coronary vasodilation, peripheral vasodilation, decreased myocardial contractility, and decreased heart rate.
• Useful for angina, hypertension, and supraventricular tachycardias • Types of CCBs: o Dihydropyridines—amlodipine, nifedipine, nicardipine, felodipine, isradipine o Diltiazem o Verapamil • CCBs can be negatively inotropic, and constipation is a big problem, because they relax vascular smooth muscle in the colon |
|
|
What is the mechanism of action of ranolazine?
|
• Ranolazine helps shut the Na+ inward gate of the late Na+ current, reducing intracellular Na+, providing less substrate for the Na+/Ca++ exchanger
• By inhibiting Na+ and Ca++ overload ranolazine may reduce consumption of ATP, improve contractile function and reduce electrical instability • Ranolazine can increase the QT interval on ECG |
|
|
What are the pathophysiologic sequelae of mitral stenosis?
|
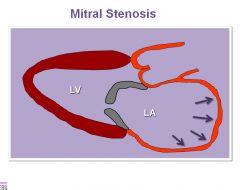
• Pulmonary venous congestion
• Pulmonary arterial hypertension • Right Ventricular Dysfunction • Systemic venous congestion • Low Cardiac Output • Atrial Fibrillation • Systemic embolization |
|
|
What is the classic triad of symptoms of aortic stenosis?
|
1. Dyspnea
2. Angina 3. Presyncope and syncope |
|
|
What are the most common causes of aortic stenosis?
|
1. Congenital (especially bicuspid valves)
2. Degenerative (calcific) 3. Rheumatic |
|
|
What is a normal aortic valve area, and what is the definition of severe aortic stenosis?
|
Normal aortic valve area is > 3.0 sq cm, and severe AS is defined as a valve area < 1.0 sq cm.
|
|
|
Can you explain the paradoxical splitting of the second heart sound?
|
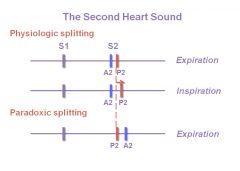
• Paradoxic splitting can occur with aortic stenosis, and P2 occurs before A2 due to delayed emptying of the LV.
• The pulmonic valve is working normally and moves to the right temporally as it should, but since A2 is on the wrong side, you get narrowing of the split upon expiration. |
|
|
When would surgery be recommended for an aortic stenosis patient?
|
Only if there are symptoms; there’s no evidence that aortic valve replacement improves outcome in asymptomatic patients.
|
|
|
What are the sequelae of aortic regurgitation?
|
Aortic regurgitation represents a combination of both increased LV preload and increased LV afterload that leads to:
1. LV hypertrophy and LV dilatation, which compensate for increased afterload but ultimately may lead to LV systolic dysfunction, elevated LV diastolic pressures and pulmonary congestion 2. Widened pulse pressure with elevated systolic BP and reduced diastolic BP |
|
|
How do you treat aortic regurgitation?
|
There’s no established medical therapy for AR other than treating HTN in patients, which could increase severity of AR. Ultimately, patients with severe AR may require surgical aortic valve replacement.
|
|
|
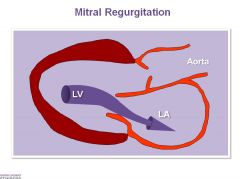
What are the sequelae of mitral regurgitation?
|
Mitral regurgitation represents volume overload of both the LV and LA, leading to:
1. Elevated LA pressure, which may lead to a. Pulmonary venous congestion, which may lead to b. Pulmonary arterial HTN, which may lead to c. RV dysfunction, which may lead to d. Systemic venous congestion 2. LV dilatation, which compensates for increased preload but ultimately may lead to LV systolic dysfunction, which contributes further to elevated LA pressure 3. LA dilatation, which may lead to a. AF, which can lead to b. systemic arterial embolization |
|
|
Does aortic regurgitation cause increased preload or increased afterload?
|
Trick question; aortic regurgitation represents a combination of both increased LV preload and increased LV afterload.
|
|
|
What are the indications for surgery for mitral regurgitation?
|
1. Development of symptoms
2. LV systolic dysfunction 3. Pulmonary HTN 4. Atrial fibrillation In valvular stenosis, it is safe to wait until symptoms to develop before recommending surgery. In valvular regurgitation, in addition to symptoms, one should consider surgery when there is LV systolic dysfunction or severe LV dilatation. |
|
|
What is the leading cause of mitral regurgitation in the USA?
|
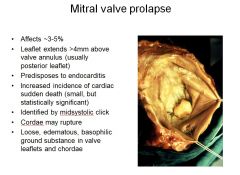
Mitral valve prolapse is a common congenital lesion (up to 5% of the population) and the leading cause of MR in the USA.
|
|
|
Which of the following does NOT create left ventricular hypertrophy:
A) HTN B) Aortic regurgitation C) Mitral regurgitation |
C) Mitral regurgitation does not cause LVH, because it does not increase afterload. Afterload is what causes the muscle to hypertrophy. As soon as the ventricle wants to shorten during MR, it sees an out (a way to relieve its pressure, and thus there’s no increased afterload.
|
|
|
Can you describe the ventricular remodeling that occurs in the following conditions: a) aortic stenosis b) mitral regurgitation c) aortic regurgitation
|
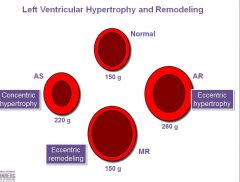
a) In aortic stenosis, there’s concentric hypetrophy due to the increased afterload
b) In mitral regurgitation, there’s dilatation/increased volume but no increase in the wall mass (i.e., no hypertrophy), because there’s no increased afterload c) With aortic regurgitation, there’s eccentric hypertrophy due to an increased dilatation/increased volume as well as an increase in the wall mass due to an increased preload and afterload For aortic valve disease, think Afterload->LVH For Mitral valve disease: think pulmonary congestion and atrial fibrillation |
|
|
What structural change in the aorta can cause aortic regurgitation?
|
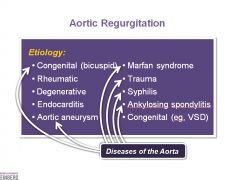
Anything that can make the aorta enlarge can pull apart the valve leaflets and cause aortic regurgitation.
|
|
|
Why do you get an S3 in aortic regurgitation?
|
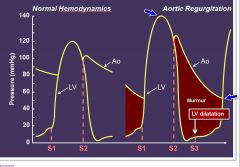
S3s are very common, because you’re dealing with a dilated chamber. (S3 is just a marker of a dilated ventricle.) Another marker of aortic regurgitation is a wide pulse pressure (note the systolic is 140 and diastolic is like 60). You get a decrescendo murmur that starts louder and gets softer.
|
|
|
Generally, what has a poorer outcome, valvular stenosis or regurgitation?
|
In general, stenosis, or narrowing of the valve leading to restriction of outflow leads to a poorer outcome than regurgitation or insufficiency.
|
|
|
What pathogens are the most common cause of infective endocarditis?
|
Most common organisms are Strep. Viridans and staph aureus.
Vegetations are most commonly on valves of the left ventricle. |
|
|
Which layer of the heart is most commonly involved in rheumatic carditis?
|
Rheumatic carditis is a pancarditis, meaning all the layers of the heart are involved – endocardium, myocardium, and pericardium.
|
|
|
What are the Jones criteria for acute rheumatic fever?
|
J – joints (polyarthritis)
O – other (carditis) N – nodules (subcutaneous nodules) E – Erythema Marginatum S – Syndenham chorea |
|
|
Which valve is most commonly involved in nonbacterial thrombotic endocarditis?
|

• The aortic valve is most common, and the mitral valve next most frequently involved.
• Malignancies are found in 50% of cases. • Morphologically, there will be small nodules on lines of valve closure, and the nodules may be bulky and friable. • The valve leaflets are otherwise normal. |
|
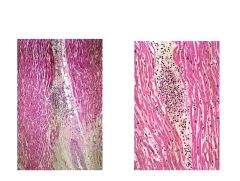
What is this pathognomonic for?
|
• The image shows an Aschoff nodule, which is pathognomonic for Rheumatic Heart disease.
• Aschoff bodies o Fibrinoid necrosis (necrotic collagen) o Mononuclear inflammatory infiltrate (usually T lymphocytes) o Anitschkow cells Histiocytes with vesicular nuclei and abundant cytoplasm Histiocytes are cells that are part of the mononuclear phagocyte system (e.g., macrophage, dendritic cell). |
|
|
Can you describe the murmurs for: a) mild aortic stenosis b) severe aortic stenosis c) mitral regurgitation d) mitral valve prolapse?
|
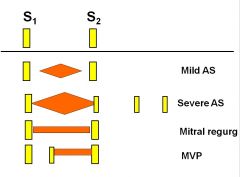
See image
|
|
|
Can you describe the murmurs for: a) mitral stenosis b) mild aortic regurgitation c) severe aortic regurgitation?
|
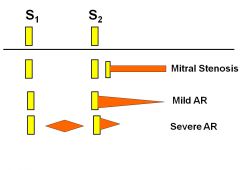
(see image)
|
|
|
What is the most frequent valvular abnormality?
|
• Aortic stenosis
• Acquired>>congenital • Senile calcification, degenerative, “wear and tear”, >10 % due to rheumatic fever • 1-2% congenitally bicuspid • Heaped-up calcified masses in sinuses of valsalva |
|
|
Can you describe the pathophysiology of dilated cardiomyopathy?
|
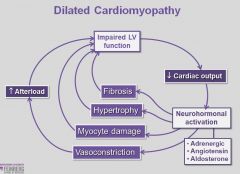
• In DCM, the left ventricle is dilated and systolic pump function is depressed.
o Results in elevated LV end diastolic pressure, LA pressure, and pulmonary venous pressure Causes dyspnea o Reduced cardiac output Causes fatigue and compensatory mechanisms • Activates sympathetic, adrenal , and RAAS systems, which increase systemic vascular resistance o Leads to hypertrophy, apoptosis and fibrosis • Majority of patients who die, die suddenly, presumably from arrhythmic causes |
|
|
Can you describe the pathophysiology of restrictive cardiomyopathy?
|
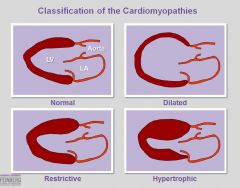
• Conditions that cause infiltrative processes in myocardium are the most common causes
o Amyloidosis o Hemochromatosis o Sarcoidosis o Etc • Thickening and stiffening of ventricular myocardium o Results in restriction of ventricular filling o Reduces forward output o elevates LV and RV filling pressures o results in systolic dysfunction (late manifestation of the disease) |
|
|
Can you describe the pathophysiology of hypertrophic cardiomyopathy?
|
• There’s marked LV hypertrophy, which increases the LV ventricle
o Impairs ventricular filling in disastole and results in small end-diastolic volumes and elevated filling pressures • Myocardial ischemia develops commonly in HCM due to marked myocardial hypertrophy which outstrips the vasodilator capacity of the coronary circulation |
|
|
What type of murmur can you get with dilated cardiomyopathy, and why?
|
You can get a systolic murmur of mitral regurgitation, because the normal heart has the papillary muscles in a unique alignment. In DCM, the papillary muscles have abnormal alignment, causing mitral regurgitation.
|
|
|
What are physical findings for pericarditis?
|
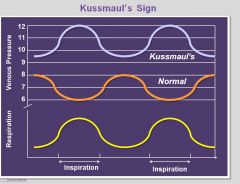
• Kussmaul’s sign
o Increase in venous pressures in the neck on inspiration as opposed to expiration • Jugular venous distention • Pericardial knock |
|
|
What is pulsus paradoxus, and what could it be indicative of?
|
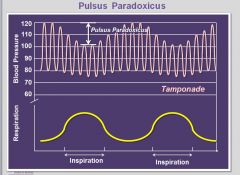
Pulsus paradoxus occurs in cardiac tamponade and reflects exaggerated decreased systolic and diastolic pressures during inspiration.
|
|
|
What is cardiac tamponade?
|
Cardiac tamponade results if more than 250 mL of fluid accumulates in the pericardial space, especially if it accumulates quickly.
Key findings on physical exam include: 1) Jugular venous distension 2) Systemic hypotension 3) A “small, quiet heart” on physical exam 4) Pulsus paradoxus a. Decrease of systolic blood pressure (more than 10 mm Hg) during normal inspirations |
|
|
What is an important parasitic cause of myocarditis?
|

An important parasitic cause of myocarditis is by Trypanosoma cruzi, transmitted by the reduviid bug (which harbors the parasite in its feces). About 20M people in South America are affected with T. cruzi.
|
|
|
What’s the most common primary tumor of the heart?
|
The most common primary tumor of the heart is cardiac myxoma, which commonly (75%) involves the LA or mitral valve, leading to impairment of ventricular filling. Famously, the clinical findings include a diastolic murmur that varies with the patient position since myxomas are ball-like and mobile.
|
|
|
What is the pattern of inheritance for familial hypertrophic cardiomyopathy?
|
Autosomal dominant
|
|
|
What is the equation for transpulmonary gradient, MAP, PVR, SVR, Wall stress?
|
• Transpulmonary gradient = mPAP – PCWP
• MAP = (SBP + (2*DBP))/3 • PVR = [(mPAP - PCWP)/CO]*80 • SVR = [(MAP - CVP)/CO]*80 • Wall stress = (P x r)/2h |
|
|
Can you describe the effect of the Class I, Na+ channel blockers on the action potential duration?
|
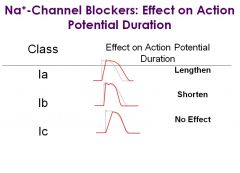
See image
|
|
|
What drug can be useful for treating Hypertrophic Obstructive Cardiomyopathy, and what are its main side effects?
|
You can use disopyramide (class Ia Na+ channel blocker) for treating HOCM, and side effects include antimuscarinic effects (e.g., urinary retention, constipation, blurred vision, dry mouth, closed-angle glaucoma).
|
|
|
Which B-blockers have solely B1 effects?
|
Atenolol and metoprolol
|
|
|
Which B-blockers have alpha and beta blocking capability?
|
Labetolol and Carvedilol
|
|
|
What are the effects of B1-blockade on renin release?
|
B1 blockade also lowers blood pressure by decreasing renin release.
|
|
|
What is the use of alpha 2 agonists like Clonidine in the treatment of cardiovascular disease?
|
Alpha2 agonists like clonidine stimulate the alpha 2 receptor and inhibit NE release from the CNS, causing a decrease in cardiac output and decrease in vascular resistance.
|
|
|
What’s the difference between dihydropyridines and non-dihydropyridine agents (CCBs)?
|
The dihydropyridines (e.g., Nifedipine, Amlodipine, Felodipine) have a more peripheral effect, while the non-dihydropyridine agents (e.g., Verapamil, Diltiazem) also affect the smooth muscle, but have a varying effect on the heart.
In other words, dihydropyridines are selective for vascular smooth muscle and do not affect the heart. |
|
|
What is the mechanism of action of calcium channel blockers (CCBs)?
|
CCBs block the transmembrane Ca++ current, resulting in relaxation of the muscle cell, particularly vascular smooth muscle cells.
|
|
|
What is the mechanism of action of minoxidil?
|
Minoxidil, a peripheral vasodilator that lowers blood pressure by relaxing peripheral vasculature, works by opening K+ channels in smooth muscle cell membranes. That stabilizes the membrane and makes contraction less likely. It dilates arterioles not veins.
Side effects include hypotension, flushing, tachycardia, dizziness, palpitations occur with all peripheral vasodilators. |
|
|
What is the definition of a hypertensive emergency, and what agents are used to lower blood pressure in a hypertensive emergency?
|
A hypertensive emergency is defined as “an acute decompensation of vital organ function secondary to the elevated blood pressure.”
Agents that are used to lower blood pressure in a hypertensive emergency are: • Na+ Nitroprusside • Labetolol • Hydralazine • Enalaprilat • Fenoldapam |
|
|
What is Qp:Qs, and what cutoff is considered an indication for the repair of a shunt lesion?
|
• Qp:Qs is the ratio of flow through the pulmonary circuit (lungs) compared with the flow through the systemic circuit (cardiac output to the body).
• A Qp:Qs of >2 is accepted as an indication for repair of the shunt lesion, because it indicates such excessive pulmonary blood flow that complications will be seen if the shunt lesion is not repaired. • Qp:Qs is measured by cardiac catheterization |
|
|
What is Eisenmenger’s syndrome?
|
Eisenmenger’s syndrome is when there’s an intracardiac L-R shunt, and pulmonary vascular resistance increases to the point that it exceeds the systemic vascular resistance, and the shunt reverses to become a R-L shunt.
|
|
|
Should you close the shunt in a patient with Eisenmenger’s syndrome? Why or why not?
|
You should NOT close the shunt, because that would require all the blood to go through the pulmonary system at high pressure, and the RV isn’t optimized to have high pressure go through there. It’s better to preserve CO and not have perfect O2 saturations.
|
|
|
What is an example of pressure hypertrophy? Volume hypertrophy?
|
• An example of pressure hypertrophy would be aortic stenosis.
• An example of volume hypertrophy would be an atrial-septal defect where blood flows from the LA to the RA. • When myocardium fails, they use the term dilatation |
|
|
What is a normal range for the ankle to brachial index?
|
The ankle to brachial index is a measure of the ratio of the blood pressure in the lower legs to the blood pressure in the arms. Lower blood pressure in the leg is an indication of blocked arteries (peripheral artery disease).
• 0.9-1.2 is normal • Above 1.2 is abnormal vessel hardening from PAD • Less than 0.9 represents PAD |
|
|
Why do emboli lodge in the SMA more than the celiac artery?
|
The SMA has more of an oblique angle, as compared to the acute angle of the celiac.
|
|
|
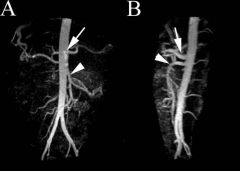
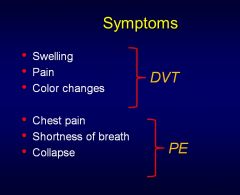
Of the following types of mesenteric ischemia, which has the greatest mortality?
A) Embolic B) Thrombotic C) Nonocclusive D) Venous Thrombosis |
Thrombotic and Nonocclusive have the greatest mortality, although embolic is the most common.
|
|
|
What are the main symptoms for acute mesenteric ischemia?
|
• Sudden pain out of proportion to exam (they’ll be screaming, like the worst pain they’ve ever had)
• Gut emptying • Nausea • Vomiting • Diarrhea |
|
|
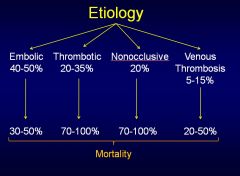
What are types A and B of aortic dissection, and what age groups do they commonly affect?
|
Type A involves the ascending aortic arch, and type B doesn’t.
• 50-60 years of age – Type A • 60-70 years of age – Type B |
|
|
How are aneurysms defined (i.e., what is the criterion for an aneurysm)?
|
• An aneurysm is a localized, blood-filled balloon-like bulge in the wall of a blood vessel.
• An aneurysm is defined as at least a 50% increase in diameter compared with the expected normal diameter. |
|
|
What are protective factors against abdominal aortic aneurysms and what are important risk factors?
|
• Protective
o Female sex o Black race o Diabetes mellitus • Risk factors o Current smoker o Ever smoked o Old age o Family history o Symptomatic atherosclerosis o Hypercholesterolemia |
|
|
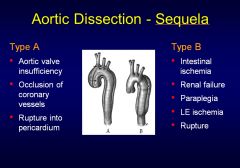
What are the main symptoms for DVT? PE?
|
See image
|
|
|
What vein is the most common to thrombose?
|
Superior mesenteric vein is the most common site of venous thrombosis.
|
|
|
Why does the ventricular wall thicken in systemic hypertension?
|
One of the adaptive mechanisms by which the heart combats the ill-efects of systemic HTN is to increase its wall thickness, which decreases wall stress.
|
|
|
What factors determine ejection fraction?
|
• Preload
• Afterload • Contractility |
|
|
Why do patients with heart failure almost universally have atrial enlargement?
|
It’s due to chronic pressure overload of the atria due to the HF state. Atrial fibrosis accompanies atrial enlargement, which causes atrial arrhythmias such as AF and atrial flutter.
|
|
|
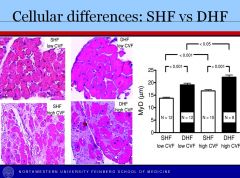
What are important differences between systolic heart failure and diastolic heart failure (besides ejection fraction and filling pressure)?
|
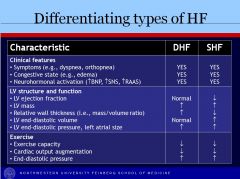
• In DHF, wall thickness is increased while SHF has decreased wall thickness
• In DHF, LV EDV is normal, while it’s increased in SHF |
|
|
Can you describe the different classes of the NYHA functional classification system?
|
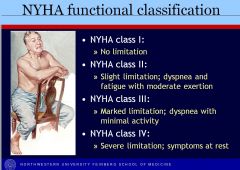
(see image)
|
|
|
What are typical signs/symptoms of CHF?
|
• Symptoms
o Dyspnea on exertion o Orthopnea o Paroxysmal nocturnal dyspnea (PND) o Fatigue o Leg swelling o Abdominal pain/bloating • Signs o Tachycardia o Tachypnea o Elevated JVP o Pulmonary rales o S3 gallop o Increased P2 (in patients with pulmonary HTN) o Hepatomegaly o Peripheral edema |
|
|
How do you treat someone who’s warm and wet? Cold and wet? Cold and dry?
|
• Warm and wet (67% of patients): congested with good perfusion; diuresis is most important. Uptitrate and ensure treatment with other life-saving heart failure medications (e.g., beta-blocker, ACE-inhibitor/ARB, and spironolactone)
• Cold and wet (28%) – congested with poor perfusion; these patients cannot undergo successful diuresis until their perfusion improves. Vasodilators are the mainstain of therapy in this situation. Inotropes can also help, but these agents increase mortality, so use with caution (can be used as a bridge to ventricular assist device or cardiac transplantation). • Cold and dry (5%) – no congestion but poor perfusion; these patients are typically end-stage HF patients and require increased vasodilator and/or inotropic therapy. Consider ventricular assist device and/or cardiac transplantation in these patients. |
|
|
Of the IV vasodilators, nitroglycerin and nesiritide, which can be used in hypotensive patients?
|
Nesiritide (recombinant BNP) is a natriuretic peptide and promotes natriuresis, but also acts as a potent vasodilator. It should NOT be used in hypotensive patients. Nitroglycerin and nesiritide can generally be used in patients who are “warm and wet,” but should be used with caution in patients who are “cold,” because they can acutely worsen hypotension.
I think it’s okay to use nitroglycerin, but nitroprusside is the vasodilator of choice if the patient is cold, because it won’t decrease preload as much as other agents. |
|
|
What is the optimal range for digoxin, and why can hypokalemia increase digoxin levels?
|
• The optimal range for digoxin is 0.5 – 0.8 ng/mL, which is below the usual therapeutic range. Above this dose, digoxin increases mortality.
• Hypokalemia can increase digoxin levels since digoxin normally competes with K+ ions for the same binding site on the Na+/K+ ATPase pump. |
|
|
Can you use beta-blockers for CHF patients?
|
Beta-blockers improve survival and outcomes in systolic HF by combating the maladaptive neurohormonal response that occurs n HF.
|
|
|
What are the determinants of stroke volume?
|
Contractility (increased) - anything that increases intracellular calcium
Preload (increased) Afterload (decreased) |
|
|
What’s the most common type of congenital cyanotic disease?
|
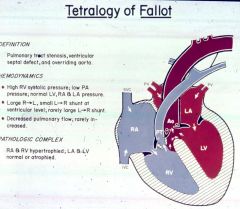
Tetralogy of Fallot
|
|
|
At what level of narrowing in obstruction do you start to see problems?
|
65%
|
|
|
What class of drugs are the treatment of choice for Prinzmetal's angina (angina caused by vasospasm)?
|
CCBs are the treatment of choice for Prinzmetal's angina. They cause vasodilation of the coronary arteries and peripheral resistance arteries.
|
|
|
What are the 3 major determinants of myocardial O2 demand?
|
The 3 major determinants of myocardial O2 demand are:
1) Ventricular wall stress a. Related to ventricular pressure and the radius of the ventricle and inversely proportional to the wall thickness, wall stress is the tangential force acting on the myocardial fibers, tending to pull them apart, and energy is expended in opposing that force 2) Heart rate a. The amount of ATP consumed per minute increases with heart rate and so do the O2 requirements. Conversely, slowing the HR with a beta blocker decreases ATP utilization and O2 consumption 3) Contractility |
|
|
What is the equation for the Fick principle version of cardiac output?
|
CO = rate of O2 consumption/(arterial O2 content - venous O2 content)
|
|
|
What is the definition of syncope?
|
Syncope is defined as transient loss of consciousness with loss of postural tone. Some include that it is also due to decreased cerebral blood flow. It’s important to distinguish syncope from:
• Vertigo • Seizures • Falls Syncope can be associated with a prodrome of dizziness but not with a sensation of motion. |
|
|
Can you give a broad pathophysiological diagnosis of syncope?
|
• Neurally-mediated Syncope (25%)
o Bradycardiac (cardio-inhibitory) o Hypotensive (vaso-depressor) o Vasovagal (mediated by emotional distress, fear, pain, etc.) o Situational (cough, sneeze, GI stimulation, micturition, post-prandial, etc.) o Carotid sinus syncope (hypersensitivity of carotid body to pressure) • Cardiac Arrythmias (14%) o Brady and tachy-arrhythmias are the most common serious cause of syncope • Neurologic Disease (10%) o Seizure disorders o Syncopal migraines o TIAs or strokes • Postural Hypotension (8%) o Primary etiology is volume depletion or autonomic failure • Cardiovascular mechanical disorders (4%) o Could be due to PE o Aortic stenosis can reduce ability to increase CO during exercise • Metabolic and Toxic causes (3%) o Narcotics, phenothiazines, and recreational drugs are most commonly associated drugs • Psychiatric disrorders (2%) • Unknown (34%) |
|
|
What is the equation for BP that relates HR, SV, and SVR?
|
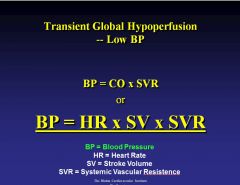
see image
|

