![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
Hydrochlorothiazide
|

Diuretic; decrease volume of blood; block renal Na resoprtion (natriuresis) and thereby causing dieresis (loss of water) from the blood.
|
|
|
Amlodipine
|

Vasodilation; calcium channel blocker; calcium channel blocker that directly acts in the vascular smooth muscle to cause vasodilation and also acts in the heart to decrease cardiac output.
|
|
|
Captopril
|

Decrease blood volume AND vasodilation; ACE inhibitor; Angiotensin converting enzyme (ACE) inhibitor which blocks the formation of antiotensin II and blocks the inactivation of bradykinin. The blockade on angiotensin II formation limits the vasoconstriction and stimulation of aldosterone release while the blockade of bradykinin inactivation allows continued bradykinin-induced vasodilation.
|
|
|
Losartan
|

Angiotensin receptor blocker; decreases blood volume AND vasodilation; Angiotensin II receptor antagonist (or blocker also called ARB for Angiotensin Receptor blockers) that blocks the actions of angiotensin II to cause vasoconstriction and aldosterone release.
|
|
|
Clonidine
|

Central acting alpha-2 agonist; decrease sympathetic stimulation to heart and vasculature; alpha-2 adrenergic agonist that works within the CNS to decrease overall (heart, resistance arterioles and capacitance venules) cardiovascular sympathetic stimulation from the CNS (sympathoplegics).
|
|
|
Prazosin
|

Alpha 1 antagonist; decrease sympathetic stimulation to vasculature; alpha-1 adrenergic antagonist that decreases blood pressure by blocking alpha-1 receptors in resistance arterioles and capacitance venules and thereby affecting both cardiac output and total peripheral resistance.
|
|
|
Metoprolol
|

Beta adrenergic antagonist (beta blocker); decrease sympathetic stimulation to the heart;beta-1 adrenergic antagonist that decreases blood pressure by blocking beta-1 receptors primarily in the heart and secondarily in the kidney.
Beta blockers can also block release of renin (secondary affect) |
|
|
Hydralazine
|

Direct vasodilator; acts directly on smooth muscle cells of arterioles (much more than veins);a direct acting arteriole-specific vasodilator that may cause nitric oxide release and that causes decreases in blood pressure by effects on total peripheral resistance.
|
|
|
Nitroprusside
|

NO releasing drugs; vasodilation; powerful dilator of both veins and arterioles; breaks down to release nitric oxide (NO) which directly acts on vascular smooth muscle relaxation.
|
|
|
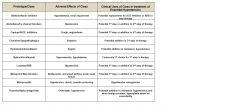
Adverse effects/antihypertensive clinical uses of aliskirin/renin inhibitor?
|

|
|
|
Adverse effects/antihypertensive clinical uses of amlodipine/Ca channel blockers?
|

|
|
|
Adverse effects/antihypertensive clinical uses of captopril/ACEinhibitor?
|
|
|
|
Adverse effects/antihypertensive clinical uses of captopril/ACEinhibitor?
|
|
|
|
Adverse effects/antihypertensive clinical uses of clonidine/sympathoplegics?
|

|
|
|
Adverse effects/antihypertensive clinical uses of hydralazine/vasodilators?
|

|
|
|
Adverse effects/antihypertensive clinical uses of hydrochlorothiazide?
|

|
|
|
Adverse effects/antihypertensive clinical uses of losartan/ARB?
|

|
|
|
Adverse effects/antihypertensive clinical uses of metoprolol/B-blockers?
|

|
|
|
Adverse effects/antihypertensive clinical uses of nitroprusside?
|

|
|
|
Adverse effects/antihypertensive clinical uses of prazosin/alpha antagonists?
|

|
|
|
What are two pathological reasons for poor response to antihypertensive therapy?
|
Sleep apnea and secondary hypertension
|
|
|
What are some pharmacological reasons for poor response to antihypertensive therapy?
|
Non adherence, suboptimal antihypertensive dose, suboptimal choice of drugs, dietary components that promote hypertension (salt, licorice)
|
|
|
What is the target HTN tx blood pressure in absence of complicating comorbidities?
|
< 140/90 mmHg
|
|
|
What is the target HTN tx blood pressure in presence of complicating comorbidities
|
< 130/90 mmHg
In presence of heart failure = < 120/80 mmHg |
|
|
What are some complicating comorbidities to hypertension?
|
Diabetes, kidney disease, coronary heart disease, heart failure
|
|
|
Why does dopamine act on adrenergic receptors?
|
It's chemically similar to norepinephrine and epinephrine since it's a catecholamine; thus has some binding affinity for adrenergic receptors
|
|
|
Dose dependent nature of dopamine
|
Low dose - D1
Higher dose - B1 agonist (increases cardiac output, opposite of beta blockers) Very high dose - A1 (peripheral vasoconstriction) |
|
|
Aliskirin
|

Renin inhibitor which limits the formation of Angiotensin I. This blockade limits angiotensin II vasoconstriction and angiotensin II stimulation of aldeosterone secretion.
|
|
|
Explain why diuretics are an appropriate 1st line therapy for most patients confirmed as having essential hypertension not responding to lifestyle interventions
|
Reducing the Na load decreases mean blood pressure by 10 to 15 mm Hg in most patients. Other agents that affect either vasoconstriction and/or sympathetic nervous system components tend to become compensated for by increasing Na load. Thus, in mild to moderate hypertension diuretics tend to function alone better than other agents.
|
|
|
Low DA dose
|
'pure' dopamine respeonse; vasodilation of arterioles of the renal and splanchnic region; this is due to binding of DA to D1R in those vascular regions
|
|
|
Intermediate DA dose
|
this dose is high enough to allow binding to DAR and B1R; this causes cardiac manifestations of increased force and rate of heart contractions
|
|
|
High DA dose
|
Additional stimulation of alpha-1 adrenergic receptors and vasoconstriction throughout the body
|
|
|
Digoxin
|
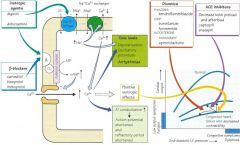
Cardiac glycoside; Inhibitors of Na+, K+ ATPase cause cardiac cells to
accumulated Na+ inside the cell. This increases the movement of Na+ out and Ca+2 into the cell by the antiport exchanger on the cardiac cell surface. The increased Ca+2 causes increased force of contraction. Thus cardiac glycosides force the heart to work harder. These agents are used as a 4th stage of therapy when the patient is in Class III or IV (Stage C or D) heart failure. They have been shown to decrease hospitalizations but not decrease death rate. |
|
|
Dobutamine
|
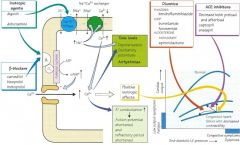
Beta adrenergic agonist; stimulation of the beta receptor of the heart forces the heart to increase rate and force of contraction. These agents increase
cardiac oxygen demand and may initiate arrhythmias due to the beta adrenergic receptor activation. |
|
|
Carvedilol
|
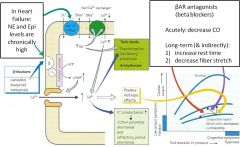
Beta adrenergic antagonist; decrease HR and FOC;
second step of therapy when added to ACE inhibitors or in combo with ACE inhibitors a component of the first step of therapy |
|
|
Furosemide
|
Loop diuretic; decrease blood volume thus decrease preload; most efficacious diuretics available;
Can cause hyponatremia, hypokalemia and electrolyte imbalances |
|
|
Furosemide
|

Loop diuretic; decrease blood volume thus decrease preload; most efficacious diuretics available;
Can cause hyponatremia, hypokalemia and electrolyte imbalances |
|
|
Spironolactone
|

Aldosterone antagonist; act in collecting tubules of kidney at aldosterone R to cause mild diuresis and block K+ excretion. Can minimize potential for hypokalemia caused by other diuretics.
Can cause hyperkalemia an care must be taken when used in combination with ACE inhibitors |
|
|
Captopril
|

ACE Inhibitors; Inhibit formation of AII, decrease breakdown of bradykinin; decrease vasoconstriction (by decreased AII) and stimulate vasodilation (by increased bradykinin) as well as decrease blood volume (by decreasing AII and thus less release of aldosterone).
First choice therapy in omst causes of heart failure |
|
When are beta adrenergic antagonists appropriate to use to tx heart failure?
|
Chronic heart failure - need to let heart rest and decrease oxygen demand
|
|
Explain why β‐adrenergic receptor antagonists must not be discontinued abruptly and why it is important monitoring heart rate, blood pressure, and body weight while taking these agents.
|
BAR antagonists increase # BARs (upregulation) on heart -> abrupt discontinuation = excess stimulation by unopposed NE (or Epi) - Arrythmia and Heart Failure
|
|
|
Give example of select heart failure patient situations where cardiac glycoside could be beneficial but why monitoring serum potassium is important when they are used.
|
Examples
To support renal, hepatic or coronary perfusion. If need positive inotrope with negative chronotrope Monitoring of K+ Therapeutic Index very low (- ~ 2) |
|

Identify heart failure patient situations where a loop diuretic could be beneficial over thiazide diuretic and why potassium sparing diuretics such as aldosterone receptor antagonists should be considered to be used.
|
Loops versus thiazide diuretics
Efficaciousness Addition of potassium sparing diuretics With digoxin – avoid hypokalemia-induced problems Severe CHF – add on to therapy – increase survival & reduce hospitalization |

