![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back

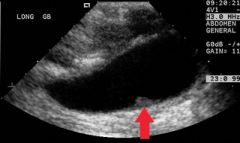
Gross pathology reveals black lumps in the gallbladder.
|
Pigmented cholethiasis (gallstones)
|
|

What is acalculous cholecysitis?
|
Ischemia due to cysic artery obstruction secondary to inflammation or edema which comrpomies blood flow
|
|
Acute calculous cholecystitis
|
Chemical irritation and inflammation of the obstructed gallbladder (due to gallstones)
Bile salts are often irritating exposed mucosal walls |
|
|
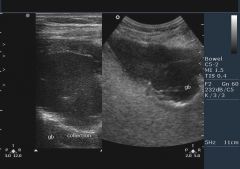
87yo M critically ill, on long-term TPN w RUQ pain. Abdomen is tender. Murphy’s sign elicited. No similar episodes in past. Ultrasound: No GB wall thickening, pericholecystic fluid present, no gallstones. Diagnosis: ?
|
Acute acalculous cholcystisis
|
|
|
Choledocholiathiasis
|
Stones within the bile ducts of the biliary tree
|
|
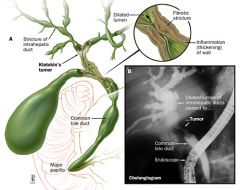
Cholangitis
|
Narrowing of bile duct; could be secondary to bacterial infection, inflammation, tumor or gallstone
|
|
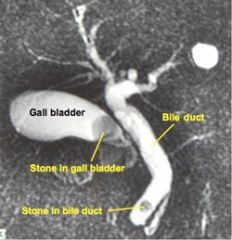
46yo F p/w RUQ pain, jaundice, acholic stools, dark tea-colored urine, no fever. Past history of cholelithiasis. No treatment ever undertaken. Exam: unremarkable. HepB/C neg. Ultrasound: solitary CBD stone, dilated CBD > 1cm. Diagnosis: ?
|
Choledocholiathiasis
|
|
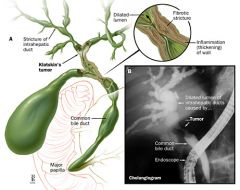
46yo F p/w fever, RUQ pain, acholic stools, dark tea-colored urine.
If also altered mental status and signs of shock = Raynaud’s pentad |
Ascending cholangitis
|
|
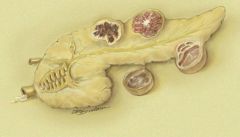
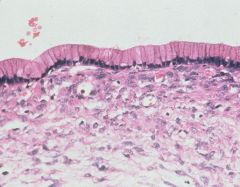
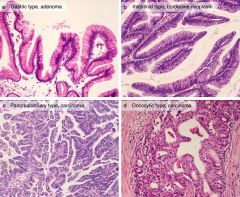
72 yo F p/w mild RUQ pain since last several months. She also complains of intermittent episodes of acute colicky pain. She gives past history of gall stones. Her last U/S taken 2 years ago reveal thickend gall bladder, with multiple stones. No pericystic fluid was observed. CBD was not affected. Her present U/S reveals an infiltrative mass occupying most of the gall bladder. Also noticed are gall stones. Cholecystectomy was performed. Gross and histo-pathology are shown. Diagnosis?
|
Carcinoma of the gallbladder
|
|
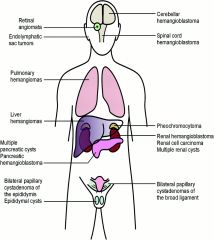
Von Hippel Lindau disease
|
vascular neoplasms found in the retina, cerebellum or brain stem in association with congenital cysts in the pancreas, liver and kidney
|
|
|
How can you histologically determine a cyst?
|
Cyst lacks a true epithelial lining and is lined by fibrin and granulation tissue
|
|
|
A 20-year old woman was first admitted with nausea, weakness, vomiting, dizziness, and visual disturbance. The findings of a fundoscopy were normal, but a CT scan showed a cerebellar tumor in the posterior fossa, which was removed. Histopathologic examination confirmed a cerebellar hemangioblastoma. The patient remained completely asymptomatic until 4 years later, when she presented again with vomiting and dizziness. On admission, an abdominal CT scan showed a 14X10-cm, well circumscribed, thin-walled cyst in the head of the pancreas, and multiple smaller cysts in the tail and body region of the pancreas. She also had bilateral ovarian cysts.
|
Von Hippel Lindau Disease
|
|
|
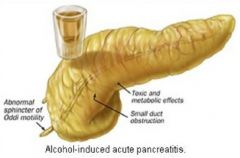
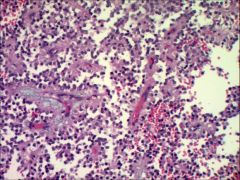
Acute pancreatitis
|
Reversible pancreatic parenchymal injury associated with inflammation
|
|
|
What two laboratory findings wil you find in acute pancreatitis?
|
Marked elevation of serum amylase levels during the first 24 hrs followed by rising serum lipase levels in 72-96 hours.
|
|
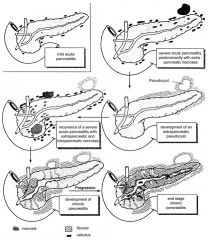
Chronic Pancreatitis
|
Inflammation of the pancreas with irreversible destruction of exocrine parenchyma, fibrosis, and in the late stages, the destruction of endocrine parenchyma.
|
|
|
What is the most common cause of chronic pancreatitis?
|
Long term alcohol abuse
|
|

What happens to the pancreas of an alcoholic in chronic pancreatitis?
|
Elevated protein concentrations form ductal plugs which calcify; contribute to chronic pancreatitis
|
|
Mucinous Cystic Neoplasm
|
95% arise in women associated with invasive carcinoma; often at body or tail
|
|
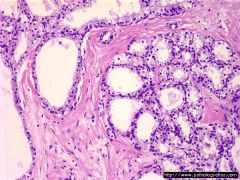
Histology of Mucinous cystic Neoplasms (Mucinous Cystadenoma)
|
Lined by columnar mucinous epithelium
|
|
Serous Cystadenoma
|
Benign cystic neoplasms composed of glycogen rich cuboidal cells surroudning small cysts containing clear, thin, straw colored fluid
|
|
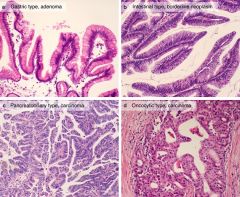
Intraductal Papillary Mucinous Neoplasms
|
arise more frequently in men then women, involve the head of the pancreas instead of the tail
|
|
Histology of Intraductal Papillary Mucinous Neoplasms
|
Lack the dense ovarian stroma and involve a larger pancreatic duct
|
|
|
Solid Pseudopapillary Neoplasm
|
Large, well circumscribed pancreatic masses with solid and cystic components
|
|
Histology of solid pseudopapillary neoplasm
|
Grows in solid sheets or papillary projectoins
|
|
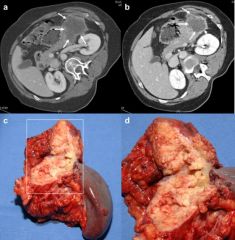
Pseudocysts
|
Often manifests as a sac between the stomach and pancreas; usually arise after acute pancreastitis (often chronic alcoholic pancreatitis)
Hapens when body walls of peripancreatic hemorrhagic fat necrosis with fibrous tissue |
|
CA 19-9 Use
|
Pancreatic cancer marker
|
|
|
What causes cholelithiasis?
|
Supersaturation of bile with cholesterol (cholesterol stones) or bilirubin salts (pigmented stones) promotes stone formation
|
|
|
A jaundice patient with a history of gallstones suggests what?
|
common bile duct obstruction (choledocholiathiasis)
|
|
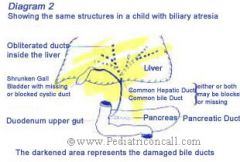
biliary atresia
|
complete obstruction of bile flow due to destruction or absence of some part of the extrahepatic bile ducts (most common cause of liver failure death in early childhood)
|
|
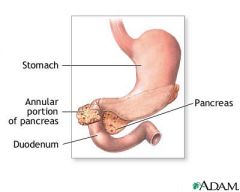
annular pancreas
|
pancreatic tissue completely encircles the second portion of the duodenum; can cause duodenal obstruction
|
|
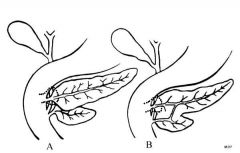
pancreas divisum
|
failure of fusion of the ventral and dorsal pancreatic primordia; causes secretions to drain only through
|
|
|
which enzyme is inappropriately activated in pancreatitis?
|
trypsin, which goes on to activate other enzymes
|
|
|
What is the function of the cationic trypsinogen gene PRSS1?
|
PRSS1; codes for a failsafe site on trypin critical for its own activation; if its trypsin will be hyperactive and cause pancreatitis
|
|
|
What is the function of serine protease inhibitor, kazal type 1 (SPINK1)?
|
mutation leads to a defective protein that can no longer inactive trypsin, resulting in pancreatitis
|
|
|
A pt has a positive urease breath test. Is the organism h. pylori or c. jejuni?
|
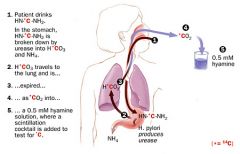
H. pylori
|
|
A pt has a positive H2S production test. Is the organism h. pylori or c. jejuni?
|
C. Jejuni
|
|

A pt has a positive nitrate reduction test with an organism that grows at 42C (NOT 37C). Is the organism h. pylori or c. jejuni?
|
C. Jejuni
|
|
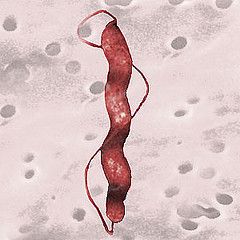
Compare the morphology of h. pylori with c. jejuni?
|
h. pylori: spiral w/ 3 unipolar flagella
c. jejuni: comma shaped or "gull winged" with bipolar flagella |
|
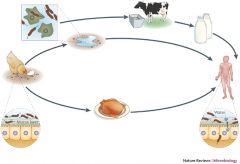
How is c. jejuni transmitted?
|
Zoonotic: Poultry, dogs, cattle, sheep
|
|
|
What is notable about the c. jejuni incubation temperature?
|
Needs 42C, compared to h. pylori which needs 37C
|
|
Compare the disease course of c. jejuni and c. fetus?
|
c. jejuni: gastroenteritis
c. fetus: systemic intravascular and extraintestinal infections |
|
|
How might you differentiate between c. jejuni and c. fetus?
|
only c. jejuni can grow at 42C, c. fetus needs 37C (similar to h. pylori)
|
|
|
What does the S-protein virulence factor for c. fetus do?
|
Helps the organism evade the immune system
|
|
|
Tx of choice for campylobacter infections?
|
Erythromycin (broad spectrum); eliminates carriage in 72 hours
|
|
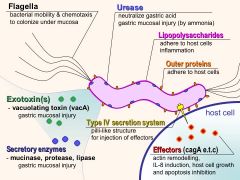
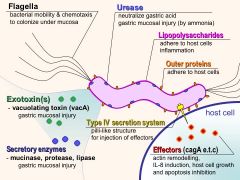
What is the function of LPS O side chain in h. pylori?
|
Resembles the blood group antigens so it protects the bacteria from immune clearance
|
|
|
What si the gold diagnostic standard for h. pylori?
|

Histological examination of gastric biopsy
|
|
|
A patient taking antibiotics, pepto bismal, and PPI has stomach ulcers but comes back negative for h. pylori via rapid urease test. What might be happening?
|
The drugs he's taking have decreased the h. pylori load making producing false-negative results.
|
|
|
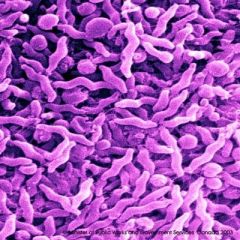
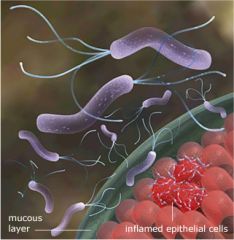
Why does h. pylori being microaerophilic help it grow in the stomach
|
It can grow extremely well in the ciscous mucus layer that coats the gastroepithelium
|
|
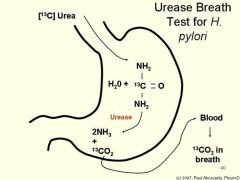
How does the production of urease by h. pylori help it?
|
A byproduct of urease activity, ammonia, neutralizes gastric acids in the local vicinity
|
|
|
A mutation in h. pylori hop genes would result in what?
|
An inability of h. pylori to withstand peristalsis or mucosal shedding. (i.e. these genes are adherence genes0
|
|
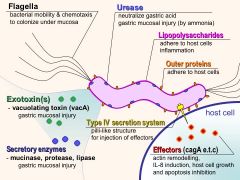
What does the VacA virulence factor on h. pylori do to cells?
|
(Vacuolating toxin; causes swelling of cellular compartments)
|
|
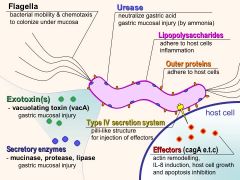
What does the Cag virulence factor on h. pylori do to cells?
|
Cytotoxin associated gene; IL8 induction via Type IV Secretion system for Cag entry attracts inflammatory cells = cell damage
|
|
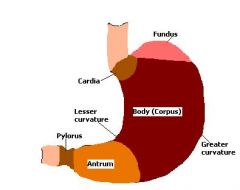
Where will h. pylori be dominant in the stomach of an individual with low acid output (for ex. someone on ppi)?
|
Corpus Predominat Gastritis (body)
|
|
Where is h. pylori normally more pronounced in most patients?
|
Antral predomiantn; higher acid production in body and fundus which is inhibitory to bacterial growth, so it settles in the antrum
|
|
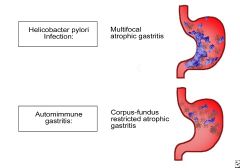
Which h. pylori gastritis pattern is seen in individuals who develop gastric carcinoma and gastric ulcers?
|
Multifocal atrophic gastritis (corpus, fundus, antrum)
|
|
|
What is the triple combo tx for h. pylori infection?
|
PPI, clarithryomycin, beta lactam (amoxicillin) for 7 to 10 days
|

