![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
116 Cards in this Set
- Front
- Back
|
A patient presents with the urge to vomit. How would you describe this symptom?
|
Nausea
|
|
|
A patient forcefully expels gastric contents through the mouth. What symptom is this?
|
Vomiting
|
|
|
A neonate effortlessly moves stomach contents into the esophagus and mouth. What symptom is this?
|
Regurgitation
|
|
|
A patient presents with spasmodic movements of the respiratory muscles against the closed glottis and contractions of the abdominal muscles. You note no expulsion of gastric contents. What is the patient doing?
|
Retching
|
|
|
A patient chews and swallows some regurgitated food that has come back to the mouth after a recent meal. What is this called?
|
Rumination syndrome
In animals it allows them to eat quickly and chew later while it's resting; it's generally an involuntary eating disorder in humans |
|
|
A patient presents with nausea and vomiting that has been occurring for more than a month. Is this chronic or acute?
|
Chronic
|
|
|
A patient presents with nausea and vomiting that has been occurring for less two weeks. Is this acute or chronic?
|
Acute
|
|
|
Which vomiting regulation center is located on the floor of the fourth ventricle and contains a chemoreceptor 'trigger zone' sensitive to drugs, toxins, and neurotransmitters?
|
Area postreme
|
|
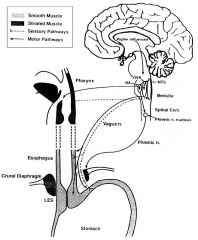
Which vomiting regulation center is located in the medulla and serves as a 'central pattern generator' accepting information from area postrema and n. vagus, and projects to motor nuclei to evoke muscle reactions?
|
Nucleus tractus solitarius
|
|
|
A patient presents with watery diarrhea, abdominal cramps and vomiting. Patient reports having drank water from a natural source that has not been filtered or boiled. What is the likely organism?
|
Cryptosporidium
|
|
|
A patient presents with acute abdominal pain that radiates to the back.
|
Pancreatitis
|
|
|
A patient presents with bloody vomiting. What should you suspect?
|
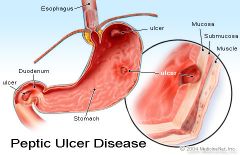
Peptic ulcer
|
|
|
A patient presents with bilious vomiting.
|
Proximal small bowel obstruction
|
|
|
A patient presents with feculent vomitus.
|
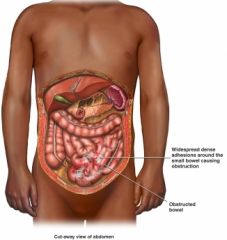
Distal small bowel obstruction
|
|
|
A patient presents with vomiting food that was eaten more than several hours previously and is only partially digested.
|
Gastric retention
|
|
|
A patient presents with projectile vomiting.
|
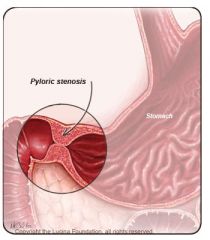
Pyloric stenosis; also seen in increased intracranial pressure
|
|
|
A neonate has been vomiting mucous during the first few hours after birth. Should you be concerned?
|
No; this is due to swallowed materials during delivery will typically spontaneously disappear
|
|
|
A patient presents jaundiced, with dark urine and light colored stools.
|
Hepatitis
|
|
|
A patient presents with a headache, nausea and vomiting, as well as papilledema.
|
Infratentorial tumor
|
|
|
What are the three layers of gastric mucosa?
|
Epithelium; lamina propria; muscularis mucosa
|
|
|
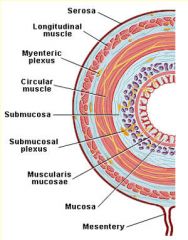
What are the four main layers of the gastrointestinal tract?
|
Mucosa; submucosa; muscularis externa; serosa
|
|
|
In which type of smooth muscle must each cell be activated to contract.
|
Multi-Unit; like skeletal muscle each muscle cell is innervated by a nerve; NO GAP JUNCTIONS; each cell must be activated to contract
|
|
|
In which type of smooth muscle will stimulation of one cell cause the whole layer of muscle to contract?
|
Unitary/Single Unit; muscle layer acts as a syncitium; CONTAINS GAP JUNCTIONS
|
|
|
How would you compare smooth muscle to skeletal muscle?
|
Smooth muscle uses much less energy than skeletal muscle and is also weaker and slower to contract (but can cause sustained contraction, such as a blood vessel, for an extended period of time and hold it without using much energy)
|
|
|
Describe the chemical cascade leading to increased smooth muscle tension.
|
1. Intracellular Ca concentratoins increase mainly from extracellular space but some from SR
2. Calcium binds calmodulin (CaM) 3. Ca-CaM complex activates myosin light chain kinase (MLCK) 4. MLCK phosphorylates light chains in myosin heads and increased myosin ATPase activity 5. Active myosin crossbridges slide along actin and create muscle tension |
|
|
Where is the myenteric plexus located?
|
Between the inner (circular) and outer (longitudinal) layers of smooth muscle in GI tract wall
|
|
|
Where is the submucosal layer and what is its function?
|
Regulates local secretions, blood flow and absorption
Located between mucosa and inner layer of smooth muscle in GI tract wall |
|
|
How is the plasma filtrate that is saliva modified as it is SLOWLY secreted? (plasma at the lowest flow rates?)
|
Na/K pumps remove Na from the filtrate and increase K
Low Na, Cl and HC03 concentrations but highest K concentration It has the lowest osmolarity here |
|
|
How is the plasma filtrate that is saliva modified as flow rate increases? (i.e. person is eating)
|
Ions approach palsma values because less time is available for modification
High sodium, chloride, low potassium |
|
|
Saliva is always HYPOTONIC, but what happens to its osmolarity as its flow rate increases
|
Osmolarity increases (and nearly reaches 300 mOsm/L)
|
|
|
Contraction of what structure in the GI tract would cause shortening of a segment?
|
Longitudinal muscle
|
|
Contraction of what structure in the GI tract would cause a narrowing of the lumen?
|
Circular muscle
|
|
|
What type of cells secrete saliva in the primary secretion stage?
|
Acinus; produces an initial saliva with a composition similar to plasma; is initially isotonic
|
|
|
What happens in the secondary stage of saliva secretion?
|
Saliva is modified in the ducts which reabsorb Na and Cl FROM saliva and secrete K and HC03- INTO saliva
|
|
|
What drug could you give to block parasympathetic induction of salivation?
|
Atropine; anticholinergic drugs inhibit the production of saliva and cause DRY MOUTH
|
|
|
What neurotransmitter does the parasympathetic and sympathetic system use to induce saliva secretion?
|
PS -> Acetylcholine at MAchR
S -> NE at B-R |
|
|
What parasympeathetic cranial nerves control salivation?
|
CN IX and X
|
|
|
The parasympathetic and sympathetic control systems are what kind of neural control for the GI tract?
|
Extrinsic control via the autonomic nervous system
|
|
|
The myenteric (Auerbach) plexus and submucosal (Meissners) plexus are examples of what kind of neural control for the GI tract
|
Intrinsic control via enteric nervous system
|
|
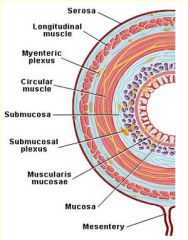
What is the core function and location of the myenteric plexus?
|
GI motility; located between longitudinal and circular smooth muscle layers
|
|
|
What is the core function and location of the submucosal plexus?
|
Local control (secretion, absorption, contraction of muscularis mucosa); located between mucosa and inner layer of smooth muscle in GI tract wall
|
|
|
Barium swallow confirms achalasia with megaesophagus in a patient. The pt asks what can be done to treat this?
|
1. Antispasmodic drugs to inhibit the peristaltic muscles
2. Pneumatic dilator (stiff balloon) to stretch out LES 3. Surgical myotomy to cut out some of the hypertonic muscles to decrease tone/LES pressure |
|
|
Which area of the stomach relaxes to accomodate food?
|
Fundus area (receptive relaxation)
|
|
|
Which area of the stomach mixes food with gastric juices?
|
Body and antrum areas (retropulsion)
|
|
|
Which area of the stomach propels chyme into duodenum?
|
Antrum and pylorus (antral pump)
|
|
|
Which neurotransmitter mediates relaxation of the fundus?
|
VIP
|
|
|
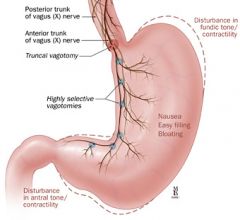
What is the function of the vagal-vagal reflex and why would someone get a vagotomy?
|
VV reflex causes relaxation of the stomach; vagotomy prevents people from eating alot of food since the stomach does not relax
|
|
|
What does an increase in cholecystokinin (CCK) indicate?
|
An increase in fatty acids (fats) and amino acids (protein) in the small intestine decreases the rate of gastric emptying because food is still in the duodenum
|
|
|
What is the function of slow waves?
|
To set the maximum frequency of contractoins for each part of the GI tract (lowest in stomach, highest in duodenum)
Initiated by pacemaker cells which spread the electrical activity (interstitial cells of Cajal, pacemaker cells for GI smooth muscle) |
|
|
Compare the relationship of electrical control activity and contractile force of the cell; (ECA)
ECA + electrical response activity (ERA) + plateau ECA + ERA + spiking |
ECA = no contraction
ECA + ERA (plateau) = weak contraction ECA + ERA + AP spikes on the slow waves = BIG contraction |
|
|
A diabetic patient presents with nausea, vomiting, an early feeling of fullness when eating, weight loss, abdominal bloating and abdominal discomfort. Likely diagnosis?
|
Gastroparesis; high blood glucose from diabetes damages vagus nerve; results in slow emptying/paralysis of the stomach
Goal is to lower blood glucose but you can't fix the vagus nerve |
|
|
A child is born with an absence of parietal cells. What condition will this eventually result in?
|
Pernicious Anemia; decrease in red blood cells due to a lack of B12, which requires intrinsic factor which is produced by parietal cells
|
|
|
A patient presents with a congenital absence of chief cells. Digestion of what will be affected?
|
Proteins via pepsin/pepsinogen
|
|
|
What conditions are required to convert pepsinogen to pepsin?
|
Pepsinogen is secreted by chief cells and activated by HCl (low pH) secreted by parietal Cells
|
|
|
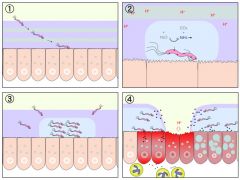
What events control the cephalic phase of digestion?
|
Thinking about food; this goes away after a bit if you don't eat
|
|

What is the major neural control of the cephalic phase of digestion?
|
Vagal innervation; parasympathetics excite peps
|
|
|
What events begin the gastric phase of digestion?
|
It is stimulated by distension of the stomach, presence of food in stomach and decrease in pH; the feedback via entry of food into the stomach intesifies gastric secretions including the release of gastrin and HCl
|
|
|
What events occur during the intestinal phase of digestion?
|
Initiated by the entry of food and acid from the stomach into the duodenum; initiates release of CCK and secretin from the small intestine results in the release of digestive enzymes and bile to digest the ingested meal
|
|
|
Which stage of digestion would be blocked by a vagotomy?
|

Cephalic phase; neural control from brain due to the stimuli of thought, smell, taste, hypoglycemia
|
|
|
What is the function of gastrin?
|
Secrted from the G cells of the antrum in response to a meal; increases H+ secretion via parietal cells; stimulates mucosal growth
|
|
|
How does the combination of Ach Histamine and gastrin effect acid secretion?
|
Massive synergistic effect
|
|
|
Why might you prescribe a patient cimetidine?
|
Blocks the release of histamine (H2R antagonist) to decrease stomach acid; this drug came out when there were no proton pump inhibitors
|
|
|
Which gastric phase accounts for the largest acid response to a meal?
|
Gastric phase; 60%
|
|
|
An acidification of the antrum will block which digestive phase?
|
Gastric phase
|
|
|
What five things do gastric (oxyntic) glands secrete?
|
HCl
Pepsinogen Intrinisic factor Mucus Rennin (chymosin) |
|
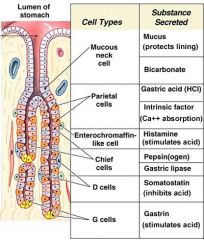
What two main things so pyloric glands secrete?
|
Gastrin
Mucus |
|
|
What are the three major functions of gastric acid?
|
Bacteriostatic
Convert pepsinogen to pepsin Begin protein digestion (via pepsin) |
|
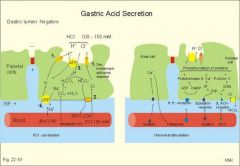
Where do parietal cells get HCl from?
|
Carbon dioxidie pulled out of blood
C02 + H20 -> H2C03 -> H + HC03- |
|
What is the alkalyn tide?
|
Bicarb is dumped out into the blood after a meal
Bicarbonate in the lumen is exchanged for chloride within the parietal cells (so HCl can form), parietal cells dump bicarb into blood = alkalyn tide |
|
What is the etiology of stomach ulcers?
|
A decreased mucous layer or something (h. pylori) cause a break in the underlying epithelial cells which prevents them from carrying out their normal buffering action of H+; the H+ gets underneath the cells and an ulcer happens
Tx w/ proton pump inhibitors |
|
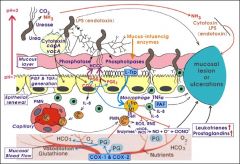
What kind of things weaken the integrity of the mucosal barrier, potentially causing ulcers?
|
H. pylori, NSAIDs, ethanol, bile salts
|
|
|
In which type of learning does repeated stimulation decrease a response
|
Habituation; learning to ignore irrelevent stimuli like behavioral science class
|
|
|
In which type of learning is there a progressive amplification of a response following repeated administration of a stimulus.
|
Sensitization
|
|
|
In which type of learning is there an association between a stimulus that evokes a physiologic reflex and a new stimulus
|
Classical conditioning; pavlov
|
|
|
After repeated trips to the hospital for chemotherapy, the side effects of which include nausea, a patient may begin to experience nausea. The pt experiences nausea as soon as they see the hospital. What type of learning is this?
|
Classical conditioning distinct from operant conditioning because it deals with involuntary reflex behaviors; CC is not maintained by consequences
|
|
|
In which type of learning is a behavior strengthened if followed by a reinforcer or diminished if followed by a punishment?
|
Operant Conditioning; disctinct from classical because it deals with voluntary behaviors
|
|
|
In pavlov's dog how would you cause extinction of the classically conditioned response?
|
Don't give food with the bell and eventually the dog will stop salivating to the bell
|
|
|
What type of stimulus is that which naturally/automatically triggers a response?
|
Unconditioned stimulus
|
|
|
In the Pavlov's dog, which component was the conditioned stimulus?
|
The bell; it was originally neutral but became able to illict a response following learning of an association
|
|
|
In Pavlov's dog, which component was the conditioned response?
|
Salivation in response to the bell; it was a learned response to a previously neutral stimulus derived from an association between an unconditioned stimulus and a conditioned stimulus
|
|
|
In Pavlov's dog, if the dog suddenly started salivating in response to the bell many years later what is this an example of?
|
Spontaneous recover; sudden reappearance of a previously extinguished conditioned response
|
|
|
Why might you administer a continuous reinforcement schedule vs intermittent reinforcement schedule?
|
Intermittent reinforcement results in slower acquisition but a much greater resistance to extinction than a continous reinforcement schedule
|
|
|
Which family of bacteria are gram negative rods, found in a wide variety of environments, motile and facultative anaerobes with LPS as the major cell wall antigen. Some are opportunistic pathogens; others are always human pathogens; some are normal flora that can become pathogenic after acquiring virulence genes from other sources
|
enterobacteriaceae
|
|

A patient presents with fever, abdominal pain, transient diarrhea and a salmon coloured maculopapular rash on the trunk. Labs reveal motile, gram negative rods INTRACELLULARLY. What type of Salmonella is this?
|
Typhoid (Typi Paratyphi) ; its host specificity is human restricted
|
|
|
A patient presents with sym,ptoms of gastroenteritis including abdominal pain, vomiting and inflammatory diarrhea after eating poorly cooked eggs. Labs reveal motile, gram negative rods. You suspect which type of salmonella?
|
Non-typhoid (Salmonella typhimurium enteriditis)
|
|

Which organism notoriously causes gastroenteritis via infection of the gall bladder?
|
Salmonella Typhi
|
|

A patient presents with a macupapular rash, called rose spots. What organism do you suspect?
|
Salmomella
|
|
|
What treatment is reccomended by typhoid by not non-typhoid salmonella?
|
Antibiotics; dianogis is based on the isolation of the microorganism from stool speciments
|
|
|
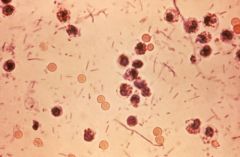
A patient presents with gastroenteritis. What would you expect to see on Eosine Methylene Blue (EMB) and MacConkey Media to suspect a salmonella suspicion.
|
Since salmonella is a non-lactose fermenter there will be no change in either media.
MCM and EMB selects for gram negative organisms which are lactose fermenters. |
|
|
How does shigella dysenteriae cause diarrhea?
|
AB toxin (A for action, B for bindig) binds to microvillus membrane in colon; A unit is released and destroys 28S ribosome; this causes cellular damage to the intestinal epithelium, which now can't absorb water and thus, diarrhea!
|
|
|
Through which colon cells do shieglla andsalmonella invade?
|
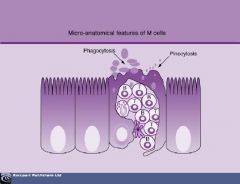
M cells
|
|
Which enteric organisms are gram negative rods which are NON motile, slow lactose fermenters (scored negative)
|
Shigella
|
|
|
Which properties of shiegella differentiate it from salmonella or e. coli?
|
Shigella has no flagella, does not ferment lactose OR produce H2S
Differentiates it from e. coli (lactose fermenter) and salmonella (non lactose fermenter, produces H2S) |
|
|
Which form of shiegalla is more severe?
|
s. dysenteriae is more severe than s. sonnei (85% of shiegellosis cases in US, mostly children and male homosexuals)
|
|

Between E. coli, salmonella, and shigalla, which would you expect to be part of the normal flora?
|
E. coli; but can also be opportunistic
You don't see salmonella or shigalla in normal flora |
|
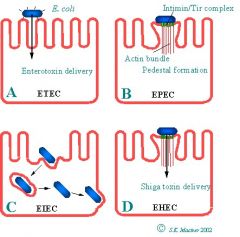
A patient presents with abdominal cramps, bloody diarrhea, thrombycotyopenia
(decrease in platelets), and renal failure (uremia) . The history is notable for consuming suspect hamburger meat from Jack in the Box. What is the likely organism? |
Enterohemorrhagic Escherichia coli (EHEC); uses shiga like toxin causing intestinal epithelial cell death
|
|
|
A patient presents with rice water diarrhea. History is notable for recent travel to Mexico. What is the likely organism?
|
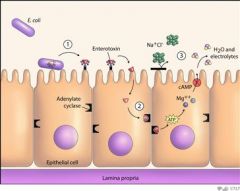
Enterotoxigenic Escherichia Coli (ETEC) = Travelers Diarrhea = Montezuma's Revenge
Heat stable/labile toxins which promote hypersecretion of electrolytes; water folows via osmotic pull resulting in water and electrolyte loss. |
|
|
A patient presents with fever and bloody stool with white blood cells. Labs reveal a lactose fermenter. History is notable for eating suspect cheese and gucamole.
|
Enteroinvasive Escherichia Coli (EIEC); presents just like Shigella and is diagnosed with a DNA probe kit
|
|

How is Enterohemorrhagic Escherichia Coli (EMEC) diagnosed?
|
Isolation of sorbitol nonfermenting colonies on SMAC + serotying and/or presence of shiga toxin in the stool
|
|
|
A patient from Alaska presents with abdominal pain, fever, and diarrhea. You intially suspect appendicitis, but labs return a lactose negative, urease positive organism with motility ONLY at temperatures below 30 C. History is notable for drinking suspect milk.
|
Yersinia enterocolitica; since it's cold tolerant it can survive refrigeration which becomes a problem with stored blood and blood transfusion related bacteremia
|
|
|
Between ETEC, EHEC, and EIEC, which two cause bloody diarrhea?
|
EHEC and EIEC
|
|
What is the only nonmotile enteric orgainsm?
|
Shigella
|
|
|
What is the most common viral cause of endemic severe diarrheal illness in infants and young children?
|
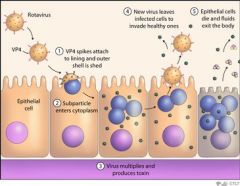
Rotavirus Group A
member of the family reovirus (respiratory enteric orphan) |
|
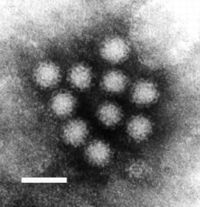
What is the most common cause of viral gastroenteritis in adults?
|
Norwalk virus
|
|
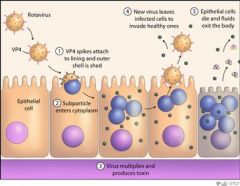
What viral protein does rotavirus use to infect cells?
|
NSP4; for budding, intracellular Ca release = diarrhea, disrupts tight junctions = diarrhea
|
|
|
How do Adenovirus's VA-RNA's interfere with host defense?
|
Block interferon anti-viral response
|
|
|
How does Adenovirus's E1A, E1B, E3 interfere with host defense?
|
Promote cell proliferation and block apoptosis by binding Rb and p53
|
|

A preschooler presents with gastroenteritis. Under the microscope you note a virus with cup shaped indentations
|
Calciviridae
|
|
|
An adult presents with viral gastroenteritis. History is notable for eating steamed oysters. How does the suspect virus react against ABO blood group patients vs A or AB?
|
Preferentially binds the carbohydrates of ABO blood group antigens in the mucosal cell surfaces of the gut
|
|
A patient presents with viral gastroenteritis. Labs reveal an organism with star morphology.
|
Astrovirus
|
|
|
A patient presents with a SUDDEN onset of gastroenteritis with fever followed 5 days later by jaundice, dark urine, pale stool and itch. Patient is notable for eating shell fish 20 days prior.
|
Hepatitis A
Diagnosis made by anti-HAV IgM detection by ELISA |
|
|
A patient presents with diarrhea. Labs show a lactose negative orgainsm with flagellar motility.
|
Salmonella
|
|
|
A patient presents with bloody diarrhea. Labs show a lactose negative orgainsm which produces Shiga toxin.
|
Shigella
|
|
|
A patient presents with bloody diarrhea and signs of hemolytic uremic syndrome. Labs show a a shiga like toxin.
|
EHEC
Enterohemorrhagic E. coli |
|
|
A young child presents with bloody diarrhea. She is in day care and the symptoms may possibly be appendicitis but you're not sure yet. If not appendicitis, what is it?
|
Yersinia enterocolitica
|
|
|
A patient presents with watery diarrhea. Labs reveal ST and LT toxins.
|
Traveler's diarrhea; ETEC
entertoxigenic E. coli |

