![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
A patient complains of difficulty initiating swallowing. What kind of dysphagia is this?
|
Oropharyngeal
|
|
|
A patient complains of solid food sticking in his throat. What kind of dysphagia is this?
|
Esophageal mechanical
|
|
|
A patient complains of liquids 'sticking' in his throat. What kind of dysphagia is this?
|
Esophageal motility
|
|
|
A patient complains of solid foods sticking in his throat that occurs intermittently. Diagnosis?
|
Esophageal spasm
|
|
|
A patient complains of solid foods sticking in his throat that has been getting progressively worse. Differential?
|
Scleroderma, achalasia, diabetes
|
|
|
A patient presents with dysphagia to solids and occasionally liquids. There is occasional regurgitation which usually occurs shortly after a meal or while in the recumbent position. This patient also reports a history of chest pain following a meal. Diagnosis?
|
Achalasia
|
|
|
A patient presents with dysphagia to solids and occasionally liquids. There is occasional regurgitation which usually occurs shortly after a meal or while in the recumbent position. This patient also reports a history of chest pain following a meal. Barium esophagram reveals poor emptying of the barium from the esophagus which is dilated. You note a characteristic 'bird's beak' narrowing of the distal esophagus due to a non relaxing LES. What disease is this indicative of?
|
Achalasia
|
|
|
A patient presents with incomplete LES relaxation, increased LES tone, and aperistalsis of the esophagus. Diagnosis?
|
Achalasia; results from a loss of distal esophageal inhibitory neurons (idiopathic)
|
|
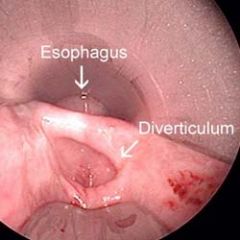
Using barium swallow you notice an outpouching directly above the upper esophageal sphincter. Diagnosis?
|
Zenker diverticulum
can accumulate significant amounts of good, producing a mass and symptoms that include regurgitation |
|
An anemic patient presents with pain and dysphagia when her food hasn't been completely chewed. Barium swallow is notable for thin membranes of normal esophageal tissue consisting of mucosa or submucosa that protrudes out in the upper portion of the esophagus. Diagnosis?
|
Esophageal web; can be congenital or acquired (anemia)
|
|
|
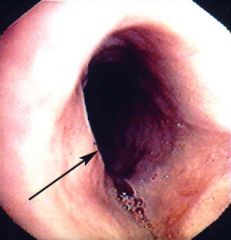
After barium swallow you note that the patient has marked narrowing of the distal esophagus. A biopsy reveals mucosa, submucosa and hypertrophic muscularis propria in rings.
|

Schatzki's Ring
|
|
|
A patient eating steak presents with acute dysphagia and drooling. This patient is notable for a history of schatzki's rings.
|
food bolus impaction; may require endoscopy to push the obstructing food into the stomach or remove it from the esophagus
|
|

A child presents with intermittent dysphagia. You note in the history they have many allergies.
|
Eosinophilic Esophagitis; allergic inflammatory condition of the esophagus; can tx with steroids; the esophagus is fragile so there is a greater risk of perfornation
Diagnosis is made with biopsy; normal esophageal tissue does not have any eosinophil |
|
|
A patient presents with dysphagia, heartburn and the occasional regurgitation of sour tasting fluid. The history is notable for alcoholism.
|
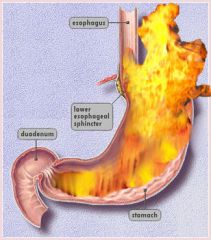
Gastroesophageal Reflux Disease (GERD)
Alcohol decreases lower esophageal reflux tone |
|
|
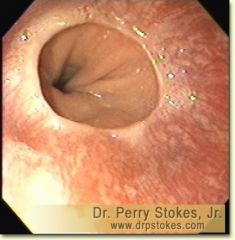
A patient presents complaining of dysphagia and heartburn. Endoscopy reveals several patches of red, velvety mucoa extending upward from the gastroesophageal junction. A biopsy shows intestinal metaplasia within the esophageal squamous mucosa.
|
Barrett Esophagus; due to chronic GERD; increases risk of esophageal adenocarcinoma
Management = frequent endoscopy and biopsy of the affected squamous mucosa to detect for dysplasia |
|
|
A patient presents with pain upon swallowing, progressive weight loss, chest pain and vomiting. The history is notable for a 30 year history of smoking and alcoholism.
|
Barrett's Associated Adenocarcinoma or Squamous Cell Carcinoma
|
|
|
A patient presents with dysphagia upon ingestion of solid foods only.
|
Esophageal mechanical dysphagia
|
|
|
A patient presents with dysphagia upon ingestion of both solids and liquids.
|
Esophageal motor (neural) dysphagia
|
|
|
What is the most common cause of fungal esophagitis?
|
Candidiasis
Mucormycosis and aspergillosis may also occur |
|
|
A patient presents with dysphagia. History is notable for a history of connective tissue disease.
|
Scleroderma
|
|
|
A patient presents with a sense of solids and liquids sticking in the esophagus. You cannot detect any evidence of reflux or histopathology based esophageal motility disorder.
|
Functional dysphagia
May tx with antidepressants |
|
|
A young man presents with solid dysphagia. What should you be on the lookout for?
|
Eosinophilic Esophagitis
|
|
|
What kind of dysphagia would you not use esophageal function testing (manometry)?
|
Obstructive dysphagia
|
|
|
If you knocked out cholinergic neurons in the myenteric plexus what disease would manifest?
|
Achalasia; the LES is inhibited by the myenteric plexus using vasoactive intestinal polypeptide (VIP) and nitric oxide (NO) neurotransmitters; knocking out the MP would result in increased tone
|
|
|
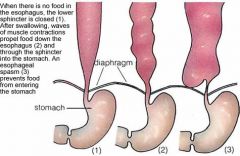
What action stimulates the cholinergic neurons in the myenetric plexus to inhibit the lower esophageal sphincter?
|
Deglutition (swallowing)
|
|
|
Barium swallow reveals a mid esophageal diverticulum. What is the likely etiology?
|
It is the only true diverticulum of the esophagus (contains all the layers of the esophageal wall)
It's a traction diverticulum due to pulling of the esophageal wall by inflammatory or fibrotic tissue |
|

What might cause an epiphrenic diverticulum (located near the diaphragm/right above the LES)?
|
Achalasia or another motility disorder
|
|
|
What kind of diverticulum is Zenker's?
|
False diverticulum; a herniation of just the MUCOSA and SUBMUCOSA through the muscular wall
|
|

A patient presents with hypertrophy and fibrosis of muscle, coupled with incomplete relaxation, which causes a defect in the posterior cervical esophagus.
|
Cricopharyngeal bar; the CP muscle constitutes the superior esophageal sphincter;
|
|
Hypertrophied smooth muscle above the squamo-columnar junction is called what
|
Esophageal A Ring (differs from Schatzki rings in that its muscular, not mucosa or submucosa)
|
|
|
A bulemic patient presents with dysphagic. Barium swallow reveals narrowing of the esophagus.
|
Caustic esophageal stricture; damage to esophageal tissue caused scar formation, which tightens the tissue/pulls traction causing difficulty upon swallowing
|
|
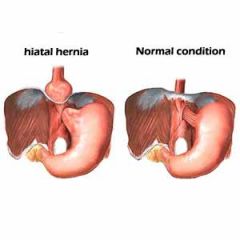
A patient presents with abdominal pain and LES incompetence.
|
Hiatal hernia; separation of the diaphragmatic cura and protrusion of the stomach into the thorax through the resulting gap
|
|
|
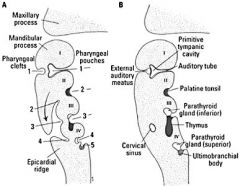
Which arch and nerve is this describing:
Mesoderm: Muscles of mastication, mylohyoid, anterior belly of digastric, tensor veli palatini, tensor tympani Neural crest: Maxilla, mandible,incus, malleus, zygomatic bone, squamous temporal bone, palatine bone, vomer, sphenomandibular ligament |
Arch 1: CN V
|
|
|
Which arch and nerve is this describing?
Mesoderm: Muscles of facial expression, posterior belly of digastric, stylohyoid, stapedius Neural Crest: Stapes, styloid process, stylohyoid ligament, lesser horn and upper body of hyoid bone |
Arch 2: CN VII
|
|
|
Which arch and nerve is this describing?
Mesoderm: Stylopharyngeus, common carotid arteries, internal carotid arteries Neural Crest: Greater horn and lower body of hyoid bone |
Arch 3: CN IX
|
|
|
Which arch and nerve is this describing?
Mesoderm: Muscles of soft palate (except tensor veli palatini), muscles of the pharynx (except stylopharyngeus) cricothyroid, cricopharyngeus, laryngeal cartilages, right subclavian artery, arch of aorta Neural Crest: None |
Arch 4: CN X (superior laryngeal nerve)
|
|
|
Which arch and nerve is this describing?
Mesoderm: Intrinisic muscles of the larynx (except cricothyroid), upper muscles of the esophagus, laryngeal cartilages, pulmonary arteries, ductus arteriosus Neural Crest: None |
Arch 6: CN X (recurrent laryngeal nerve)
|
|
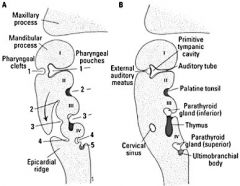
Which pouch gives rise to the epithelial lining of auditory tube and middle ear cavity?
|
Pouch 1
|
|
|
Which pouch gives rise to epithelial lining of palatine tonsil crypts?
|
Pouch 2
|
|
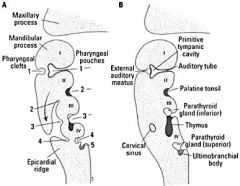
Which pouch gives rise to the inferior parathyroid gland and the thymus?
|
Pouch 3
|
|
|
Which pouch gives rise to the superior parathyroid gland and the ultimobranchial body?
|
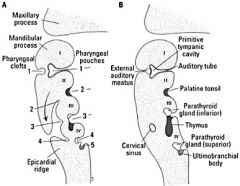
Pouch 4
|
|
|
What are the three primordia swellings of the face?
|
Frontonasal prominence, maxillary prominence (pharyngeal arch 1), mandibular prominence (pharyngeal arch 1)
|
|
|
How are the nasal cavities and sinuses formed?
|
Invaginations of ectoderm at the nasal pits
|
|

A patient presents with an abnormally small jaw. You suspect this disease is characterized by a lack of migration of neural crest cells into pharyngeal arch 1 during development. Diagnosis?
|
Treacher Collins Syndrome (mandibulofacial dysotosis)
|
|
|
What happens when pharyngeal pouch 2 and pharyngeal groove 2 persist?
|
Tracheoesophageal Fistula
|
|
An abnormal migration of pouch's 3 or 4 would lead to what?
|
Ectopic thymus, parathyroid, or thyroid tissue
Glandular tissue may be found anywhere along their migratory path |
|
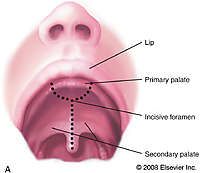
Which anatomical landmark separates anterior from posterior cleft palate defects?
|
Incisive foramen
|
|
|
which type of cleft palate occurs when the palatine shelves fail to fuse with each other and with the nasal septum?
|
Posterior Cleft Palate
|
|
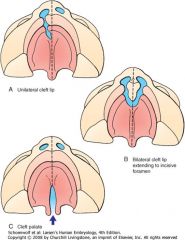
Which type of cleft palate occurs when the palantine shelves fail to fuse with the primary palate?
|
Anterior cleft palate
|
|
|
Which type of cleft palate occurs when there is a combination of both anterior and posterior defects?
|
Anteroposterior cleft palate
|
|

A patient presents with a small jaw, low set ears, wide spaced eyes and a cleft palate. Diagnosis?
|
DiGeorge's Syndrome; occurs when pharyngeal pouches 3 and 4 fail to differentiate into the thymus and parathyroid glands
|
|
|
Which two arches do the bulk of the tongue come from?
|
1 (anterior 2/3) and 3 (posterior 1/3)
4 forms the very back of the tongue |
|
|
What is the nervous innervation of the general sensory of the tongue?
|
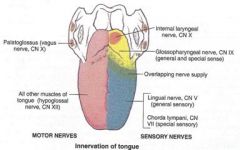
V3 (anterior 2/3), IX (posterior 1/3), X (very back)
|
|
|
What is the nervous innervation of the special sense of the tongue?
|
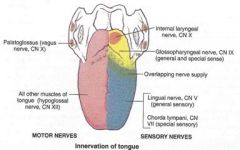
VII (taste anterior 2/3 of tongue, does NOT precisely follow sulcus terminalis boundry), valate papallae which is just anterior to the sulcus terminalis is thus innervates by IX, and X still innervates very back
|
|
|
Where do abnormal cysts generally occur?
|
Anterior border of the sternocleidomastoid m.
|

