![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
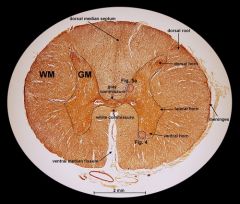
label transverse section of spinal cord
|
|
|
|
Describe the structure of a neurone and a nerve cell body
|
Neurone consists of:
Cell body (perikaryon)- contains nucleus, cytoplasm, nissl bodies (aggregations of RER, basophilic due to lots of r.RNA, protein synthesis) Function: maintains the cell, generates nerve impulses. Axon hillock – region at end of cell body. Controls firing of the neuron- action potential generated by axon hillock if signal is greater the threshold level in axon hillock action potential is fired down the axon. Axon- outgoing single process, function is to conduct nerve impulses away from cell body to other cells (muscle, glands, nerve). Terminal arborisation may occur where axon divides into 2 branches at the terminal, which have small swellings at end called boutons terminaux which are in close contact with another nerve cell or effector cell – synapse ( synaptic vesicles release neurotransmittier substances into synaptic cleft) Dendrites – incoming multiple processes, specialised to receive stimuli from sensory organs or other neurones and conduct them towards cell body, increase surface area. Proximal dendrite – nearest to cell body, thickest Distal dendrite – further away from cell body, thin The thicker the process, the faster the conduction. 2+ dendrites, 1 axon = multipolar neurone,(mostly CNS) 1 dendrite, 1 axon = bipolar neurone, fusion of dendrite and axon forming a single stem from cell body = pseudounipolar. |
|
|
How can the nervous system be classified anatomically and functionally ?
|
ANATOMICALLY:
CNS: consists of the brain and spinal cord which are composed of neurones and supporting neuroglial cells ( prevent polarisation of nerves) Grey matter – cell bodies and their associated fibres – collections = nucleus White matter – nerve fibres - myelinated axons – collections = tract PNS: consist of the cranial, spinal and autonomic nerves and their associated ganglia. FUNTIONALLY: Autonomic nervous system: effector organs are visceral organs, smooth muscle, cardiac muscle, secretory glands. Constant action – establishes and maintains homeostasis. Intermittent action- promotes excretory mechanism when necessary and appropriate. ANS division – sympathetic and parasympathetic NS (non-voluntary) Somatic nervous system: 1 effector neurone from spinal cranial locations terminates directly on effector organ – skeletal muscle. Voluntary control. |
|
|
Compare collections of nerve fibres in CNS & PNS.
|
CNS: collections of nerve fibres form tracts which form functional groupings. They are found in white matter – myelin gives white appearance.
PNS: collections of nerve fibres form peripheral nerves which are sensory or motor neurones and are surrounded by connective tissue. Non-myelinated or myelinated according to arrangement of Schwann cells along axon. |
|
|
Compare neuroglial cells in CNS and PNS.
|
Non neural cells found in-between neurones and provide structural and mechanical support for them.
In the CNS: Astrocytes: support epithelial cells of the blood brain barrier, repair and scarring of brain and spinal cord following trauma, provision of nutrients to neurone Oligodentrocytes: support and maintenance, form myelin sheath ( up to 250 axons, 1 schwann cell-1axon) Microglia: macrophages derived from monocytes – inflammation and immunity Ependymal cells: line central cavities of brain and spinal cord where they supply a permeable barrier between the cerebrospinal fluid which fills the cavities and the tissue fluid which bathes the CNS cells. In the PNS: Satellite cells( Capsule) – surround cell bodies in ganglia to support them, allow functions to occur. Schwaan cells – myelination of cell – support and maintenance Microglia : macrophages derived from monocytes – inflammation and immunity |
|
|
What are the meninges?
|
The meninges is a 3 layer connective tissue sheath which covers the CNS (white and grey matter) in the brain and spinal cord and forms the protective bony housing along with skull and vertebral column.
- the dura mater – Outer most layer is thick, fibrous - arachnoid – deep to the dura, non-vascular connective tissue membrane - the pia mater - The inner layer is vascular tissue cerebrospinal fluid is located between the arachnoid and pia mater |
|
|
Compare collectiong of cell bodies in CNS & PNS.
|
CNS: a collection of cell bodies inside the CNS is called a nucleus and found in grey matter. In spinal cord grey matter is centrally positioned, surrounded by white matter. In cerebrum or cerebellum, white matter is centrally positioned, surrounded by grey matter- cortex. Nuclei may lie deeply placed in the brain
PNS: a collection of cell bodies outside the CNS is called a ganglion and are surrounded by connective tissue capsules Cerebrospinal ganglia – comprise of cell bodies of all afferent/sensory neurones. Ganglia is found in dorsal root of spinal nerves. The ganglion cells are round with large ovoid nuclei and conspicuous nucleoli. Pseudoplar ( dendrite from PNS, axon to CNS), axons are mostly myelinated. The cell bodies are grouped together at periphery and the myelinated fibres are central. A Single layer of satellite cells surround each cell for support. Autonomic ganglia – a collection of cell bodies found in the sympathetic system as 2 parallel chain along the anterior surface of the vertebrae or in the parasympathetic system as poorly encapsulated structures near or within various organs Unlike cerospinal ganglia, they don’t show peripheral arrangement of cell bodies. Autonomic ganglion cells are small, multipolar, axons are generally unmyelinated. Ill-defined layer of satellite cells around cell bodies, |
|
|
Describe the structure of the peripheral nerve.
|
The peripheral nerves are found outside the CNS and comprise of bundles of nerve fibres, held together by connective tissue. Axons and dendrites form bundles called fascicules which are surrounded by dense connective tissue (perineurium). Inside each fascicle the individual nerve fibres are supported by loose connective tissue (areolar)- endoneurium. Bundles of fascicles are surrounded by a loose connective tissue called the epineurium which houses blood vessels, lymphatics, fat cells and sometimes nerve cells.
Peripheral nerves that carry impulses to CNS – sensory/afferent/. Those that carry impulses from CNS – motor/efferent. |
|
|
Describe how nerve fibres can by myelinated or non myelinated in PNS.
|
Each nerve fibre in a peripheral nerve consists of an axon surrounded by a sheath of Schwann cells (neurolemma) which support and maintain the nerve. Non-myelinated – nerve fibres invaginated into the cytoplasm of the Schwann cells. Myelinated – Schwann cell has formed several concentric layers of its own plama membrane ( myelin). Nodes of ranvier- gaps in sheath- interval between the contributions made to the sheath, by consecutive Schwann cells. Myelinated nerves are difficult to recognise unless treated with special fixatives and stains eg osmium tetroxide to retain and stain lipids (usually dissolve).
myelinated increases conduction speed of impulse along axon - saltatory conduction, action potential jumps from node of ranvier to the next node. myelination insulates internodal regions by increasing resistance ( ability to resist charge - closed channels) and lowering capacitance ( ability to store charge). the ion channels are concentrated in the nodes of ranvier |
|
|
Give an outline of the anatomy of the autonomic nervous system and its division into the sympathetic and parasympathetic parts.
|
General layout of ANS: 2 neurones arranged in series, preganglionic neurone has cell body in CNS, preganglionic neurone has myelinated axon (white rami communicante), postganglionic neurone has cell body and axon in PNS and terminates directly on effector organ eg visceral organs, smooth muscle, secretory glands. Postganglionic neurone has un-myelinated axon ( grey rami communicante).
SNS – preganglionic neurone has cell bodies in thoraco-lumbar cord (cell bodies in all 12 thoracic segments of spinal cord and the first 2 lumbar segments), relatively short preganglionic neurone which secretes acetylcholine (cholinergic- SAME IN PNS). Post ganglionic neurones have nicotinic receptors (same in PNS), secrete noradrenalin or adrenalin (noradrenergic or adrenergic) and are relatively long. Post ganglionic neurones for Sweat glands and ejaculation mechanisms are cholinergic. Effector organs express a variety of adrenoreceptors – alpha and beta. PNS – cell bodies in brain and spinal cord (s2,s3,s4)– cranio sacral. Preganglionic neurones are relatively long and cholinergic. Post ganglionic neurones are short and within the walls of effector organs. They express nicotinic receptors and are cholinergic. Effector organs express muscarinic receptors which are blocked by atropine. |
|
|
Describe the different pathways via which these 2 division distribute their fibres to and from target organs.
|
Target organs = visceral organs, smooth muscle, secretory glands
Sympathetic pathway - flows out of thoraco lumbar cord only ( 12 thoracic segments and 1st 2 lumbar segments of spinal cord) - preganglionic neurone (short) – cholinergic ( acetylcholine) - postganglionic neurone(long) – noradrenalin/adrenalin ( adrenal medulla) – cholinergic in sweat gland and ejaculation mechanisms - preganglionic neurone (short) synapses in paravertebral chain. - Synapse in 3 ways: synapse in paravertebral chain at same level as origin, synapse at different level to origin (up or down), doesn’t synapse in paravertebral chain (splanchnic nerve) - Effector organ – 2 types of adrenoreceptors – alpha or beta Parasympathetic pathway - Flows out of cranio sacral – brainstem and spinal cord - Preganglionic (long) and postganglionic (short) are cholinergic - Postganglionic neurone within wall of effector - Effector organ express muscarinic receptors ( inhibited by atropine) |
|
|
Deffentiate between the ganglion in sympathetic nervous system and parasympathetic nervous system.
|
ANS ganglia: cells are small, multipolar, unmyelinated, no peripheral arrangement of cell bodies. connective tissue capsule, ill-defined layer of satelite cells.
SNS: synapses in paravertebral chain. cell bodies in parallel chains along the vertebrae. PNS: poorly encapsulated ganglia near or within effector muscle. |
|
|
Describe the difference in the overall functional roles of the 2 ANS divisions
|
SNS: fight or flight, expenditure of energy, diversion of blood to muscles and heart, increase in blood preasure and heart rate, reduced blood flow to GI tract and skin, increases glucagon, increased lipolysis & glycogenolysis & gluconeogenesis.
PNS: rest or digest, reduces heart rate and force of heart contraction, promotes digestion, promotes bodily functions such as bladder emptying, promotes sleep, increases insulin, increased glycogenesis, lipogenesis, increased uptake of glucose by cells, increased protein synthesis, growth and repair. Most organs are innervated by ANS, usually in duality with both sympathetic and parasympathetic NS. However sweat gland receives only sympathetic. Most effects of SNS and PNS are reciprocal. ANS constant control – homeostasis, intermittent control – excretory mechanisms when necessary and appropriate |
|
|
Describe the clinical consequences of overactive ANS
|
Overactive PNS – dilated blood vessels over time can result in shortage of glucose to CNS
Overactive ANS – constriction of blood vessels over time can result in shortage of substrates to tissues. |
|
|
Explain the flexibility in ANS
|
PNS and SNS share the same anatomical layout but differ slightly in detail. They both have the same number of synapses however they use different neurotransmitters and have different receptors. Transmitters and receptors of ANS are the essence of therapeutics and their side effects. Cardiac ones are especially important as well as the exceptions (sweat glands and ejaculation mechanisms have cholinergic postganglionic neurones in SNS instead of noradrenergic or adrenergic.)
Postganglionic neurone in SNS releases noradrenalin or adrenalin whereas in PNS acetylcholine is released. Therefore there are different receptors on the effector organs. In the sympathetic pathway the effector organs have either alpha or beta adrenoreceptors. In the parasympathetic pathway the effector organs have muscarinic receptors which are blocked by atroprine. |
|
|
Describe the transmitters involved at the synapses and end organs of both SNS and PNS.
|
Sympathetic nervous system: postganglionic neurone nicotinic receptors, effector organs have alpha and beta adrenoreceptors
Parasympathetic nervous system: postganglionic neurone nicotinic receptors, effector organs have muscarinic receptors which are blocked by atropine |
|
|
Explain the affect of the loss of myelin sheath in a nerve fibre
|
Saltatory conduction is lost and channels spread out from node of ranvier along axon to allow local spread to occur - increasing capacitance and decreasing resistance. In the PNS schwann cells can sometimes remyelinate cells. In the PNS oligodendrocytes cannot.
This is a defect seen in certain disorders of the CNS such as multiple sclerosis. The loss of myelin is selective and patchy along the axon. In addition to demyelination, there is axonal destruction as well as overgrowth of glial tissue. The most frequent symptom is spastic paralysis of both legs. |
|
|
Describe the affect of degeneration in peripheral nerves
|
Noninflammatory disease of peripheral nerves ( peripheral neuropathy – diabetes) and inflammatory disorder (neuritis) are common degenerative changes in peripheral nerves causing sensory loss, motor weakness or both.
Walerian degeneration of axon, regeneration of proximal axon can occur in PNS. If a myelinated axon then channels will redistribute along axon and change from saltatory conduction to local spread. Remyelination by schwann cells can occur but oligodenodrocytes cannot in the CNS. |
|
|
Describe nerve degeneration and regeneration.
|
Mature nerve cells do not undergo mitosis and so can’t be replaced. Regeneration of damaged peripheral nerves may happen if their axons are still attached to the cell bodies- the proximal segment of the axon attached to the cell body has the potential to regenerate. The distal segment undergoes complete disintegration (wallerian degeneration). The neurolemmal sheaths ( Schwann cells) of these degenerating axons, however, remain intact and play an important role in regeneration, This is called axontemesis which is worse than neuropraxia where there is compression causing blockage of impuleses but better than neuotemesis where the neurolemma is damaged as well as axon and myelin sheath and full recovery is unlikely.
Parkinsons disease, carpal tunnel syndrome – entrapment of nerves |
|
|
Outline the process of haemopoiesis, explaining how the cellular components of the blood are derived from stem cells.
|
In the foetus blood is initially made by mesoderm of the yolk sac, then the liver, then the spleen and finally the bone marrow ( when all hyaline cartilage is bone)
All cellular components derive from stem cells. There are 2 distinct lines which come from stem cells, myeloid blasts and lymphoblasts. Myeloid blasts are precursors for RBCS ( reticulocyte-immature > erythrocyte – mature), platelets (from megakaryocyte), macrophages ( from monocytes), granulocytes ( white cells with granules -mast cells, neutrophils, eosophils, basophils). Lymphoblasts are precursors of lymphocytes . Lymphocytes leave the bone marrow and some pass through the thymus, transforming to t lymphocytes( killer or memory). Others are beta lymphocytes ( which produce plasma cells ). Immature blood cells are held in the bone marrow by adhesion molecules (collagen and fibronectin). As blood cells mature, the adhesion molecule receptors on their surface decrease and so they are released into the circulation. The rate of division and differentiation of blood cells is regulated by growth factors –cytokines. |
|
|
Describe the structure and function of erythrocytes and reticulocytes
|
Structure: no nucleus, 7.2micrometes in diameter, bioconcave shape – increased surface area to volume ratio, can squeeze through capillaries. Contains haemoglobin – 4 subunits (tetramer), 2 alpha, 2 beta, each with haem that binds 2 oxygen atoms.
Function: transport oxygen from the lungs to the tissues of the body and to transport co2 back to the lungs. Regulation: in low oxygen levels (hypoxia) feedback mechanism stimulates increased erythropoietin production from peritubular endothelial cells in the kidney, which increase the rate of red cell production and release from bone marrow, increasing oxygen carrying capacity of blood. The average RBC survives 120 days and is broken down in liver and spleen: iron is recycled, protoporphyrin ring of haem forms bilirubin. |
|
|
Describe the structure and function of neutrophils
|
Neutrophils are most numerous granulocytes – multi-lobed nucles and small granules in cytoplasm(lysosomes with enzymes).
Function: migrate out of circulation to site of infection (chemotaxis- movement of a cell in response to chemical stimulus) and destroy foreign material by phagocytosis. Regulation: activated by Cytokines such as GCSF- granulocyte colony stimulating factor, released from damaged cells, increases neutrophil production and chemotaxis and phagocytosis. The average neutrophil survives 10 hrs. |
|
|
Describe the structure and function of eosinphils
|
Structure: bilobed nucleus , orange (stain) large granules
Function: highly mobile, weakly phagocytosis, release cytotoxic enzymes to damage large particles, ingest antigen-antibody complexes. Regulation: numbers increased in association with allergic reactions eg asthma and hay fever |
|
|
Describe the structure and function of basophils:
|
Least common cells of the blood
Structure: many large dark purple/blue granules Function: mediate acute inflammatory reactions, heparin and histamine. At local tissue damage basophils are released into tissue. Histamine causes dilation of blood vessels – leaky vessels- oedema, heparin prevents clotting of the blood |
|
|
Describe the structure and function of monocytes
|
Structure: largest cells in peripheral blood , folded kidney shaped nucleus, lysosomes, grey/blue cytoplasm, occasional vacuoles
Function: migrate out of circulation to tissues after 20-40 hrs to become macrophages ( kupffer cells in liver, microglia in CNS). Chemotaxis – movement towards areas of infection, inflammation and neoplasm. Phagocytosis and interact with T cells |
|
|
Describe the structure and function of lymphocytes
|
Structure: small cells, round nucleus, thin blue rim of cytoplasm
Differentiation: 75% t lymphocytes – cellular immunity, processed by thymus. Recognise HLA –human leucocyte antigens and not react against them – self histiocompatibility molecules. CD4 expressing helper T cells recognise antigens attached to HLA and stimulate cytotoxic T cells expressing CD8 to recognise and kill virally infected host cells. CD4 expressing helper t cells also stimulate the transformation of B cells to plasma cells ( release immunoglobulins). B cells- humoral immunity Lymphocytes return to circulation via lymphatic system |
|
|
Describe the structure and function of platelets
|
Structure: small round non nucleated blue particles produced from megakaryocytes in bone marrow, complex surface membrane, cytoplasm contains alpha granules- fibrinogen, von willebrand’s factor and other large molecules and dense granules – small molecules ADP and calcium.
Function: platelet activation -> aggregation with other platelets and adhesion to damaged inner endothelial lining. Phospholipid surface to provide binding surface for clotting factors during activation of clotting cascade- fascilitate clotting, factor III on surface activates prothrombin to thrombin which converts fibrinogen to fibrin to form blood clot, release seretoninc to cause vasoconstriction |
|
|
Describe the structure of plasma
|
plasma contains large numbers of substances eg proteins – albumin, globulin, fibrinogens, and traces of mineral ions all dissolved in water (90% of plasma volume) and also fat molecules eg chylomicrons
|

