![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
202 Cards in this Set
- Front
- Back
|
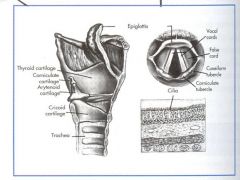
How many cartilages is the larynx formed by?
|
9
|
|
|
Name the 3 unpaired cartilages that form the larynx.
|
1. Thyroid
2. Cricoid 3. Epiglottis |
|
|
Name the 3 paired cartilages that form the larynx and characteristics of each.
|
1. Arytenoid - pyramid shaped; attached to vocal cords; responsible for opening and closing larynx
2. Corniculate - above arytenoids 3. Cuneiform - elongated pieces of cartilage in aryepiglottic folds |
|
|
ANATOMY - LARYNX CARTILAGES
|
|
|
|
The posterior crico-arytenoid muscles are the only ______ of the vocal cords.
|
abductors
PCA = pulls cords apart! |
|
|
The posterior crico-arytenoid muscles are innervated by the ______ ______ nerve.
|
recurrent laryngeal
|
|
|
How do the posterior crico-arytenoid muscles create glottic opening?
|
They create glottic opening by rotating arytenoid cartilages so vocal processes move laterally.
|
|
|
What muscles are the adductors of the vocal cords?
|
The lateral crico-arytenoid muscles.
|
|
|
The lateral crico-arytenoid muscles are innervated by the _______ ________ nerve.
|
recurrent laryngeal
|
|
|
How do the lateral crico-arytenoid muscles work to close the glottis?
|
They rotate the arytenoids medially to close the glottis.
|
|
|
What muscles tense the vocal cords? These muscles increase the distance between vocal process of the arytenoids and hyoid cartilage.
|
The cricothyroid muscles.
|
|
|
The cricothyroid muscles are innervated by the _______ branch of the ______ _______ nerve.
|
external; superior laryngeal
|
|
|
Which cranial nerve provides sensory to the mucous membranes of the nose, hard and soft palate, and anterior 2/3 of the tongue?
|
CN V - Trigeminal Nerve
|
|
|
Which cranial nerve provides motor to the tongue? Paralysis of this CN causes the tongue to deviate toward the affected side.
|
CN XII - Hypoglossal Nerve
|
|
|
Which cranial nerve provides sensory to the posterior 1/3 of the tongue, roof of the pharynx, undersurface of the soft palate, and gag reflex?
|
CN IX - Glossopharyngeal Nerve
|
|
|
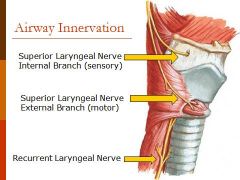
The vagus nerve (CN X) branches into the _________ ______ & _______ _________ nerves.
|
superior laryngeal; recurrent laryngeal
|
|
|
The superior laryngeal nerve divides into the 2 branches. What are the branches and which one is motor or sensory?
|
The external branch = motor nerve
The internal branch = sensory nerve |
|
|
The external nerve branch provides motor innervation to the __________ _______.
|
cricothyroid muscles - tensors of vocal cords
|
|
|
What is expected to be present if there is unilateral damage to the SLN external branch?
|
very subtle changes
|
|
|
What is expected to be present if there is bilateral injury to the SLN external branch?
|
hoarseness or tiring of voice; no airway problems
|
|
|
The internal branch of the SLN provides sensory supply between the _____ & _______.
|
epiglottis; cords
|
|
|
AIRWAY NERVE INNERVATION
|
|
|
|
What nerve innervates the larynx below the vocal cords and the trachea?
|
The recurrent laryngeal nerve.
|
|
|
The recurrent laryngeal nerve innervates ALL muscles of the larynx except the ___________ muscle. Which nerve innervates it?
|
cricothyroid muscle - innervated by the external laryngeal branch of the SLN
|
|
|
The RLN provides ______ to the posterior cricoarytenoid muscles which _____ the vocal cords.
|
motor; abduct
|
|
|
The RLN provides ______ to the lateral cricoarytenoid muscles which _______ the vocal cords.
|
motor; adduct
|
|
|
What does unilateral injury to the RLN cause?
|
Deterioration in voice.
|
|
|
What does bilateral injury of the RLN cause?
|
Stridor and respiratory distress.
|
|
|
REVIEW - NERVE INNERVATION & INJURY
1. The RLN & SLN are branches of the VAGUS.... 2. The CRICO-ARYTENOID MUSCLES are innervated by RLN... responsible for opening and closing cords.... 3. The CRICO-THYROID MUSCLES are innervated by the external branch of the SLN... responsible for tensing the cords.... |

|
|
|
The ______ extends from the lower end of the cricoid cartilage to the carina.
|
trachea
|
|
|
How many C-shaped cartilages support the trachea?
|
16-20 (closed posteriorly by tracheal muscles)
|
|
|
The trachea is approximately ___ inches long with 2 inches above the _________ _____ (3 inches with neck extension).
|
6; suprasternal notch
|
|
|
A tracheostomy is done between the _______ ______ and the ________ _______.
|
cricoid cartilage; suprasternal notch
|
|
|
What is the normal distance from incisors to larynx in adults?
|
~13 cm
|
|
|
What is the normal distance from the larynx to the carina in adults?
|
~13 cm
|
|
|
What is the normal distance from the incisors to the carina in adults?
|
~26 cm
|
|
|
Which bronchus is shorter (2.5 cm), wider (to supply larger lung), and more vertical (25 degree angle to trachea)?
|
The right mainstem.
|
|
|
Aspiration and endobronchial intubation are more likely in the ______ main bronchus.
|
right
|
|
|
Which bronchus is 5 cm long (passes under aortic arch), 45 degree angle (has to extend laterally behind arch to reach lung)?
|
The left main.
|
|
|
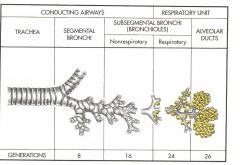
The right and left bronchi enter the lung at the hill or "roots" of lungs, branch into ______ bronchi, then into _______ bronchi, finally to the _______ bronchioles at sixteenth generation ("respiratory" bronchioles).
|
lobar; segmental; terminal
|
|
|
Name the 3 layers from the bronchial walls through terminal bronchioles.
|
1. Epithelial lining
2. Smooth muscle layer 3. Connective tissue layer |
|
|
What 2 types of cells are contained in the epithelial lining?
|
1. Goblet cells
2. Ciliated cells |
|
|
What is the function of goblet cells in the epithelial lining?
|
Goblet cells secrete mucous that keeps surfaces moist and traps small particles.
|
|
|
What is the function of ciliated cells in the epithelial lining?
|
The ciliated cells propel mucous blanket toward trachea and pharynx for elimination from airway.
|
|
|
What is the smooth muscle layer of the epithelial lining responsible for?
|
Responsible for dilation and constriction of airway.
|
|
|
The connective tissue layer of the epithelial lining contain cartilage in larger bronchi and bronchioles. What is the function of this cartilage?
|
The cartilage maintains patency of airway.
|
|
|
The terminal bronchioles of the connective tissue layer don't have cartilage. How are they kept expanded?
|
They are kept expanded by transpulmonary pressures (like alveoli).
|
|
|
ANATOMY - BRONCHI LAYERS
|

|
|
|
The bronchioles start with ____th through ____rd divisions.
|
16th; 23rd
|
|
|
Bronchioles have increasing or decreasing numbers of alveoli - respiratory bronchioles going from the 16th to the 23rd division.
|
increasing
|
|
|
What are characteristics of bronchioles?
|
1. Walls are thin.
2. No cilia or goblet cells. 3. Very little smooth muscle. 4. No cartilage - thin and elastic connective tissue. |
|
|
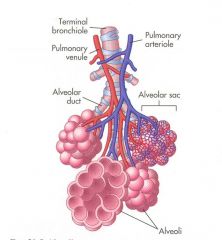
What structures are found at the end of the bronchioles?
|
Alveolar ducts
|
|
|
What is found at the end of alveolar ducts?
|
Alveolar sacs made up of alveoli.
|
|
|
TRACHEAL DIVISIONS
|
|
|
|
What is the main function of the alveoli?
|
They are the primary gas-exchange units of the lungs.
|
|
|
What are the 2 major types of epithelial cells in the alveolus?
|
1. Type I
2. Type II |
|
|
What is the function of the Type I epithelial cells in the alveolus?
|
Type I cells provide structure and are the most abundant (90%).
|
|
|
What is the function of the Type II epithelial cells in the alveolus?
|
Type II cells secrete surfactant (about 10% of alveolar epithelial cells); they can differentiate into Type I cells.
|
|
|
What does surfactant do?
|
It decreases surface tension; acts like a detergent
|
|
|
What is surfactant?
|
Surfactant is a lipoprotein that coats the inner surface of alveolus and facilitates expansion during inspiration.
|
|
|
What is meant by surfactant having a 'detergent like effect'?
|
It greatly reduces surface tension of water.
Reverses the law of Laplace (as radius expands, the tension in the wall structure will increase). Therefore, with surfactant present as the radius decreases, the surface tension decreases. Surfactant has a much weaker attraction than liquid. |
|
|
If surfactant production decreases, why is there a increased work of breathing?
|
Surfactant spreads over most of the surface of the inner surface of alveoli. If the production is decreased, the surface tension increases. The increase in surface tension causes the alveoli to collapse. Collapsed alveoli causes decreased lung expansion, therefore increased work of breathing.
|
|
|
Define surface tension.
|
Surface tension refers to the tendency for liquid molecules to adhere to one another. An example is water at the top of a glass about to overflow. Water "bead" up when splashed on water proof surface. An area that is exposed to air has decreased surface tension.
|
|
|
In a sphere, does surface tension make expansion easier or difficult?
|
difficult
|
|
|
What is the equation for the Law of Laplace?
|
P=2 (surface tension) / radius
* As the sphere gets bigger, pressure goes down. As radius of sphere becomes smaller, more pressure is required to inflate it. * Surfactant causes this to be reversed - as the sphere gets smaller, the pressure decreases. |
|
|
Define the pores of Kohn.
|
The pores of Kohn are tiny passages that allow ome air to pass through the septa from one alveoli to another. They promote collateral ventilation and even distribution of air among alveoli - if the bronchioles become obstructed, can still ventilate.
|
|
|
The alveolus and capillary are divided by the _______ ______.
|
interstitial space
|
|
|
Name and explain 2 disease processes that make diffusion of oxygen and carbond dioxide difficult across the interstitial space between the alveolus and capillary.
|
1. Pulmonary edema - fluid is in the interstitial space.
2. Pulmonary fibrosis - the interstitial space hardens and doesn't allow diffusion. |
|
|
FACTS ABOUT THE RESPIRATORY MEMBRANE
|
1. Even with all layers, the membrane only averages 0.6 micrometers thick.
2. Total surface area of the membrane is 70 m2 (equal to 25x30 foot room). 3. Total amount of blood in pulmonary capillaries is 60-140 ml (small amount of blood over a 25x30 ft room) - very rapid exchange of oxygen and carbon dioxide. 4. Average diameter of pulmonary capillary is 5 micrometers - RBC average size is 2.5 to 7 micrometers so RBCs squeeze through. |
|
|
Why can gases diffuse between alveolus and RBC without passing through plasma?
|
Due to RBCs squeezing through the respiratory membrane, the RBC membrane usually touches the capillary wall.
|
|
|
What is defined as double-walled membrane covering the lung?
|
Pleura
|
|
|
Name the 2 layers of the pleura.
|
1. Visceral pleura.
2. Parietal pleura. |
|
|
The visceral pleura is tightly adherent to the surface of the lung. What is the function of the visceral pleura?
|
It absorbs lymph (serous fluid in the pleural cavity).
|
|
|
What is the function of lymph in the pleural cavity?
|
It allows for decreased friction on the lungs when inhaling and exhaling.
|
|
|
The parietal pleura lines the chest wall and diaphragm. What is the function of the parietal pleura?
|
It forms lymph.
|
|
|
Why do we feel pain from inflammation of the pleura?
|
The parietal pleura is very sensitive to pain due to the rich supply of somatic afferent visceral nerve fibers that innervate it.
Pain would not be felt from inflammation of the visceral pleura because it is insensitive to pain – its afferent fibers relay stretch sensations only. |
|
|
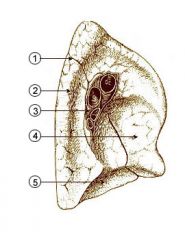
The 2 layers of the pleura meet at the ______.
|
hilum - Above and behind the cardiac impression is a triangular depression named the hilum, where the structures which form the root of the lung enter and leave the viscus. These include the pulmonary artery, superiormost on the left lung, the superior and inferior pulmonary veins, lymphatic vessels and the bronchus, with bronchial vessels surrounding it (Wikipedia)
|
|
|
REVIEW HILUM OF THE LUNG (SHOWS LEFT LUNG HILUM)
1. Oblique fissure 2. Vertebral part 3. HILUM OF LUNG 4. Cardiac impression 5. Diaphragmatic surface |
|
|
|
Layers of the pleura slide over each other aided by small amount of serous fluid in the pleural cavity. How does this effect the lungs?
|
It creates a partial vacuum of negative pressure which helps aid in lung expansion.
|
|
|
What happens to the lungs if negative pressure is lost?
|
Lungs collapse.
|
|
|
What is the space between the layers of the pleura called?
|
The pleural cavity.
|
|
|
Increased pressure on the venous side of the pleura can cause fluid to collect (pleural effusion). Which patient population do we think of with pleural effusions?
|
Lung cancer patients.
Malignant pleural effusion can develop around the lungs as a complication of lung cancer. |
|
|
How do pleural effusions affect ventilation?
|
Pleural effusion is excess fluid that accumulates between the two pleural layers, the fluid-filled space that surrounds the lungs. Excessive amounts of such fluid can impair breathing by limiting the expansion of the lungs during ventilation (Wikipedia).
|
|
|
What are the differences between pulmonary and systemic arteries?
|
1. Pulmonary arteries have larger diameters, thinner walls, and are more distensible.
2. Pulmonary circulation is a low pressure system so it can accept CO at all times. It doesn't have to have direct blood flow to all body like systemic circulation (can perform at low pressures). |
|
|
What are the differences between pulmonary and systemic arteries?
|
1. Pulmonary arteries have larger diameters, thinner walls, and are more distensible.
2. Pulmonary circulation is a low pressure system so it can accept CO at all times. It doesn't have to have direct blood flow to all body like systemic circulation (can perform at low pressures). |
|
|
PULMONARY CIRCULATION:
* PA divides and enters lung at hilus with each main bronchus * Branches with bronchus at every division * Every bronchus or bronchiole accompanied by artery or arteriole * Arterioles regulate blood flow through capillary bed * Arterioles divide at terminal bronchiole to form capillaries around alveoli *Each pulmonary vein drains several capillaries * Dispersed randomly throughout lung * Leave lung at hilum and enter LA * Similar to veins in systemic circulation but no valves |
|
|
|
What 3 areas does bronchial circulation supply?
|
1. Lung tissue
2. Visceral pleura 3. Lymph nodes |
|
|
During bronchial circulation, veins empty deoxygenated blood into the _____ _____. This contributes to normal physiologic shunt.
|
left atrium
|
|
|
Bronchial circulation receives approximately ___% of cardiac output.
|
3%
|
|
|
What are small veins in the heart that drain used blood into the endocardium of the nearest chamber? They are also part of bronchial circulation.
|
Thesbian veins
|
|
|
Thesbian veins empty into all heart chambers deoxygenated blood from heart tissue. They mainly empty into which side of the heart?
|
right heart
|
|
|
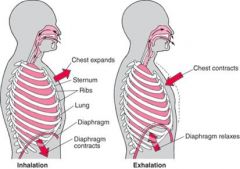
During _________, the diaphragm contracts (lower surfaces of the lungs are pulled down).
|
inspiration
|
|
|
During __________, the diaphragm relaxes (elastic recoil of lungs, chest wall, and abdomen compress the lungs).
|
expiration
|
|
|
MECHANICS OF BREATHING
|
|
|
|
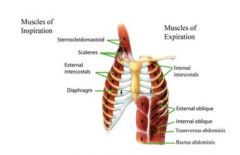
The muscles of inspiration increase chest cage size. Name the muscles of inspiration.
|
MAJOR: diaphragm; EXTERNAL intercostals (elevates anterior ribs)
ACCESSORY: sternocleidomastoid (lifts sternum); anterior serati (lifts ribs); scaleni (raises first two ribs) |
|
|
The muscles of expiration depress the chest cage. Name the muscles of expiration.
|
NO MAJOR MUSCLES OF EXPIRATION.
ACCESSORY: abdominis rectus; INTERNAL intercostals (when MV high, coughing, airway obstruction) |
|
|
MECHANICS OF BREATHING: MUSCLES OF INSPIRATION AND EXPIRATION
|
|
|
|
What makes elastic properties (recoil & compliance) important in the lungs?
|
Permits the lung and chest to expand during inspiration and return to resting volume during expiration.
|
|
|
What tends to happen is the elastic properties of the lungs become defected?
|
1. Lungs tend to collapse.
2. Chest tends to expand outward. 3. Opposing forces create increase in negative pressure. |
|
|
Recoil (desire to return to resting state after inspiration) in the lungs is caused by what 4 things?
|
1. Elastin fibers in alveolar walls, small airways, and pulmonary capillaries.
2. Surface tension in alveoli. 3. Surfactant lowers surface tension. 4. Surfactant is more concentrated in smaller alveoli to prevent their collapse. |
|
|
Recoil of the lungs occurs in the chest wall by what 2 structures?
|
1. Ribs
2. Muscles |
|
|
Recoil permits passive expiration without the need for major muscles of expiration. When are accessory muscles used?
|
If disease compromises recoil (emphysema) or blocks airways.
|
|
|
What term describes the measure of chest wall and lung distensibility?
|
Compliance
|
|
|
Compliance determines how easily structures can be "stretched". A patient with emphysema alveoli stay open, therefore their compliance is increased or decreased?
|
Increased or floppy
|
|
|
Abnormally easy to inflate or "stretch" = _______ compliance.
|
increased
|
|
|
More difficult to inflate = _______ compliance.
|
decreased
|
|
|
Resistance in the lungs/conducting airways is usually very low and is measured by PFTs. Where is resistance greatest?
|
Nose
|
|
|
Name 3 things that increase resistance.
|
1. Edema
2. Obstruction 3. Bronchospasms |
|
|
Describe the effects of anesthesia on pulmonary mechanics related to....
1. Supine position 2. Induction of anesthesia 3. Chest and lung compliance 4. Resistance |
1. Supine position decreases FRC by 15-20%.
2. Induction of anesthesia decreases FRC by 15-20% - so total decrease of 30-40% in asleep, supine patient. 3. Chest and lung compliance reduced. 4. Effects on resistance usually not a problem. |
|
|
Lung Volumes: What is residual volume (RV)? What is the normal value?
|
The volume remaining after maximum expiration.
1200 ml |
|
|
Lung Volumes: What is expiratory reserve volume (ERV)?
|
The maximum volume exhaled from resting end-expiratory level.
|
|
|
Lung Volumes: What is tidal volume (TV or Vt)? What is the normal value?
|
The volume in or out with each quiet breath.
500 ml |
|
|
Lung Volumes: What is inspiratory reserve volume? What is the normal value?
|
The maximum volume inspired from end-insp. level.
3000 ml |
|
|
Lung Capacities (Combination of 2 or more volumes): What is inspiratory capacity? What is the normal value?
|
The maximum volume inspired from end-exp. level.
IC = IRV + Vt (3500ml = 3000 + 500) |
|
|
Lung Capacities: What is vital capacity? What is the normal value?
|
The maximum volume expired from maximum insp. level. Everything but FRC included.
VC = IRV + Vt + ERV (4500ml = 3000 + 500 + 1000) |
|
|
Lung Capacities: What is functional residual capacity (FRC)? What is the normal value?
|
The volume remaining at end-exp. level.
FRC = RV + ERV (2300ml = 1200 + ~1100) With each Vt, only get about 1/7 of FRC exchange. Example: 2 mm/kg is going to be dead space... If patient is getting 500 TV and pt weighs 140 kg, then only getting 220ml gas exchange. |
|
|
Lung Capacities: What is total lung capacity? What is the normal value?
|
The volum in the lungs after maximum inspiration. Includes everything.
TLC = IRV + Vt + ERV + RV (5800ml = 3000 + 500 + 1100 + 1200) |
|
|
What are pulmonary function tests used to indicate?
|
The dynamic function of the lungs.
|
|
|
What 4 parameters are used to compute normal values on PFTs?
|
1. Weight
2. Height 3. Sex 4. Age Interpretation deprends on patient's effort. |
|
|
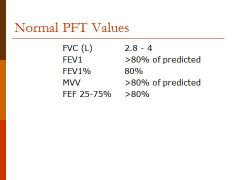
PFTs: What is forced vital capacity (FVC)? What is the normal value?
|
The amount of air forcefully expelled after maximal inspiration.
Normal 55-85 ml/kg (2.8-4 L) |
|
|
Restrictive disease is indicated if the FVC is (what value)?
|
Less than 80%
FVC may be 100% or greater in mild to moderate obstructive disease - but can decrease with severe COPD. Need at least 1 L to generate cough. |
|
|
PFTs: What is forced expiratory volume in one second (FEV1)?
|
Measures the amount of air exhaled in first second of FVC.
Healthy patients 75-80% of FVC. FEV1 decreased in obstruction. |
|
|
Forced Expiratory Volume Percent (FEV1%) compares ____ and ____.
|
FEV1%; FVC
FEV1% / FVC |
|
|
FEV1% < 70% indicates _________ disease - especially in larger airways.
|
obstructive
|
|
|
In restrictive disease FEV1% is usually _______ (value).
|
normal
|
|
|
What is the volume a patient can breathe as quickly as possible through a low pressure system during 15 seconds?
|
Maximal Voluntary Ventilation (MVV)
|
|
|
Maximal voluntarty ventilation is very dependent on patient effort. What is the normal value and how can it be estimated?
|
Normal 150 Liters/minute
Can be estimated by multiplying FEV1 by 30. |
|
|
What is forced expiratory flow (25-75%)?
|
It measures the mean rate of flow over the middle half of FVC. It evaluates emptying of the smaller airways.
|
|
|
Forced expiratory flow is normally ___% of predicted. If it is less it indicates _________ disease in smaller airways.
|
80; obstructive
|
|
|
NORMAL PFT VALUES
|
|
|
|
INDICATORS FOR HIGH-RISK
|
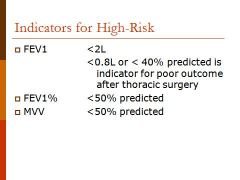
|
|
|
RESTRICTIVE VS. OBSTRUCTIVE DISEASE
|
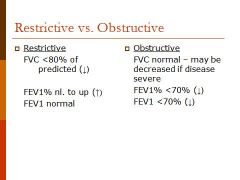
|
|
|
OBSTRUCTIVE DISORDERS / RESTRICTIVE DISORDERS
|
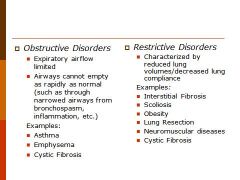
|
|
|
What does it mean if a lung disease is called intrinsic or extrinsic?
|
Intrinsic (or interstitial) - disease within the lung itself
Extrinsic - outside the lung |
|
|
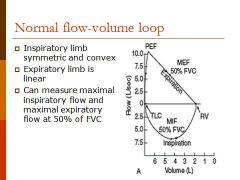
Flow volume loops shows ______ _____ ______.
|
forced vital capacity
Flow volume loops are produced by plotting flow on the y axis (liters/second) against volume on the x axis (liters). |
|
|
What do flow volume loops record?
|
They record the maximum flow when a patient inspires rapidly from residual volume (RV) to total lung capacity (TLC) and then exhales as hard as possible back to residual volume.
|
|
|
NORMAL FLOW-VOLUME LOOP
*Start at RV* |
|
|
|
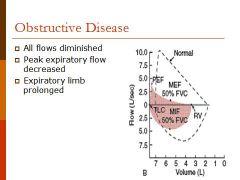
OBSTRUCTIVE DISEASE
*Have more air at RV (It's obstructive disease so can't get air out)* |
|
|
|
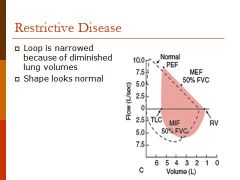
RESTRICTIVE DISEASE
*Shape looks normal - just smaller* *Don't have as much RV* |
|
|
|
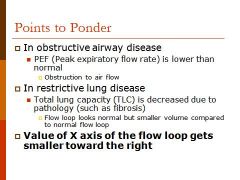
POINTS TO PONDER REGARDING OBSTRUCTIVE AND RESTRICTIVE DISEASE...
|
|
|
|
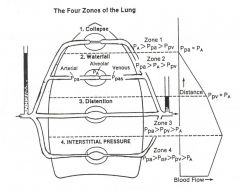
Ventilation & Perfusion: Distribution of blood flow is dependent upon?
|
Gravity
|
|
|
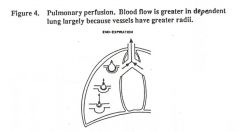
Ventilation & Perfusion: Describe the relationships that the amount of blood flow depends on in pulmonary perfusion.
|
The amount of flow depends on the relationship between pressure in the pulmonary artery (Ppa), pressure in alveoli (PA), and pressure in the pulmonary vein (Ppv).
|
|
|
PULMONARY PERFUSION
|
|
|
|
WEST'S ZONES OF THE LUNGS
|
|
|
|
Which zone always has perfusion and the ideal place for pulmonary catheter?
|
Zone 3
|
|
|
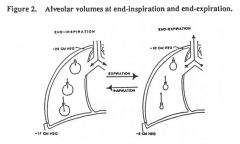
Regarding distribuation of ventilation, alveolar pressure is the same throughout the lung. Is there more ventilation to the dependent or nondependent areas?
|
Dependent
Alveoli are smaller, but can expand more (by 80% in dependent lung compared to 20% in nondependent lung). Intrathoracic pressure is more negative at the apex than at the base so the alveoli in the apex remain more open. |
|
|
LaDonna had: REVIEW POSITIONING AND V/Q!! Here are some things found in an article by Dr. Lauren Barker & Karen Johnson, RN, PhD.
|
SUPINE: In the supine position, ventilation and perfusion are greater in dependent areas of the lungs
than in the anterior areas. In healthy lungs, adequate matching of ventilation and perfusion (V/Q match) can be achieved in the supine position. In diseased lungs, prolonged placement in the supine position can alter the V/Q match. For example, excess fluid associated with pulmonary edema accumulates in the dependent areas of the lungs and interferes with diffusion of gases across the alveolarcapillary membranes. Perfusion, however, remains constant in the dependent areas. Therefore, there is a V/Q mismatch that results in an intrapulmonary shunt. |
|
|
LaDonna had: REVIEW POSITIONING AND V/Q!! Here are some things found in an article by Dr. Lauren Barker & Karen Johnson, RN, PhD.
|
TRENDELENBERG: Increased venous return. Lung compliance and functional residual capacity (FRC) are decreased with increased V/Q mismatch, especially in obese patients (IPPV may be preferable to SV).
|
|
|
LaDonna had: REVIEW POSITIONING AND V/Q!! Here are some things found in an article by Dr. Lauren Barker & Karen Johnson, RN, PhD.
|
REVERSE TRENDELENBERG: Reduced venous return in this position may lead to a fall in cardiac output and arterial pressure. As baroreceptor activity is reduced under anaesthesia a vasopressor may be needed. Blood pressure readings should be interpreted in the context of relative positions of the blood pressure cuff and the level of the brain above it. Functional residual capacity (FRC) is improved.
|
|
|
LaDonna had: REVIEW POSITIONING AND V/Q!! Here are some things found in an article by Dr. Lauren Barker & Karen Johnson, RN, PhD.
|
PRONE: V/Q is improved. Aeration improves because the heart does not compress the lung like in supine positioning.
|
|
|
LaDonna had: REVIEW POSITIONING AND V/Q!! Here are some things found in an article by Dr. Lauren Barker & Karen Johnson, RN, PhD.
|
LITHOTOMY: Vital capacity is decreased.
|
|
|
LaDonna had... REVIEW POSITIONING AND V/Q!! Here are some things found out of article by Dr. Lauren Barker.
|
LATERAL: The lateral position alters respiratory physiology: if breathing spontaneously, the dependent (lower) lung is efficiently perfused and ventilated. But with IPPV the dependent lung is better perfused and the non-dependent (upper) lung better ventilated, resulting in V:Q mismatch.
|
|
|
In an awake, spontaneously breathing patient, ventilation is best in the ___________ lung.
|
dependent
|
|
|
ALVEOLAR VOLUMES AT END-INSPIRATION & END-EXPIRATION
AT END-INSPIRATION: * At top alveoli - partially inflated at all times because increase in intrathoracic pressure. * At bottom alveoli - negative pressure is less so it is more collapsed. |
|
|
|
V/Q Spontaneously Breathing: More blood flow and ventilation to gravity-dependent part of lung. Nondependent areas get less ventilation and perfusion. V/Q ratios vary widely throughout the lung, ideal ratio is 1 - at 3rd rib...
Above area, V>Q = V/Q > 1 = _________. Below area, V<Q = V/Q < 1 = ______. |
deadspace
shunt |
|
|
V/Q ratio averages ____ g/L.
|
0.8 g/L
Ventilation normally 4 g/min. Perfusion normally 5 L/min. 4/5 = 0.8 g/L "V" – ventilation – the air which reaches the alveoli."Q" – perfusion – the blood which reaches the alveoli. These two variables constitute the main determinants of the blood oxygen concentration. In fact since V determines the quantity of oxygen mass reaching the alveoli per minute (g/min) and Q expresses the flow of blood in the lungs (l/min), the V/Q ratio refers to a concentration (g/l). |
|
|
Alveolar to Alveolar Blood Gradient:
Normal PAO2 to PaO2 gradient on room air = 5-15 mmHg. Normal gradient on 100% O2 is up to (not over) 100 mmHg. Normal PaCO2 to PACO2 gradient = 2-10 mmHg regardless of FiO2. If either gradient is higher than normal, V/Q mismatch is the cause of ________. |
hypoxia
|
|
|
To estimate PaO2 in a healthy patient, multiply FiO2 by __.
|
5
arterial O2 |
|
|
To estimate PAO2 in a healthy patient, multiply FiO2 by __.
|
6
alveolar O2 |
|
|
About _____ mL of oxygen is transported to cells per minute.
|
1000
|
|
|
Oxygen is tranported in 2 forms. What are the 2 forms and what percentage makes up each?
|
Bound to Hgb - 97%
Dissolved in plasma - 3% |
|
|
About _____ mL of oxygen is transported to cells per minute.
|
1000
|
|
|
Each gram of Hgb can bind with a maximum of ____ mL of O2.
|
1.34
1.39 mL if Hgb is pure form - purity is decreased by other forms of Hgb. |
|
|
Oxygen is tranported in 2 forms. What are the 2 forms and what percentage makes up each?
|
Bound to Hgb - 97%
Dissolved in plasma - 3% |
|
|
Example problem:
If Hgb is 15 g/dL, then there are 15 grams in 100 mL of blood. What is the O2 content in 100 mL of blood when 100% saturated? |
15 x 1.34 mL = 20.1 mL of O2 in 100 mL of blood when 100% saturated.
|
|
|
Each gram of Hgb can bind with a maximum of ____ mL of O2.
|
1.34
1.39 mL if Hgb is pure form - purity is decreased by other forms of Hgb. |
|
|
Total O2 content includes combined with Hgb and that dissolved in plasma. The amount dissolved in plasma is 0.3 mL/dL if pO2 is 100. What is the formula for determining total oxygen content?
|
O2 content = (Hgb x SaO2 x 1.34) + (PaO2 x 0.003)
|
|
|
Example problem:
If Hgb is 15 g/dL, then there are 15 grams in 100 mL of blood. What is the O2 content in 100 mL of blood when 100% saturated? |
15 x 1.34 mL = 20.1 mL of O2 in 100 mL of blood when 100% saturated.
|
|
|
Total O2 content includes combined with Hgb and that dissolved in plasma. The amount dissolved in plasma is 0.3 mL/dL if pO2 is 100. What is the formula for determining total oxygen content?
|
O2 content = (Hgb x SaO2 x 1.34) + (PaO2 x 0.003)
|
|
|
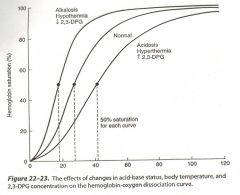
What relationship does the oxyhemoglobin-dissociation curve represent?
|
Shows the relationship between PaO2 and SaO2 - how much Hgb is saturated with O2 for a given partial pressure.
Looks at affinity for O2. |
|
|
Oxy-hgb Dissociation Curve: Name 5 factors that alter O2 binding.
|
1. H+ ion concentration.
2. CO2 tension. 3. Temperature. 4. 2,3-disphosphoglycerate (2,3-DPG). 5. Presence of abnormal Hgb. |
|
|
What relationship does the oxyhemoglobin-dissociation curve represent?
|
Shows the relationship between PaO2 and SaO2 - how much Hgb is saturated with O2 for a given partial pressure.
Looks at affinity for O2. |
|
|
Oxy-hgb Dissociation Curve: Name 5 factors that alter O2 binding.
|
1. H+ ion concentration.
2. CO2 tension. 3. Temperature. 4. 2,3-disphosphoglycerate (2,3-DPG). 5. Presence of abnormal Hgb. |
|
|
OXYHEMOGLOBIN-DISSOCIATION CURVE
* Each Hgb can hold 4 molecules of O2. * Remember 4, 5, 6, 7, 8, 9... PaO2 is 40 then SaO2 70%... PaO2 is 50 then SaO2 80%... PaO2 is 60 then SaO2 90%... |
|
|
|
P50 = PaO2 at which Hgb is 50% saturated with O2. What is the normal P50 in adults?
|
27 mmHg
When SaO2 is 50%, PaO2 is 27. |
|
|
With increased P50, the curve shifts to the _____. Hgb's affinity for O2 ________ (more available for tissues).
|
right; decreases
|
|
|
Name 4 conditions that shift the curve to the right.
|
1. Acidosis.
2. Increased CO2. 3. Hyperthermia. 4. Increased 2,3-DPG. *2,3-DPG is a by-product of glycolysis. *It accumulates during anaerobic metabolism. *It normally keeps the curve shifted to the right. *It rises during hypoxia, shifting the curve even further. |
|
|
With decreased P50, the curve shifts to the ____ and Hgb's affinity for O2 _________ (less available for tissues).
|
left; increases
|
|
|
Name 5 conditions that shift the curve to the left.
|
1. Alkalosis.
2. Decreased CO2. 3. Hypothermia. 4. Decreased 2,3-DPG. 5. Presence of abnormal Hgb (fetal and met-hgb). |
|
|
Normally __ mL of CO2 is transported from tissues to lungs in each 100 mL of blood.
|
4
70% reacts with H2O for transport; 23% combines with Hgb; 7% is dissolved. |
|
|
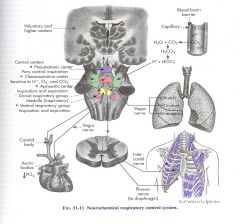
The respiratory center located in the ______ _____ controls respiration.
|
brain stem
|
|
|
The respiratory center transmits impulses to respiratory muscles and is composed of several groups of neurons located bilaterally in the brain stem. Name the 4 groups of neurons.
|
1. Dorsal respiratory group (DRG)
2. Ventral respiratory group (VRG) 3. Pneumotaxic center 4. Apneustic center |
|
|
NEUROCHEMICAL RESPIRATORY CONTROL SYSTEM
|
|
|
|
The dorsal respiratory group is responsible mainly for ___________.
|
inspiration
|
|
|
The dorsal respiratory group is located in the _______ _______ in the nucleus of tractus solitarius.
|
dorsal medulla
|
|
|
The dorsal respiratory group receives ________ impulses from peripheral chemoreceptors, baroreceptors, and receptors in the lungs.
|
afferent
|
|
|
The dorsal respiratory group sends efferent signals to the ___________ and _________.
|
diaphragm; intercostals
|
|
|
The dorsal respiratory group is responsible for ___________ rhythm of respiration.
|
automatic
DRG = automatic respirations |
|
|
The pneumotaxic center is located in the _______ _____.
|
upper pons
|
|
|
Where does the pneumotaxic center transmit signals to?
|
Dorsal respiratory group (DRG)
|
|
|
What does the pneumotaxic center cause the DRG to do?
|
It causes the DRG to end inspiration.
|
|
|
The ventral respiratory group (VRG) is located in the _______ near the DRG.
|
medulla
|
|
|
What causes signals from the DRG spill over into the VRG?
|
When increase ventilation is needed.
|
|
|
The apneustic center is located in the _______ ____.
|
lower pons
|
|
|
Where does the apneustic center send signals to and for what response?
|
Sends signals to the DRG to continue or sustain inspiration.
|
|
|
Name the 3 types of lung receptors and where they are located.
|
1. Irritant - in epithelium of conducting airways.
2. Stretch - in smooth muscles. 3. J-receptors - near capillaries in alveolar septa. |
|
|
What do chemoreceptors monitor in arterial blood?
|
pH; PaCO2; PaO2
|
|
|
What do central chemoreceptors sense change of?
|
Central chemoreceptors sense changes in pH of CSF - H+ ion concentration reflects PaCO2. (Increase PaCO2 leads to increase H+ ions)
|
|
|
Peripheral chemoreceptors are located where?
|
aortic bodies; aortic arch; carotid bodies
|
|
|
What are peripheral chemoreceptors mostly sensitive to?
|
PaO2.
Peripheral chemoreceptors are sensitive to pH and PaCO2 but mostly to PaO2. |
|
|
What are the effects of anesthesia on the respiratory center?
|
1. GA causes a decrease in central chemoreceptor's response to PaCO2.
2. Peripheral chemoreceptors response is eliminated by as little as 0.1 MAC. |
|
|
What are the effects of volatiles and narcotics on rate and Vt?
|
Volatiles: respirations rapid and shallow.
Narcotics: respirations longer and deeper. |

