![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
“I’m having trouble breathing.”
HPI: WF is a 55 yo man who present to the ED c/o increasing SOB. The patient states that he was well until approximately four days ago when he began experiencing SOB with minimal exertion. He also reports that his coughing has increased and that his sputum color has turned from clear to yellow. PMH: chronic bronchitis x 10 years; hospitalized three times in the past year for acute exacerbations; HTN FH: mother is alive and well; father is alive and also has HTN SH: currently unemployed, previous smoker of two cigars a day x 30 years, quit 1 year gago; occasional alcohol Meds Ipratropium bronmide MDI 2 puffs QID Albuterol MDI 2 puffs QID PRN HCTZ/triamterene 25 mg/37.5 mg PO daily Allergies NKDA ROS: SOB with productive cough (yellow sputum), denies fever or chills PE Gen: paitent is a well nourished man in mild respiratory distress VS: BP 134/82 mmHg left arm sitting, P 106 RR 24 T 36.4 C Lungs: decreased breath sounds BL; air movement decreased markedly; inspiratory and expiratory wheezes LBL without any rales or rhonchi Ext: Co CCE Remainder of PE normal Labs: Hgb 17.5 Hct 51.9% WBC 11.2 with 67% PMNs, 4% bands, 19% lymphs, 10% monos ABG: pH 7.42, PCO2 46 PO2 61 SaO2 93% on room air CXR: increased bronchovascular markings in the lower lung fields consistent with COPD, no effusions of infiltrates What risk factors does this individual have the COPD? What signs, symptosm and labs indicate acute exacerbation of COPD What additional information is necessary to completely evaluate theis paitnt? Which bacterial organisms are usually responsible for exacerbation fo COPD? What the tx goals? What tx alternatives? Design a paln for actue exacerbation. Describe montiorign parameters ? |
“I’m having trouble breathing.”
HPI: WF is a 55 yo man who present to the ED c/o increasing SOB. The patient states that he was well until approximately four days ago when he began experiencing SOB with minimal exertion. He also reports that his coughing has increased and that his sputum color has turned from clear to yellow. PMH: chronic bronchitis x 10 years; hospitalized three times in the past year for acute exacerbations; HTN FH: mother is alive and well; father is alive and also has HTN SH: currently unemployed, previous smoker of two cigars a day x 30 years, quit 1 year ago; occasional alcohol Meds Ipratropium bronmide MDI 2 puffs QID Albuterol MDI 2 puffs QID PRN HCTZ/triamterene 25 mg/37.5 mg PO daily Allergies NKDA ROS: SOB with productive cough (yellow sputum), denies fever or chills PE Gen: paitent is a well nourished man in mild respiratory distress VS: BP 134/82 mmHg left arm sitting, P 106 RR 24 T 36.4 C Lungs: decreased breath sounds BL; air movement decreased markedly; inspiratory and expiratory wheezes LBL without any rales or rhonchi Ext: Co CCE Remainder of PE normal Labs: Hgb 17.5 Hct 51.9% WBC 11.2 with 67% PMNs, 4% bands, 19% lymphs, 10% monos ABG: pH 7.42, PCO2 46 PO2 61 SaO2 93% on room air CXR: increased bronchovascular markings in the lower lung fields consistent with COPD, no effusions of infiltrates What risk factors does this individual have the COPD? Previous smoker What signs, symptoms and labs indicate acute exacerbation of COPD Increased intensity of sx, h/o frequent exacerbations (hospitalized 3 x in past year), mild respiratory distress (decreased breath sounds, markedly decreased air movement, general appearance of distress, pO2 dropping and pCO2 rising suggests risk for pending respiratory failure, however, not currently in respiratory distress as the SaO2 is > 90% on room air. What additional information is necessary to completely evaluate this patient? Spirometry Which bacterial organisms are usually responsible for exacerbation fo COPD? SKIP this question. Covered on p240 of textbook. Note different microbes depending on severity of exacerbation and COPD. What the tx goals? Prevent respiratory failure Treat underlying pulmonary infection What tx alternatives? Antibiotics Bronchodilators Systemic corticosteroids Inhaled corticosteroids Oxygen Design a plan for acute exacerbation. Start 30-40 mg prednisolone PO daily x 7-10 days After complete, add ICS Recommend pulmonary rehab Describe monitoring parameters ? Spirometry, SaO2, ABGs in two weeks after completion of PO steroid treatment Symptom resolution daily Sputum culture after antibiotic regimen complete |
|
|
COPD Textbook case
A 49 y.o. man with a PMH of HTN presents to the clinic c/o SOB that began about 3-4 years ago. His sx have gradually gotten worse since then. He is now unable to walk 100 yards without have to stop and rest. He also has a daily cough that is usually productive of yellowish sputum. He smokes about 11/2 ppd and has done so x the past 30 years. He also drinks on average 6-7 beers a day. He does not have any significant occupational exposures to dust, gases, or fumes. What info is suggestive of COPD? What risk factors does he have for COPD? What additional information do you need to know before creating a treatmen plan for this patient? |
COPD Textbook case
A 49 y.o. man with a PMH of HTN presents to the clinic c/o SOB that began about 3-4 years ago. His sx have gradually gotten worse since then. He is now unable to walk 100 yards without have to stop and rest. He also has a daily cough that is usually productive of yellowish sputum. He smokes about 11/2 ppd and has done so x the past 30 years. He also drinks on average 6-7 beers a day. He does not have any significant occupational exposures to dust, gases, or fumes. What info is suggestive of COPD? SOB that is chronic (3-4 years) with evidence of progression (“gradually worse”). Productive daily cough with yellow sputum Smokes 1 and ½ ppd x 30 years. [study hint: see box “Key Indicators for COPD” ] What risk factors does he have for COPD? Tobacco smoke What additional information do you need to know before creating a treatment plan for this patient? PMH: any h/o asthma, allergy, sinusitis, etc FH History of exacerbations or previous hospitalizations Comorbidities (heart disease, osteoporosis, malignancies) Impact of sx on functioning Social and family support available Tests: Reversibility testing to rule out (r/o) asthma CXR to r/o tuberculosis, pneumonia, heart failure ABGs (only if FEV1 < 50%) SaO2 on room air Spirometry (FEV1, FVC, FVC/FEV1) Alpha-1 antitrypsin (only if < 45 y.o.a. with FH of COPD) Medication allergies |
|
|
Part 2
PMH: HTN x 6 years, currently controlled SH: works as an accountant, married with two children FH: father with emphysema and lung cancer. There is no family h/o DMType2 or heart disease Meds: lisinopril 40 mg PO once daily; HCTZ 25 mg PO once daily ROS: (-) skins rash, (-) nasal congestion, drainage; (-) chest pain, paroxysmal nocturnal dyspnea, orthopnea; (+) SOB, cough, intermittent wheezing; (-) hemoptysis; (-) heartburn, reflux sx, N/V/D, change in appetite, change in bowel habits; (-) joint pain or swelling; (-) pedal edema PE: VS: BP 134/82 mm Hg, P 80 bpm, RR 20 /min T 35.8 C Wt 132# Ht 64 in BMI 22.7 HEENT: EOMI; mucosal membranes are moist; no evidence of JVD; no palpably enlarged cervical lymph nodes. Lungs: barrel-shaped chest; hyperresonant percussion noted BL; lung sounds are fairly distant, no rhonchi or crackles. CV: RRR, normal heart sounds ABD: soft, non-tender, no hepatomegaly EXT: no cyanosis, edema, or finger clubbing; evidence of onychomycosis on all fingernails PFTS Prebronchodilator Postbronchodilator Actual % Predicted Actual % Predicted FVC (L) 4.4 107% 4.0 97% FEV1 (L) 1.68 50% 1.59 47% FEV1/FVC 39% CXR: hyperlucency and hyperinflation of the lungs suggestive of emphysematous change What is your assessment of this person’s COPD? What stage of COPD? List treatment goals for his COPD. What nonpharmacologic and pharmacologic interventions would you recommend? |
Part 2
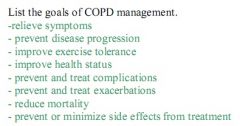
PMH: HTN x 6 years, currently controlled SH: works as an accountant, married with two children FH: father with emphysema and lung cancer. There is no family h/o DMType2 or heart disease Meds: lisinopril 40 mg PO once daily; HCTZ 25 mg PO once daily ROS: (-) skins rash, (-) nasal congestion, drainage; (-) chest pain, paroxysmal nocturnal dyspnea, orthopnea; (+) SOB, cough, intermittent wheezing; (-) hemoptysis; (-) heartburn, reflux sx, N/V/D, change in appetite, change in bowel habits; (-) joint pain or swelling; (-) pedal edema PE: VS: BP 134/82 mm Hg, P 80 bpm, RR 20 /min T 35.8 C Wt 132# Ht 64 in BMI 22.7 HEENT: EOMI; mucosal membranes are moist; no evidence of JVD; no palpably enlarged cervical lymph nodes. Lungs: barrel-shaped chest; hyperresonant percussion noted BL; lung sounds are fairly distant, no rhonchi or crackles. CV: RRR, normal heart sounds ABD: soft, non-tender, no hepatomegaly EXT: no cyanosis, edema, or finger clubbing; evidence of onychomycosis on all fingernails PFTS Prebronchodilator Postbronchodilator Actual % Predicted Actual % Predicted FVC (L) 4.4 107% 4.0 97% FEV1 (L) 1.68 50% 1.59 47% FEV1/FVC 39% CXR: hyperlucency and hyperinflation of the lungs suggestive of emphysematous change What is your assessment of this person’s COPD? Stage III COPD with reduced exercise capacity as evidenced by unable to walk 100 yards, FEV1 < 50%, at risk for respiratory failure What stage of COPD? 3 List treatment goals for his COPD. Relieve symptoms Prevent disease progression Improve exercise tolerance Improve health status Prevent complications Prevent exacerbations Reduce mortality Prevent or minimize side effects What nonpharmacologic and pharmacologic interventions would you recommend? Pulmonary rehab Oxygen may be needed if SaO2 < 90% on room air and/or PaO2 < 60 mm Hg Pharmacologic regimen should include: Up-to-date influenza vaccination SABD PRN (beta-agonist or anticholinergic) LABD scheduled Inhaled glucocorticosteroids (if repeated exacerbations) |
|
|
What is treatment option that is worst case scenario in COPD?
|
Pulmectomy
|
|

|
|
|
|
Hallmark symptom of COPD?
|
Dyspnea
|
|
|
preventable and treatable disease characterized by progressive airflow limitation that is not fully reversible and abnormal inflammatory response of lung to noxious particles or gases
|
COPD
|
|
|
presence of cough and sputum production for at least 3 months in each of 2 consecutive years(not necessarily associated with airflow limitation).
|
Chronic Bronchitis
|
|
|
destruction of the alveoli; a pathological term used clinically but only describes one of several structural abnormalities present in pts with COPD.
|
Emphysema
|
|
|
List the common risk factors for developing COPD. Which one is the most commonly encountered?(4)
|
Tobacco smoke(most common)
Occupational dusts and chemicals Indoor air pollution Outdoor air pollution |
|
|
Describe the key indicators when a diagnosis of COPD is being considered? Over what age are these good indicators?(4)
|
Age over 40 with:
1. Dyspnea: progressive, worse with exercise, persistent(daily) 2. Chronic cough: intermittent, unproductive 3. Chronic sputum production: any pattern 4. History of exposure to risk factors |
|
|
Stage I -MILD
FEV1: FEV1/FVC: Presentation |
S1
FEV1: >80% FEV1/FVC: <70% Presentation: May be unaware of abnormal lung function |
|
|
Stage II -moderate
FEV1: FEV1/FVC: Presentation |
S2
FEV1: 50-80% FEV1/FVC: <70% Presentation: Often difficulty on expiration(this is where most pts seek help) |
|
|
Stage III-severe
FEV1: FEV1/FVC: Presentation: (3) |
S3
FEV1: 30-50% FEV1/FVC: <70% Presentation: More SOB, reduced exercise capacity, repeated exacerbations |
|
|
Stage IV Very severe
FEV1: FEV1/FVC: Presentation |
S4
FEV1: <30% FEV1/FVC: <70% Presentation: FEV1 <50% + Chronic Respiratory failure |
|
|
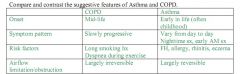
Though asthma can usually be distinguished from COPD, what symptoms makes them difficult to distinguish?
|
In some individuals with Chronic Respiratory symptoms and fixed airflow limitation it remains difficult to differentiate
|
|
|
What are the 5 A's for helping someone quit smoking?
|
Ask - document
Advise - Implore against Assess -are you ready to quit Assist - Quit plan Arrange - Schedule follow-up |
|
|
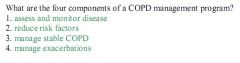
What are the general principles of managing stable COPD?(3)
|
-Determine disease severity
-Implement a stepwise treatment plan -Choose treatments |
|
|
At what stage of COPD would a LABD(long-acting bronchodilator be used)
|
SII
|
|
|
When would an ICS be added to COPD therapy. Under what conditions?
|
SIII. Repeated exacerbations
|
|
|
|
|
|
|
|
|
|
|

|

|
|

|

|
|
|

|
|

|

|
|
|
|

