![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
130 Cards in this Set
- Front
- Back
|
1. Which is not a real or possible physiological effect of positive pressure breathing?
a. increased intercranial pressure b. increased venous return c. decreased cardiac output d. decreased blood pressure |
b. increased venous return
|
|
|
2. When the sensitivity is adjusted to make the machine more sensitive; the patient can:
a. control inspiratory flow with less work b. the patient can determine the tidal volume more precisely c. the patient can breath spontaneously, but must apply more effort d. trigger a breath with less effort e. all of the above |
d. trigger a breath with less effort
|
|
|
3. During positive pressure breathing there is bulk movement of air into and out of the lungs. If we define P1 as pressure applied to the airway and P2 as alveolar pressure, which of the following is correct during inhalation?
a. P1>P2 b. P1<P2 c. Boyle’s Law causes P2 to increase while P2 decreases d. P1=P2 |
a. P1>P2
|
|
|
4. You are caring for a patient on a PB 840 in volume targeted ventilation on a rate of 8, a tidal volume of 550ml, and a peak flow of 40 L/M. You are asked to increase the rate. Which of the following would also occur as a result of this change?
a. The expiratory time will decrease b. The inspiratory time will increase c. The peak inspiratory pressure (PIP) will decrease d. The I:E ratio will stay the same |
a. The expiratory time will decrease
|
|
|
5. You are caring for a patient on a PB7200 in volume control ventilation on a rate of 8, a tidal volume of 500ml, and a peak flow of 60 L/M. You elect to increase the peak flow. Which of the following would also occur as a result of this change?
a. Peak Inspiratory pressure (PIP) will decrease b. Expiratory time will increase c. Tidal volume will increase d. Inspiratory time will increase |
b. Expiratory time will increase
|
|
|
6. You are caring for a patient on mechanical ventilation and you observe the following settings/parameters for that patient: set tidal volume = 650ml, SIMV mode on a set rate of 12, PEEP of 5 cmH2O and the plateau pressure is 24 cmH2O. What is this patient’s calculated airway resistance (assuming a constant flow)?
a. .5 cmH2O/L/s b. 3.75 cmH2O/L/s c. 10 cmH2O/L/S d. 16 cmH2O/L/s e. 12 cc/L/M |
d. 16 cmH2O/L/s
|
|
|
7. What effect can positive pressure ventilation have on antidiuretic hormone (ADH)?
a. it inhibits the action of ADH b. it enhances the action of ADH c. it has no effect on the action of ADH d. it stimulates the secretion of ADH e. it decreases the secretion of ADH |
d. it stimulates the secretion of ADH
|
|
|
8. A patient on the ventilator has the following settins; Set Vt = 900cc, rate=10 bpm, PEEP=5cmH2O, FIO2=70%. 20 BPM is the respiratory rate that you count, and the total minute ventilation that you measure is 14 L/M. Which of the following modes is the patient most likely in?
a. SIMV b. Pressure Support c. Control d. Assist control |
a. SIMV
|
|
|
9. What effect will pressure support have on the set machine breath in A/C mode?
a. as pressure support is increased the machine breath will increase b. pressure support can only effect the machine breath during pressure target ventilation c. pressure support will only support the machine breath that is triggered by the patient d. pressure support has no effect on machine breaths |
d. pressure support has no effect on machine breaths
|
|
|
10. You are caring for a patient on mechanical ventilation and you observe the following settings/parameters for that patient: set tidal volume = 450 ml, SIMV mode on a set rate of 8, PEEP of 3 cmH2O, FIO2 of .35 and a flowrate of 40 L/M. The patient’s PIP is 27 cmH2O and the plateau pressure is 24 cmH2O. What is the patient’s calculated airway resistance (assuming a constant flow).
a. 4.5 cmH2O/L/s b. 3.0cmH2O/L/s c. 10 cmH2O/L/s d. 16 cmH2O/L/s e. 12 cc/L./m |
a. 4.5 cmH2O/L/s
|
|
|
11. Which of the following will help prevent ventilator associate pneumonia (VAP)?
I. elevation of the bed 30-40 degrees II. active humidification without a heated wire III. frequent closed suction and circuit changes IV. oral care with chlorohexidine at least q4 a. I b. I, III c. II, III d. I, IV e. I, II, III, IV |
d. I, IV
|
|
|
12. What FIO2 is usually considering the threshold for the development of oxygen toxicity?
a. 90% b. 60% c. 30% d. FIO2 is not a factor; toxicity is likely at a PaO2 of 150mmHg |
b. 60%
|
|
|
14. If static compliance decreases and/or RAW increases, what happens to delivered Vt and PIP in volume targeted ventilation?
a. Vt and PIP will increase b. Vt will not change, PIP will increase c. Vt will decrease, PIP will not change d. Vt and PIP will decrease e. Vt will not change, PIP will decrease |
b. Vt will not change, PIP will increase
|
|
|
15. Which of the following is not true of volume targeted ventilation?
a. volume delivered stays the same despite changes in airway resistance or lung compliance b. inspiratory pressures will vary with increased RAW and/or decreased compliance c. flow will vary depending on inspiratory demand d. flow may not be synchronized with patient demand |
c. flow will vary depending on inspiratory demand
|
|
|
17. A patient on a ventilator has a peak pressure of 25cmH2O, a plateau pressure of 20 cmH2O measured with an inspiratory hold of 1 second. The baseline pressure is a PEEP of 5 cmH2O. The tidal volume delivered to the patient is 550ml. What is the static compliance?
a. 12L cmH2O b. 36.7 ml/cmH2O c. .027 cmH2O/cc d. 600 ml/sec e. 27.5 ml/cmH2O |
b. 36.7 ml/cmH2O
|
|
|
18. Which of the following are involved in a normal, spontaneous, negative pressure inspiration?
I. elevation of the diaphragm II. increased volume in the thorax III. Boyle’s law IV. decreased venous return to the right side of the heart a. I, II b. I, II, III c. II, III, IV d. II, III e. I, II, III, IV |
d. II, III
|
|
|
19. A patient mechanically ventilated with volume control (pre-set) positive pressure is set in the A/C mode. The patient’s lung compliance decreases; which of the following is true?
a. the tidal volume will decrease b. the tidal volume will remain the same, while the PIP increases c. only the spontaneous tidal volume will decrease d. the tidal volume will increase, while the PIP decreases |
b. the tidal volume will remain the same, while the PIP increases
|
|
|
20. You are caring for a patient on pressure control (pre-set) ventilation in A/C. the set Inspiratory Pressure is 20cmH2O and the PEEP is set at 10cmH2O. What will the PIP equal?
a. 10cmH2O b. 25 cmH2O c. 30 cmH2O d. the PIP will vary depending on patient effort, RAW, and lung compliance e. 800cc |
c. 30 cmH2O
|
|
|
21. A patient is set in volume targeted ventilation, control mode (sensitivity is locked out). What will happen when the patient tries to take a breath?
a. the patient will receive the set tidal volume at a faster rate determined by the patient b. the patient’s effort will not communicate to the machine; the set rate and machine breath will not change c. the patient will be able to breath spontaneously between maching breaths d. the patient can increase the set tidal volume but not the rate |
b. the patient’s effort will not communicate to the machine; the set rate and machine breath will not change
|
|
|
22. Which mode is most appropriate for gradually weaing the patient from the ventilator?
a. Control b. Assist/Contrl c. Pressure targeted assist/control d. SIMV |
d. SIMV
|
|
|
23. A patient on a ventilator has a peak pressure of 30 cmH2O, a plateau pressure of 20 cmH2O measured with an inspiratory hold of 1 second. The baseline pressure is zero (no PEEP). The tidal volume delivered to the patient is 600 cc. What is the static compliance?
a. 12 L cmH2O b. 30 cc/cmH2O c. .033 cmH2O/cc d. 600 cc/sec e. 20 cc/cmH2O |
b. 30 cc/cmH2O
|
|
|
24. During inspiration with normal spontaneous breathing:
a. A relative negative pressure is generated inside the thorax by decreasing the volume in the thorax b. A relative negative pressure is generated in the thorax which results in impeded venous return to the right side of the heart c. A relative positive pressure is generated in the thorax by the elastic recoil of the lugns d. A relative negative pressure is generated in the thorax by increasing the volume in the thorax e. A relative positive pressure is generated in the atmosphere by decreasing the volume of the atmosphere |
d. A relative negative pressure is generated in the thorax by increasing the volume in the thorax
|
|
|
25. Considering the new findings concerned VAP the cuff pressure should be set:
a. as low as possible while still providing a seal for mechanical ventilation b. high enough to hold the tub in proper position c. high enough to prevent microaspiration > than 35 cmH2O d. high enough to limit aspiration, at least 20 cmH2O |
d. high enough to limit aspiration, at least 20 cmH2O
|
|
|
26. You are caring for a patient on “typical” volume targeted (pre-set) ventilation (you directly set a tidal volume, a peak flow and a rate), who is on a rate of 8, a tidal volume of 750ml, and a peak flow of 50L/M. You are asked to decrease the set tidal volume to 600 ml. Which of the following would also occur as a result of this change?
a. Peak Inspiratory pressure (PIP) will increase b. Expiratory time will increase c. I:E ratio will remain the same d. Inspiratory time will increase |
b. Expiratory time will increase
|
|
|
27. You are assessing a ventilator patient and notice that the PIP pressure is about 15 cmH2O higher than it has been previously. The plateau pressure is also about 15 cmH2O higher than before. Where is the problem most likely to be?
a. In the ventilator tubing itself, the patient hasn’t changed b. In the alveoli, pleura or chest wall c. In the airways d. In the nasopharynx |
b. In the alveoli, pleura or chest wall
|
|
|
28. A patient on a ventilator has the following settings; Set Vt-900cc, set rate-10 bpm, PEEP-5cmH2O, FIO2-70%. 20 bpm is the respiratory rate that you count and the total minute ventilation that you measure is 14 L/M. Which of the following modes is the patient most likely in?
a. SIMV b. Pressure Support c. Control d. Assist Control |
a. SIMV
|
|
|
29. You are doing a routine ventilator check on a patient. You notice the PIP in increased about 10cmH2O since the last ventilator check. The plateau pressure hasn’t changed. You auscultate the lungs and hear coarse rhonchi bilaterally. What is the most likely interpretation of this information?
a. The patient’s static compliance has increased and the patient likely needs diruretics b. The patient’s Raw ha decreased, no further intervention is needed c. The patient’s static compliance has decreased and he needs a bronchodilator d. the patient’s Raw has increased and he needs suctioning |
d. the patient’s Raw has increased and he needs suctioning
|
|
|
30. The intrapleural pressure during normal negative pressure breathing is:
a. negative during inspiration but positive during exhalation b. positive during inspiration but negative during exhalation c. negative during inspiration and still negative during exhalation d. positive during inspiration and still positive during exhalation e. a little negative about the positive but positive about the negative |
c. negative during inspiration and still negative during exhalation
|
|
|
31. Which of the following is not true of volume targeted ventilation?
a. volume delivered stays the same despite changes in airway resistance or lung compliance b. inspiratory pressures will vary with increased Raw and/or decreased compliance c. flow will vary depending on inspiratory demand d. flow may not be synchronized with patient demand |
c. flow will vary depending on inspiratory demand
|
|
|
32. Which of the following are involved in a normal, spontaneous, negative pressure inspiration?
I. elevation of the diaphragm II. increased volume in the thorax III. Boyle’s law IV. decreased venous return to the right side of the heart a. I, II b. I, II, III c. II, III, IV d. II, III e. I, II, III, IV |
d. II, III
|
|
|
33. What lung capacity or volume is determined by the equilibrium between the elastic recoil of the lungs and the natural expansion tendencies of the thoracic cage?
a. TLC b. VC c. ERV d. FRC e. VT |
d. FRC
|
|
|
34. You are caring for a patient on mechanical ventilation and you observe the following settings/parameters for that patient: set tidal volume=450ml, SIMV mode on a set rate of 8m PEEP of 3 cmH2O, FIO2 of .35 and a flowrate of 40 L/M. The patient’s PIP is 27 cmH2O and the plateau pressure is 24 cmH2O. What is this patient’s calculated airway resistance (assuming a constant flow)?
a. 4.5 cmH2O/L/s b. 3.9 cmH2O/L/s c. 10 cmH2O/L/s d. 16 cmH2O/L/s e. 12 cc/L/M |
a. 4.5 cmH2O/L/s
|
|
|
35. You are called to help with a patient who is reported to have an increase WOB. You walk into the patient’s room and see a middle-aged woman slumped down in her chair. Her respiratory rate is 36 with shallow respirations. She is on a reservoir mask and an oximeter is showing a sat of 78. She does not respond to verbal stimulation; she simply stares ahead. Her nurse informs you that this is a new finding, that earlier she was awake, alert and cooperative. What is likely the best recommendation?
a. Take her off the mask and put her on a 2L/M nasal cannula b. Begin baggin her, alert the code team and prepare for intubation c. Sit her up in the chair better and listen to her lungs d. Tell the nurse that you think she “needs a neb” |
b. Begin baggin her, alert the code team and prepare for intubation
|
|
|
36. When we use the term “relative negative pressure” with respect to spontaneous breathing, we mean that the pressure is negative relative to what?
a. The pleural pressure b. The transtracheal pressure c. The atmospheric pressure d. The partial pressure of nitrogen in the lungs |
c. The atmospheric pressure
|
|
|
37. The physiological effects of positive pressure include which of the following?
I. increased airway pressure II. potential for increased lung volume III. mechanical bronchodilation IV. potential decrease in work of breathing V. manipulation of the I:E ratio a. I, II, III b. II, IV c. I, II, IV d. I, III, IV, V e. I, II, III, IV, V |
e. I, II, III, IV, V
|
|
|
38. When the sensitivity is adjusted to make the machine more sensitive; the patient can:
a. control inspiratory flow with less work b. the patient can determine the tidal volume more precisely c. the patient can breathe spontaneously, but must apply more effort d. trigger a breath with less effort e. all of the above |
d. trigger a breath with less effort
|
|
|
39. During a “vent check” you observe the following: the peak pressure has increased from 28cmH2O to 41cmH2O since the previous check approximately 2 hours ago but the plateau pressure has not changed. The patient has equal breath sounds bilaterally with rhonchi in all fields. What would you do next?
a. needle decompression of the chest b. set the high alarm lime to 55cmH2O c. suction the patient’s ET-Tube d. order a stat chest x-ray |
c. suction the patient’s ET-Tube
|
|
|
40. A patient in SIMV mode who is set on a Vt of 800cc, set rate of 4 bpm, PEEP 5cmH2O, PS of 15cmH2O, and an FIO2 of 40% takes a breath between breaths delivered from the machine. What type of breath did the patient take?
a. control b. assist c. supported d. spontaneous e. automode |
c. supported
|
|
|
41. A mechanically ventilated asthmatic patient has become more bronchospastic over several hours. Which of the following changes would you expect to see during that time?
I. decreasing PIP II. increasing PIP III. increasing plateau IV. decreasing plateau V. no change in plateau a. I, IV b. II, III c. I, V d. II, V |
d. II, V
|
|
|
42. When looking at a compliance curve (volume vs pressure) the pressure and volume beyond the upper inflection point represents (“beaking”):
a. deadspace b. tube compensation c. over distention d. alveolar recruitment |
c. over distention
|
|
|
43. Increasing the inspiratory pressure in pressure control ventilation (pressure targeted) when the patient’s compliance, resistance, and effort have not changed should:
a. increase the PEEP b. increase the delivered tidal volume c. decrease the flow d. decrease the delivered tidal volume e. decrease the set respiratory rate |
b. increase the delivered tidal volume
|
|
|
44. Which of the following is not an advantage of pressure support ventilation?
a. reduced work of breathing b. improved synchrony between ventilator and patient c. works well with heavily sedated or apneic patients d. tolerates leaks lending itself to face-mask ventilation and cuffless ETT |
c. works well with heavily sedated or apneic patients
|
|
|
45. With pressure support ventilation the flowrate is:
a. initially rapid then tapers down to maintain the set pressure b. initially slow to build pressure gradually up to peak then shuts off c. a constant square wave to insure a constant pressure d. a constant square wave to insure a present volume |
a. initially rapid then tapers down to maintain the set pressure
|
|
|
46. One benefit of a flow trigger besides decreasing inspiratory work is:
a. relatively slow rise time b. a lower PIP c. a constant delivered volume d. potential for leak compensation |
d. potential for leak compensation
|
|
|
47. The flow during exhalation does not return to baseline. Of the following choices, the best way to fix this problem would be to:
a. decrease expiratory time b. increase inspiratory time c. increase flowrate d. increase the rate |
c. increase flowrate
|
|
|
48. Given the following settings on the Servo 900: minute volume = 28L/M, master rate = 40 bpm, % inspiratory time = 50%. Calculate the inspiratory time.
a. 1.5 sec b. 0.75 sec c. 14 sec d. 0.5 sec e. none of the above |
b. 0.75 sec
|
|
|
49. Given the following settings on the Servo 900: minute volume = 28 L/M, master rate = 40 bpm, % inspiratory time = 50%. Calculate the tidal volume.
a. 1400 cc b. 800 cc c. 700 cc d. 600 cc e. none of the above |
c. 700 cc
|
|
|
50. A patient mechanically ventilated with volume targeted positive pressure is set in the A/C mode. The patient’s lung compliance decreases; which of the following is true.
a. the tidal volume will decrease b. the tidal volume will remain the same, while the PIP increases c. only the spontaneous tidal volume will decrease d. the tidal volume will increase, while the PIP decreases |
b. the tidal volume will remain the same, while the PIP increases
|
|
|
51. A mechanically ventilated adult patient in a volume targeted SIMV mode suddenly becomes dyspneic and tachycardic. The high pressure alarm sounds with every machine breath and the returned Vt is under 100cc for all breaths (machine or spontaneous). Blood pressure via an A-line increases to 165/100 from 120/80. When you attempt to suction you find you cannot pass the catheter the full length down the ETT. Which of the following is the most likely explanation for this problem?
a. the ETT has some type of obstruction (it is kinked or occluded) b. the patient has developed a significant tension pneumothorax c. the cuff of the ETT if deflated d. the patient is actually extubated e. there is a significant leak in the system |
a. the ETT has some type of obstruction (it is kinked or occluded)
|
|
|
52. A patient mechanically ventilated with pressure targeted type ventilation (you pre-set the inspiratory pressure) is set in the A/C mode. The patient’s airway resistance decreases; which of the following would you expect to see?
a. the tidal volume will decrease while the PIP remains the same b. the tidal volume will increase while the PIP remains the same c. the tidal volume will remain the same while the PIP increases d. the tidal volume will remain the same while the PIP decreases |
b. the tidal volume will increase while the PIP remains the same
|
|
|
53. A ventilator is connected to a lung simulator and a particular mode is selected. As the resistance and compliance of the simulator is changed, you notice the Vt remains constant but airway pressure changes. Which of the following mode description reflects this phenomenon?
a. pressure controlled A/C b. volume controlled A/C c. pressure support d. CPAP e. a spontaneous breath during SIMV |
b. volume controlled A/C
|
|
|
54. All of the following types of breaths are classified as mandatory machine breaths except:
a. the patient starts and stops the breath b. the patient starts the breath but the ventilator stops it c. the ventilator starts the breath but the patient stops it d. the ventilator starts and stops the breath |
a. the patient starts and stops the breath
|
|
|
55. You are called to the bedside of a ventilator patient with sudden severe respiratory distress, unilateral absence of BS, hypertympanic percussion note, tracheal deviation away from the effected side, significant hypotension, and a PIP that reaches the high pressure alarm with each breath. You should suggest/do the following:
a. turn up the pressure alarm on the ventilator to keep it from continually going off b. call for a chest x-ray c. get a blood gas d. call a physicial stat to needle the chest then place a chest tube |
d. call a physicial stat to needle the chest then place a chest tube
|
|
|
56. The limit variable:
a. start inspiration b. determines pressure, volume or flow c. starts exhalation d. determines baseline pressure |
b. determines pressure, volume or flow
|
|
|
57. In volume targeted ventilation as the patient’s compliance decreases:
a. the volume increases b. the pressure decreases c. the volume decreases d. the pressure increases |
d. the pressure increases
|
|
|
58. In volume targeted ventilation as the patient’s compliance improves:
a. the volume increases b. the pressure decreases c. the volume decreases d. the pressure increases |
b. the pressure decreases
|
|
|
59. IPAP – EPAP = ?
a. IPPB b. PAP c. PS d. PEEP e. BEEP |
c. PS
|
|
|
60. You are managing a patient on continuous BiPAP therapy with an IPAP of 12 cmH2O and an EPAP of 4cmH2O. The change in pressure (“delta P”) is equal to:
a. 4 cmH2O b. 8 cmH2O c. 12 cmH2O d. 16 cmH2O |
b. 8 cmH2O
|
|
|
61. What patient population in ventilatory failure would benefit from BiPAP in the hospital setting?
a. the patient who has just been extubated b. the patient who is refusing intubation c. the patient with a C-spine injury d. the patient with end state disease e. all of the above |
e. all of the above
|
|
|
62. Which is not a real or possible physiological effect of positive pressure breathing?
a. increased intercranial pressure b. increased venous return c. decreased cardiac output d. decreased blood pressure |
b. increased venous return
|
|
|
63. A ventilator (PB840, PB7200 or Servo i) is set for pressure targeted ventilation in A/C. The set Inspiratory Pressure is 20cmH2O, and the PEEP is set at 10cmH2O. What will the PIP equal?
a. 10cmH2O b. 20cmH2O c. 30cmH2O d. the PIP will vary depending on patient effort, Raw and lung compliance e. 800cc |
c. 30cmH2O
|
|
|
64. When you increase the inspiratory time % on the Servo 900C ventilator in volume targeted ventilation the flow will decrease.
a. True b. False |
a. True
|
|
|
65. When ventilating with a volume targeted machine breath an increase in the flow rate will:
I. increase PIP II. decrease inspiratory time III. increase inspiratory time IV. decrease PIP V. decrease expiratory time a. I, II b. I, II, V c. II, IV d. III, IV, V |
a. I, II
|
|
|
66. Which of the following is/are true a “control” machine breath in pressure targeted SIMV?
I. time triggered II. volume limited III. pressure limited IV. volume cycled (off) V. pressure cycled (off) VI. time cycled (off) a. I, II, IV b. III, V d. I, III, VI e. II, VI |
d. I, III, VI
|
|
|
67. The following are advantages of pressure support ventilation:
I. it provides a constant tidal volume II. potential reduced work of breathing III. inspiratory time will vary depending on the needs of the patient IV. improved synchrony between ventilator and patient V. works well with heavily sedated or apneic patients a. I, IV, V b. II, III, V c. I, V d. IV, V e. II, III, IV |
e. II, III, IV
|
|
|
68. IPPB used to be routinely used as the main form of hyperinflation therapy as prophylactic treatment for post-surgical atelectasis. Name the treatment modality most commonly used now instead of IPPB.
a. hand held nebulizer b. chest physical therapy c. BiPAP d. incentive spirometry e. bedside spirometry |
d. incentive spirometry
|
|
|
69. Massive hemoptysis of unknown origin, untreated pneumothroax or a pneumothorax with a nonfunctional chest tube, hypotension, vominting, recent MI, or active TB are contraindications for:
a. aerosol therapy b. oxygen therapy c. intubation d. IPPB |
d. IPPB
|
|
|
70. The following settings must be set on the ventilator when in Pressure Targeted Assist Control mode:
a. set tidal volume, rate, FIO2, PEEP, peak flow b. inspiratory pressure, inspiratory time, rate, FIO2, PEEP c. inspiratory pressure, FIO2, PEEP d. set tidal volume, inspiratory pressure, rate, FIO2, PEEP e. pressure support, rate, FIO2, PEEP, peak flow |
b. inspiratory pressure, inspiratory time, rate, FIO2, PEEP
|
|
|
71. You are caring for a patient on a Servo 900C in volume targeted A/C (literally volume control mode with the sensitivity on). As you increase the respiratory rate (master rate knob), which of the following would occur?
a. inspiratory time will be increased b. the PIP will increase c. the tidal volume will decrease d. flow rate will increase |
c. the tidal volume will decrease
|
|
|
72. Which is the correct normal phase change variables for pressure support in the following order: cycle on, limit, cycle off?
a. flow, pressure, flow b. pressure, volume, volume c. pressure, pressure, pressure d. volume, time, pressure e. flow, volume, time |
a. flow, pressure, flow
|
|
|
73. Evaluate the following statement: you observe two different patients on mechanical ventilation who both have the same I;E ratio, therefore they must both be on the same rate. This statement is:
a. true b. true only when pressure control is used c. false d. false except for SIMV in the Servo i |
c. false
|
|
|
74. If Raw stays the same and peak flow of the machine breath increases during volume controlled ventilation the most likely effect would be:
a. increase in PIP b. increase in plateau pressure c. increase in volume d. decrease in respiratory rate |
a. increase in PIP
|
|
|
75. Autopeep would most likely be made worse by:
a. increasing the flowrate b. decrease the rate c. increasing the inspiratory time d. decreasing the tidal volume |
c. increasing the inspiratory time
|
|
|
76. Which of the following is an absolute contraindication for IPPB therapy?
a. pneumothorax treated with a chest tube b. hypertension c. active TB d. massive hemoptysis of unknown origin |
d. massive hemoptysis of unknown origin
|
|
|
77. You are managing a patient on continuous BiPAP therapy with an IPAP of 8 cmH2O and an EPAP of 3 cmH2O. How much inspiratory support is the patient receiving?
a. a total of 11 cmH2O b. a total of 5 cmH2O c. a total of 8 cmH2O d. cannot be determined with a standard BiPAP machine |
b. a total of 5 cmH2O
|
|
|
80. Which of the following is NOT a desired effect of properly applied PEEP?
a. alveolar over distention b. increased PO2 c. increase in FRC which should improve compliance d. decrease in PCO2 |
a. alveolar over distention
|
|
|
What is the normal range of maximum inspiratory pressure, or MIP (also called negative inspiratory force, or NIF), generated by adults?
A. -80 to -100 cm H2O B. -50 to -80 cm H2O C. -30 to -50 cm H2O D. -20 to -30 cm H2O |
A. -80 to -100 cm H2O
|
|
|
Common bedside measures used to assess the adequacy of lung expansion include all of the following except:
A. VC B. respiratory rate C. VT D. VD/VT |
D. VD/VT
|
|
|
Which of the following are indications for BiPAP therapy?
i alveolar hypoventilation in end stage COPD ii patient who requires full ventilatory support iii moderate hypoxemia caused by atelectasis iv non-central or obstructive sleep apnea v Recent, massive heart attack A. iv B. all of the above C. i, v D. i, iii, iv E. i, ii, iv, v |
D. i, iii, iv
|
|
|
Which of the following tracheostomy tubes uses a high pressure low volume cuff.
A. Shilley dual cannula B. Portex fenestrated C. Jackson metal tube D. Bivona tight to the shaft E. none of the above |
D. Bivona tight to the shaft
|
|
|
You are evaluating an average sized, adult patient in the ICU with a pulmonary catheter in place who has the following signs: PaO2 is 76 mm Hg Cardiac Output of 5.3 L/M PvO2 is 32 mm Hg Based only on the above information, what conclusions can be drawn regarding his Oxygen consumption?
A. it will be below normal B. It will be normal C. It will be above normal D. It can't be determined |
C. It will be above normal
|
|
|
A C(a-v)O2 content of 8 vol%, would be associated with:
A. Polycythemia B. Decreased Cardiac Output C. Hypothermia D. Decreased Affinity of Oxygen to Hb E. Hypercarbia |
B. Decreased Cardiac Output
|
|
|
All of the following indicate that an adult patient is ready to be weaned from ventilatory support except:
A. VC = 1.9 L B. spontaneous rate of 32/min C. shunt= 8% D. MIP = -45 cm H2O |
B. spontaneous rate of 32/min
|
|
|
What happens to the P(A?a)O2 with mismatch and shunt?
A. increases with mismatch and decreases with shunt B. decreases with both mismatch and shunt C. increases with both mismatch and shunt D. it does not change |
C. increases with both mismatch and shunt
|
|
|
The amount of oxygen dissolved in blood plasma represents the PO2. Which of the following is true?
i the amount of hemoglobin saturated with oxygen is dependent on the PO2 ii the PO2 represents a small amount of the oxygen content in the blood iii the actual content of oxygen in the blood is a combination of the oxygen bound to hemoglobin and oxygen dissolved in the blood iv the amount of oxygen dissolved in the blood represents the majority of oxygen content A. i B. i, ii, iii C. i, iii,iv D. iv E. none of the above |
B. i, ii, iii
|
|
|
Which of the following best describes the difference between mismatch and shunt when supplemental oxygen is administered?
A. Both will respond equally well. B. mismatch will respond well but shunt will not. C. mismatch will not respond but shunt will respond well. D. Neither will respond to the administration of supplemental oxygen. |
B. mismatch will respond well but shunt will not.
|
|
|
Which of the following statements are true?
i IPAP is equivalent to PEEP ii the single hose design of the BiPAP circuit could allow rebreathing of CO2 iii EPAP + IPAP = PSV iv the BiPAP is designed to increase auto PEEP A. ii B. all of the above C. I, iii D. ii, iii E. none of the above |
A. ii
|
|
|
What is the normal P(A?a)O2 range while breathing room air?
A. 25 mm Hg to 50 mm Hg B. 10 mm Hg to 25 mm Hg C. greater than 25 mm Hg D. less than 10 mm Hg |
B. 10 mm Hg to 25 mm Hg
|
|
|
Nasal pillows used to apply CPAP directly into the nostrils will most likely:
A. allow you to use less pressure B. alleviate the need for humidity C. prevent nasal collapse D. prevent gastric inflation |
C. prevent nasal collapse
|
|
|
A Shiley and a Portex tracheostomy tube with the same inside diameter are designed to also be the same length.
False True |
False
|
|
|
You are managing a patient on continuous BiPAP therapy with an IPAP of 18 cmH20 and an EPAP of 5 cm H20. The patient's respiratory rate is 16 bpm and regular. An ABG is drawn with the following results: pH 7.52 PC02 29 P02 88 HC03 24 Which of the following choices is the best recommendation to correct the problem?
A. increase the IPAP B. decrease the IPAP C. increase the EPAP D. decrease the EPAP E. no changes necessary, this is a reasonable ABG |
B. decrease the IPAP
|
|
|
A post-op coronary bypass patient is extubated after 6 hours of mechanical ventilation. ABGs obtained 1 hour after extubation reveal the following; pH = 7.24 PCO2=55 mmHg PO2=55 mmHg HCO3 =24 mEq/L on a 40% aerosol mask. The patient's respiratory rate = 40 bpm with noticeable use of accessory muscles. Breath sounds are clear but decreased at the bases. What is the best single therapeutic modality you would use to treat this patient from the following list.
A. no therapy is needed, this is the normal clinical course for this scenario B. increase O2 to 60% C. BiPAP therapy with supplemental O2 D. instruct the patient to do incentive spirometry Q1 hour |
C. BiPAP therapy with supplemental O2
|
|
|
All of the following indicate that an adult patient is ready to be weaned from ventilatory support except:
A. PAO2 - PaO2 = 430 on 100% O2 B. VD/VT = 0.55 C. MIP = -33 cm H2O D. PO2 = 76 mm Hg on 40% O2 |
A. PAO2 - PaO2 = 430 on 100% O2
|
|
|
How is IPAP triggered on by the patient?
A. the machine senses a drop in pressure in the tubing B. the machine works by a timing mechanism C. the machine senses an increase in flow above the baseline leak D. the machine senses upward movement of the diaphragm |
C. the machine senses an increase in flow above the baseline leak
|
|
|
The physiological effects of positive pressure include which of the following:
i increased airway pressure ii potential for increased lung volume iii mechanical bronchodilation iv potential decrease in work of breathing v manipulation of the I:E ratio A. i, ii, iii B. ii, iv C. i, ii, iv D. i, iii, iv, v E. all of the above |
E. all of the above
|
|
|
A patient with a tracheostomy tube needs the passey-muir valve placed as part of the patient's rehabilitation and weaning off the ventilator. The patient is on 28% oxygen while on the vent. After you remove the vent tubing from the trach, deflate the cuff, and place the Passey-muir valve; what is the best way to oxygenate this patient?
A. place the patient on a cannula at 2 L/M B. place the patient on a ventimask over the mouth and nose at 28% C. place the patient on a 28% aerosol trach mask D. just let the patient breath room air, since they will require less oxygen off the ventilator |
C. place the patient on a 28% aerosol trach mask
|
|
|
A patient you are caring for has a pulmonary artery catheter in place. The catheter has an oximeter built into it enabling the measurement of saturation of Oxygen. The saturation is reading at 75%. Assuming his oxyhemoblobin dissociation curve is not shifted, his PvO2 should be about:
A. 30 mm Hg B. 40 mm Hg C. 60 mm Hg D. 75 mm Hg E. 90 mm Hg |
B. 40 mm Hg
|
|
|
You are assessing a patient who is breathing fast (respiratory rate of 29) and shallow (tidal volumes are clearly well below normal for spontaneous breathing). This is an acute process; the nurse reports that the patient just starting breathing like this only a couple of hours ago. Which of the following choices is mostly likely to be true?
A. The patient's hemoglobin has a high affinity for oxygen B. The patient's pH is high C. The patient's oxyhemoglobin dissociation curve is shifted to the left D. The patient's oxyhemoglobin dissociation curve is shifted to the right. |
D. The patient's oxyhemoglobin dissociation curve is shifted to the right.
|
|
|
Which of the following is the cardinal sign of increased work of breathing?
A. hyperventilation B. retractions C. bradycardia D. tachypnea |
D. tachypnea
|
|
|
You are caring for a patient who is a new post-op CABG patient on mechanical ventilation. She has returned from the operating room hypothermic (35.3 °C). Assuming all her other vital signs and labs are within normal range, how would you expect her hemoglobin's affinity for Oxygen to be affected?
A. It would be higher than normal B. it would be lower than normal C. It would not be affected at all D. It would fluctuate widely |
A. It would be higher than normal
|
|
|
If you were to apply an above ambient pressure to the airway, which caused a bulk movement of gas into the lungs, you are:
A. applying positive pressure ventilation B. breathing normally C. performing a pulmonary function test D. playing the trombone |
A. applying positive pressure ventilation
|
|
|
What is the normal range for PaO2/FIO2?
A. 350 to 450 B. 250 to 350 C. 150 to 250 D. 75 to 150 |
B. 250 to 350
|
|
|
What is the main requirement of a noninvasive ventilator?
A. leak compensation B. a guaranteed tidal volume C. a patient who requires full mechanical support D. b and c E. none of the above is a requirement of noninvasive ventilation |
A. leak compensation
|
|
|
Which of the following is the best sequence for transitioning the patient from mechanical ventilation to breathing spontaneously through the upper airway.with a tracheostomy tube designed for this purpose.
A. deflate the cuff, suction down the tube and oropharynx , cap the trach, apply O2 to the upper airway B. suction down the tube and oropharynx, remove the inner cannula, cap the tube, apply O2 to the upper airway C. apply O2 to the upper airway, remove the inner cannula, suction down the tube and oropharynx, cap the trach D. suction down the tube and oropharynx, deflate the cuff, suction down the tube, remove the inner cannula, cap the tube, apply O2 to the upper airway E. deflate the cuff, remove the inner cannula, suction down the tube and oropharynx, apply O2 to the upper airway |
D. suction down the tube and oropharynx, deflate the cuff, suction down the tube, remove the inner cannula, cap the tube, apply O2 to the upper airway
|
|
|
Which of the following is the most important factor in blood oxygen content?
A. P02 B. Respiratory rate C. Saturation D. Hemoglobin E. c. and d. |
E. c. and d.
|
|
|
Which is not a real or possible physiological effect of positive pressure breathing
A. increased intercranial pressure B. increased venous return C. decreased cardiac output D. decreased blood pressure |
B. increased venous return
|
|
|
When is ventilator dependence likely to occur?
I. when ventilatory capacity exceeds demand II. when arterial hypoxemia is present III. when the patient is malnourished. IV. when the cardiovascular system is unstable A. II and IV B. I, II, and III C. III and IV D. II, III, and IV |
D. II, III, and IV
|
|
|
Regarding the use of foam-cuffed airways, which of the following is false?
A. they are found only on tracheostomy tubes B. normally air should not be added to the cuff C. they serve the same function as a regular air-filled cuff D. when extubating, one can simply cut the pilot line instead of deflating the cuff |
D. when extubating, one can simply cut the pilot line instead of deflating the cuff
|
|
|
You are asked to assess a post-operative patient who has had abdominal surgery. The patient is alert, cooperative, and has mild atelectasis, breath sounds are decreased at the bases. His VC is 1200cc or 18cc/Kg ideal body weight. He is coughing adequately. The best recommendation would be:
A. IPPB treatments Q4 hours B. Start I.S. (incentive spirometry), Q1 hour to Q2 hours while awake 100% C. check patient's NIF (negative inspiratory force), Q shift D. continuous BiPAP therapy E. Albuterol nebs Q4 hours |
B. Start I.S. (incentive spirometry), Q1 hour to Q2 hours while awake
|
|
|
Hypoxemia can be caused by which of the following?
I diffusion impairment II alveolar hypoventilation III mismatch IV intrapulmonary shunting A. I, II, and III B. I, III, and IV C. I, II, III, and IV D. II, III, and IV |
A. obstructive sleep apnea
|
|
|
Which of the following patients has the most serious problem with the adequacy of oxygenation? Answers are in FIO2 PaO2 order
A. 0.7 90 B. 0.4 95 C. 1.0 85 D. 0.28 65 |
C. 1.0 85
|
|
|
What is the disadvantage of a pressure preset volume variable positive pressure ventilator?
A. Inconsistent ventilation B. Pressure is never excessive in the airways C. More responsive to airway physiology D. Greater uniform distribution of ventilation |
A. Inconsistent ventilation
|
|
|
What patient population in ventilatory failure would benefit from BIPAP in the hospital setting?
A. the patient who has just been extubated B. the patient who is refusing intubation C. the patient with a C-spine injury D. patient with end stage disease E. all of the above |
E. all of the above
|
|
|
A patient with a 10-year history of chronic bronchitis and an acute viral pneumonia exhibits the following blood gas results breathing room air: pH = 7.22; PCO2 = 67; HCO3? = 26; PO2 = 60. Which of the following best describes this patient's condition?
A. chronic hypoxemic respiratory failure B. acute hypercapnic respiratory failure C. chronic hypercapnic respiratory failure D. acute hypoxemic respiratory failure |
B. acute hypercapnic respiratory failure
|
|
|
A diagnosis of respiratory failure can be made if which of the following are present?
I. PaO2 55 mm Hg, FIO2 0.21, Pb 760 mm Hg II. PaCO2 57mmHg, FIO2 0.21, PB 760 mmHg III. P(A-a)O2 45mmHg, FIO2 1.0, Pb 760mmHg IV. PaO2/FIO2 400, PB 750mmHg A. I and II B. I, III, and IV C. III and IV D. I, II, III, and IV |
A. I and II
|
|
|
Hypoxemia can be caused by which of the following?
I. Diffusion impairment II. Alveolar hypoventilation III. V/Q mismatch IV. Intrapulmonary shunting A. I, II, and III B. I, III, and IV C. I, II, III, and IV D. II, III, and IV |
C. I, II, III, and IV
|
|
|
You are managing a patient on continuous BiPAP therapy with an IPAP of 8 cm H2O and an EPAP of 3 cm H2O. The patient's respiratory rate is 28 bpm and regular. An ABG is drawn with the following results:
pH 7.43 pCO2 39 pO2 51 HCO3 24 Which of the following choices is the best recommendation to correct the problem? A. increase the IPAP only B. increase the IPAP...and increase the EPAP by the same amount C. increase the EPAP only D. decrease the IPAP...and decrease the EPAP by the same amount |
B. increase the IPAP...and increase the EPAP by the same amount
|
|
|
Which is the correct phase change variables for the BiPAP ventilator in spontaneous mode in the following order: cycle on, limit, cycle off?
A. flow, pressure, flow B. pressure, volume, volume C. pressure, pressure, pressure D. Volume, time, pressure E. Flow, volume, time |
A. flow, pressure, flow
|
|
|
You are managing a patient on continuous BiPAP therapy with an IPAP of 12 cm H2O and an EPAP of 4 cm H2O. The change in pressure (delta P) is equal to:
A. 4 cm H2O B. 8 cm H2O C. 12 cm H2O D. 16 cm H2O |
B. 8 cm H2O
|
|
|
A 62 kg patient with a history of unrestrained ejection from a motor vehicle on mechanical ventilation is under your care. You get the following ABG:
pH: 7.24 pACO2: 57mmHG pAO2: 77mmHg HCO3: 25 meq SaO2 98% On these ventilator settings: Volume targeted/SIMV Rate 16 Set VT 300ml PEEP of 5 cm H2O FIO2 of .40 PS 5 cm H2O Total rate of 16 Based on this clinical information, what ventilator change would most likely be the best choice? A. Increase the rate B. Increase the VT C. Decrease the rate and increase the PS D. decrease the VT E. Increase the FIO2 |
B. Increase the VT
|
|
|
If cardiac output decreases, which of the following will change the most?
A. PAO2 B. PaO2 C. P (A-a) O2 D. Pvo2 |
D. Pvo2
|
|
|
You are assessing a patient who has a history of anxiety disorder and has been hyperventilation for several hours. Assuming she has normal lung function (no pulmonary pathophysiological problems), which of the following is likely to be true?
A. She is acidotic B. Her p50 is less than 27 mm Hg C. She is hypoxemic D. Her hemoglobin has an increased affinity for oxygen |
D. Her hemoglobin has an increased affinity for oxygen
|
|
|
Which of the following indicate severely impaired oxygenated requiring high FIO2's and positive end- expiratory pressure?
I. PAO2-PaO2 greater than 350mmHg on 100% O2 II. VC less than 10 ml/kg III. PaO2/FIO2 less than 200 A. I and II B. I and III C. II and III D. I, II, and III |
D. I, II, and III
|
|
|
Strategies to reduce auto-peep in mechanically ventilated patients with obstructive lung disease include all of the following except which one?
A. Use high inspiratory flows (60-100L/min) B. Apply extrinsic PEEP C. Use low VT values (8-10 ml/Kg) D. Use high RR (greater than 25) |
D. Use high RR (greater than 25)
|
|
|
All of the following oxygenation measures support a patient's readiness to wean except:
A. PaO2/PAO2 = 0.45 B. PaO2/FIO2= 110 C. PAO2-PaO2 = 240mmHG D. Physiologic Shunt (Qs/Qt) = 12% |
B. PaO2/FIO2= 110
|
|
|
All of the following indicate that an adult patient is ready to be weaned from ventilatory support except:
A. PAO2-PaO2= 430 on 100% O2 B. VD/VT= 0.55 C. MIP= -33 cm H2O D. PO2= 76 mmHG on 40% O2 |
A. PAO2-PaO2= 430 on 100% O2
|
|
13. You are working in the ICU and are doing a ventilator check on your patient who is in SIMV mode with pressure support. The total respiratory rate is greater than the set respiratory rate. Which of the following graphics would be displayed?
a. 1 b. 2 c. 3 d. 4 |
B. 2
|
|
16. You are working in the medical ICU and one of your patients on mechanical ventilation has had increasing peak inspiratory pressures over the course of the last several hours. You go back over her chart and notice the trend graphed out below
What is happening? a. RAW is increasing b. static compliance is increasing c. the patient is beginning to assist the machine d. the patient’s support tidal volume is getting larger e. static compliance is decreasing |
e. static compliance is decreasing
|
|
78. A ventilator patient seems progressively short of breath, SpO2 is trending down and total respiratory rate is increasing. You notice the following on the volume/time waveform
What is the problem and what should you do now? a. air leak in the system systematically find and fix the leak b. auto-PEEP is present, adjust the inspiratory or expiratory time c. the sensitivity is set too low, adjust the sensitivity to allow the patient to trigger the breath with less work d. the pause has been left on after a compliance check, remove the plateau e. the graphic looks normal, the reason for the SOB is not revealed by the above graphic |
a. air leak in the system systematically find and fix the leak
|
|
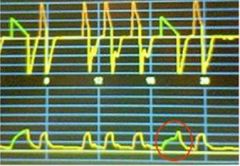
79. What does the circled waveform represent?
a. a cough b. a pressure supported breath c. a leak d. an example of flow starvation; the patient needed more flow than the set machine breath could provide e. a plateau |
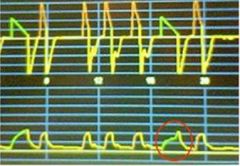
e. a plateau
|

