![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
411 Cards in this Set
- Front
- Back
|
Because a pediatric pt. may be less cooperative, what parts of the exam should be completed last?
|
distressing portions, so that crying and yelling doesn't happen until the end
|
|
|
If an infant is alert with open eyes while history is being taken, the opportunity should be taken to check what?
|
the red reflexes while it is available
|
|
|
Infancy (birth to 1 year)
What is the first thing that should be done in order to take the infants history? |
to take a history from the parent
|
|
|
Infancy (birth to 1 year)
When taking the history from the parent, what should it include? (3) |
mother's obstetrical history, including amount and type of prenatal care
where the baby was delivered any complications that occurred |
|
|
Infancy (birth to 1 year)
Where should the baby be examined? |
on the examination table or in the mother's arms
BE FLEXIBLE! :-) *If the child is able to sit and wants to sit, then begin with the child sitting. |
|
|
Infancy (birth to 1 year)
How should the baby be examined? (clothing wise) |
thoroughly with clothes off, but this may be done is a sequential manner
if the infant is undressed to the diaper, be aware of the office temperature, and offer a blanket if necessary |
|
|
Infancy (birth to 1 year)
At what age do infants start to be anxious about the exam? |
7 to 8 months of age
|
|
|
Infancy (birth to 1 year)
Careful observation should be made first. This can be done during what? |
while you are taking the history
|
|
|
Infancy (birth to 1 year)
What things should be noted while observing an infant? (3) |
"funny looking" features
parent-child interaction overall appearance of health |
|
|
Infancy (birth to 1 year)
When the infant is not crying, what should the dr. take the opportunity to do? |
auscultate the heart and lungs
*it is best to do this part of the exam early |
|
|
Infancy (birth to 1 year)
If the infant will not stop crying, what should the dr. do to examine the heart and the lungs? |
attempt to listen to the heart between cries
listen too the lungs during the inspiratory part of the cry |
|
|
Infancy (birth to 1 year)
What are the 5 ESSENTIAL parts o the infant examination? |
heart
eyes pulses hips genitourinary |
|
|
Infancy (birth to 1 year)
Conclude the exam with the parts that are more distressing to the infant. What falls into this category? (3) |
ears
throat hips |
|
|
Toddler (1year - 2 1/2 years)
What should the dr. do the first thing when he walks into the room? Second? |
speak to the child first. Call him by his first name.
*children usually respond positively to adults whom they sense like them. Then, take the history from the parent |
|
|
Toddler (1year - 2 1/2 years)
Where should the examination start? |
with the child on the mother's lap
|
|
|
Toddler (1year - 2 1/2 years)
What can you do to make the examination as fun as possible? |
offer to let them see your medical equipment (tongue blades, flashlight, etc.)
|
|
|
Toddler (1year - 2 1/2 years)
Should you ever ask permission to the child to do something? |
NO! you will be sorry!
Say: "Open your mouth, Brittany." Don't Say: "Will you please open your mouth, Brittany?" |
|
|
Toddler (1year - 2 1/2 years)
What 3 things should be examined first? |
heart
lungs abdomen |
|
|
Toddler (1year - 2 1/2 years)
What two things should be examined last? |
ears
throat |
|
|
Toddler (1year - 2 1/2 years)
What should happen if a child is resistant? |
it is important they be restrained so they will not be hurt during the exam
|
|
|
Toddler (1year - 2 1/2 years)
What are essential component of the exam in this age group? (3) |
heart
eyes (for strabismus) genitourinary (for undescended testicles, imperforate hymen) |
|
|
Toddler (1year - 2 1/2 years)
When examining the eyes it is important to look for what? (1) |
strabismus
|
|
|
Toddler (1year - 2 1/2 years)
When examining the genitourinary, it is important to look for what? (2) |
undescended testicles
imperforate hymen |
|
|
Toddler (1year - 2 1/2 years)
What anticipatory guidance should be given to this age group? (3) |
diet
development **Safety** |
|
|
Toddler (1year - 2 1/2 years)
What type of screening should be taken at age 1 and age 2? |
lead screening
|
|
|
Older toddler and school-aged child (2 1/2 years to teenager)
What should the dr. do the first thing when he enters into the room? |
Recognize the child by name when you enter the room.
Obtain part of the history from child finish by take a history from the parent |
|
|
Older toddler and school-aged child (2 1/2 years to teenager)
When beginning the exam, what should the dr. do to make the child feel more comfortable? |
explain to the child what you are doing
allow them to listen with the stethoscope, look through the otoscope, etc. |
|
|
Older toddler and school-aged child (2 1/2 years to teenager)
What two things need to be addressed? |
school performance
safety |
|
|
Older toddler and school-aged child (2 1/2 years to teenager)
What are important parts of the school aged well visit? (4) |
screening for hearing, vision, anemia, and scoliosis
|
|
|
Teenager
How should the history be taken? |
Begin by take the history from the parent and teenager together, talking mostly to the teenager, but making sure to get a complete history from the parent. Establish that you are the teen's doctor, not the parent's doctor.
Ask the parent to leave the room while you finish taking the history from the teenager alone. |
|
|
Teenager
What should be discussed when the dr. talks to the teenager alone once the parent has left? (8) |
Discuss the limits for confidentiality and under what conditions information obtained will be discussed with the parent.
Obtain the SOCIAL, SCHOOL, SEXUAL, and DRUG histories. Obtain descriptions of parent, sibling, and peer relationships. *Don't assume anything* Be nonjudgmental, but provide encouragement for good choices. Ask the patient whether or not the parent should be invited back into the room during the physical exam. |
|
|
Teenager
It is important for the doctor to address the teen's concern and the parents. T or F :-) easy one!T |
true
a parent may be concerned regarding behavior issues, but a teen may be concerned regarding their acne. |
|
|
Teenager
Who should be present during sensitive parts of the examination? |
chaperone
|
|
|
Teenager
What is it important to screen for at this age? |
Males: testicular examination is important because of the risk of testicular cancer
In sexually active females, a pelvic exam and Pap smear should be done Breast self examination should be taught. |
|
|
Teenager
Is a breast examination necessary? |
no
breast self examination should be taught. It is not always necessary to do a breast examination, as cancer is very rare in this age group. Be aware of patients discomfort- best if male examines male, etc. |
|
|
What age group is it important to look at Tanner staging?
|
all children
esp. preteen and teen age groups |
|
|
Tanner staging can usually be accomplished with a what?
|
quick look
|
|
|
Tanner staging for breast development.
|
1- prepubertal
2- breast bud 3- increased size of breast tissue 4- separation of areola above breast tissue 5- adult breast |
|
|
Tanner staging for pubic hair development.
|
1- prepubertal
2- light, straight, sparse hair 3- darker, coarser hair 4- adult type pubic hair, limited to pubic area 5- adult pubic hair, with extension onto medial thighs, and in males up towards the umbilicus |
|
|
Tanner staging for male genitourinary development.
|
1- prepubertal child
2- enlargement of testes and scrotum 3- increase in penile length and testes growth 4- increased penile breadth and length, glans development, darkening of scrotal skin, larger testes 5- adult |
|
|
Peak height velocity for girls occurs in what Tanner stages?
|
2-3
|
|
|
Menarche occurs in Tanner stage__?
|
4
|
|
|
Peak height velocity for boys occurs after what Tanner stage?
|
after Tanner stage 4
|
|
|
In the U.S. the average age for menarche is___?
|
12
|
|
|
The average age for onset of puberty in girls (usually breast development) is ?
|
9-10
|
|
|
The average age for onset of puberty in boys in the U.S. is?
|
11-12
|
|
|
Puberty is considered "precocious" in the U.S when it occurs before age:
___ in Caucasian girls ___ in African American girls ___ in boys |
7 in Caucasian girls
6 in African American girls 9 in boys |
|
|
Puberty is considered delayed if there are no changes by age _____ in girls.
However, 1-2% of normal girls will not have experienced menarche by age____. |
14
16 |
|
|
What is adrenarche?
|
onset of pubic hair development
|
|
|
What is adrenarche due to?
|
adrenal androgen production
|
|
|
In premature adrenarche levels of ____?______ may be measured.
|
dehydroepiandrostenedione-sulfate
|
|
|
Pelvic exams are indicated only when.....? (3)
|
there is a history of sexual activity
when the child is 18 years or older when the child reports gynecologic problems *should be done only by the most experienced physician seeing the pt. |
|
|
When are rectal exams done?
|
They are NOT done routinely on any pediatric pt. (risk of rectal carcinoma is low)
Should be performed on all pts. with a chief complaint suggestive of gastrointestinal disease, such as constipation or abdominal pain *should be performed by the most experienced physician seeing the pt. |
|
|
What 8 things should the dr. look for when he gives a general inspection of a child?
|

1. characteristics of the child's cry (strong, weak, absent, high pitched)
2. is the child alert aware of his environment or is the child listless 3. observe the child's interaction with the parent, look for unusual activity 4. determine the state of nutrition (obese? undernourished?) 5. any abnormalities in the child's feature? - compare with parent present ("FLK" funny looking kid= may have a syndrome or may have inherited features) 6. look for Down's syndrome symptoms 7. look for fetal alcohol syndrome symptoms 8. observe movements of child to make sure they are symmetrical |
|
|
What are the characteristics of Down's syndrome that are important for a dr. to look for when performing a general inspection?
|
facial features with upward slanting palpebral fissures, epicanthal folds, flat nasal bridge
Brushfield spots, simian crease, wide space between first and second toes, short fifth fingers, small ears, and a flat occiput |
|
|
What are the characteristics of fetal alcohol syndrome that are important for a dr. to look for when performing a general inspection? (physical characteristics, things it is associated with, IQ?)
|
narrow and widespread eyes, long single philtrum, thin upper lip, short nose and hypoplasia of the nails and distal phalanges
associated with microcephaly, growth deficiency, and congenital heart disease IQ is usually 50 to 80 these children are usually hyperactive and have problems with fine motor skills |
|
|
Major evidence of fetal alcohol syndrome is observed in ___% to ___% of offspring of chronic severe alcoholics. What is the safe level of alcohol intake in pregnancy?
|
30- 50%
there is NO safe level |
|
|
When observing a child's movements, any persistent positioning should be taken note of. This could be indicative of what?
|
of a problem such as a fracture, hip dislocation, or neurological abnormality
|
|
|
Which fluctuate more: body temperatures of children or adults? by how many degrees?
|
children, normally higher by 1 degree F
|
|
|
What is diurnal variation?
|
children 2 to 6 years old may have significant diurnal variation in temp., with a pm temp as much as 1.6 degrees F higher than in the morning.
|
|
|
Do infants have (less or more) diurnal variation in temperature than children?
|
less
|
|
|
What may infants temperature be affected by?
|
environmental factors (heavily wrapped infant may have a higher temp and then when unwrapped it will go down)
|
|
|
How may temperature be measured?
|
rectal
axillary tympanic other oral measurements |
|
|
Oral temperatures are not usually taken until after what age?
|
7
|
|
|
What is the gold standard way of taking a temperature?
|
rectal temperature...but it is used infrequently
|
|
|
Axillary temperatures are usually 1 degree (higher or lower??) than oral, while rectal temperatures are usually 1 degree (higher or lower??) than oral measurement.
|
Axillary temperatures are usually 1 degree LOWER than oral, while rectal temperatures are usually 1 degree HIGHER than oral measurement.
|
|
|
Which way of taking a temperature may be unreliable?
|
axillary temp.
|
|
|
which way of taking a temperature is accurate if done correctly?
|

tympanic
|
|
|
What is the definition of a fever in a newborn?
|
greater than 37.8 degree Celsius
|
|
|
Can temperatures as high as 38.4 be normal in newborns?
|
NO...but that is normal in older children
|
|
|
When should temperatures be take?
|
when the child is quiet, not after exercise
|
|
|
How does the heart rate of a child differ from that of an adult?
|
it is faster and fluctuates more in a child
as the child ages the heart rate decreases |
|
|
What is the average heart rate at birth?
What does it drop to by one year of age? |
140/min
drops to 110/min. by year one |
|
|
At what age does the average heat rate decrease below 110/min.?
|
6 years old
|
|
|
How can the heart rate be obtained?
|
by palpating the femoral or brachial arteries or by auscultating the heart directly
|
|
|
What are the characteristics of sinus tach?
|
usually begins gradually
heart rate may vary by 10 to 15 beats per min. |
|
|
What are the characteristics of SVT?
|
heart rate starts and stops abruptly
the rate is usually greater than 200 |
|
|
What may SVT present with in infants? (3)
|
irritability
decreased feeding increased respirations |
|
|
What is a normal and common finding in a children over 3 years of age whose pulse rate increases during inspiration and decreases during expiration?
|
sinus arrhythmia
|
|
|
How does the respiratory rate differ from that of a child to that of an adult?
What are the respiratory rate ranges for the following: newborn, infancy, 6 yrs? At what age does it decrease to adult levels? |
child- it is more variable and rapid
respiratory rate ranges: 30-80/ min = newborn 20-60 / min= infancy 16-25/min= 6 yrs decreases to adult levels by 15 years of age. |
|
|
How long should the respiratory rate be measured in young children in order to be accurately determined?
|
one minute
|
|
|
Because diaphragmatic breathing is predominant in small children, the respiratory rate is best measured by observing what?
|
abdominal (not chest) excursions
|
|
|
T or F
in infancy, respirations can be irregular, intermittent, and variable in rate and depth. |
true
|
|
|
What are normal (but scary to the parents) respiration patterns that can occur while an infant is sleeping?
|
periodic breathing, with brief respiratory pauses of up to 10 seconds and no color change
|
|
|
What is apnea?
|
a respiratory pause of over 20 seconds, or one that is associated with cyanosis, pallor, or change in heart rate
|
|
|
A respiratory rate greater than ____ in infants less than 2 months old, greater than ____ in 2-12 month olds, and greater than ___ in toddlers is probably abnormal.
|
A respiratory rate greater than __60__ in infants less than 2 months old, greater than __50__ in 2-12 month olds, and greater than _40__ in toddlers is probably abnormal.
|
|
|
At what age should the blood pressure of a child be measured?
How is blood pressure measured in younger children and infants? |
every child over 3 years of age
younger children and infants usually tested using Doppler flow techniques |
|
|
How should the blood pressure be taken in a child?
|
it must be measured with a cuff that is wide enough to cover 75% of the diameter of the upper arm, but not so big that the cuff overlies the antecubital fossa, or that the bladder of the cuff overlaps itself.
|
|
|
What will happen if the dr. uses a blood pressure cuff that is too large for the child's arm?
|
cause readings that are falsely low
|
|
|
What are the mean systolic and diastolic blood pressure readings for boys and girls?
Systolic (birth, 1 mo., 6 mo., 5 yrs, 8 yrs, 13 yrs, 18yrs.) Diastolic (1 yr., 8 yrs., 11yrs., 18yrs.) |
BOYS
Systolic: Birth- 70 mm Hg 1 month- 85 mm Hg 6 months- 90 mm Hg 5 years- 95 mm Hg 8 years- 100 mm Hg 13 years- 110 mm Hg 18 years- 120 mm Hg Diastolic: 1 year- 55 mm Hg 8 years- 60 mm Hg 11 years- 65 mm Hg 18 years- 70 mm Hg ** girls are about 5 mm Hg lower than boys at all ages** |
|
|
How much lower are girls systolic and diastolic blood pressure readings?
|
about 5 mm Hg lower at all ages
|
|
|
What should the dr. do if the blood pressure reading is elevated?
|
must measure the child's blood pressure in all 4 extremities
|
|
|
What is hypertension?
|
blood pressure greater than the 95% for age and sex determined on 3 different occasions
|
|
|
Do children or adults have a higher incidence of secondary hypertension with elevated blood pressure?
|
children
a cause for the hypertension should be sought |
|
|
What is even more important than the actual position of the child's height or weight on the chart?
|
the pattern of growth
|
|
|
What % of the normal population will fall outside the "normal" range on the growth chart?
|
5%
|
|
|
What is the most common cause of failure to thrive?
|
psychosocial depreviation
|
|
|
What does the growth chart look like in a child who has failure to thrive?
|
the weight decreases first, then the height, and finally head circumference (an ominous sign)
|
|
|
When should the head circumference be measured? How should it be plotted?
|
at every visit from birth until age 3
plotted on a chart according to the child's current age, gestational age, and sex |
|
|
More than 85% of children who have a head circumference more than 2 std. deviations above or below the mean have what?
|
mental retardation or other neurological problems
|
|
|
What should the skin be examined thoroughly for?
|
abnormalities of color, pigmentation, texture, hair distribution, and turgor
|
|
|
What is skin turgor or elasticity a good indicator of?
|
nutrition and hydration
|
|
|
How is skin turgor estimated?
|
by grasping the subcutaneous tissue over the abdominal wall between the thumb and index finger, and then releasing it
|
|
|
What occurs with decreased skin turgor?
|
the skin fails to snap back to its original position
occurs with intravascular volume depletion and poor nutrition |
|
|
On what day in newborn infants does normal "physiologic" jaundice appear? When does it peak? When does it disappear?
|
appears on the 2nd or 3rd day
peaks about the 5th day of life and usually disappears within a week |
|
|
Does jaundice progress from head to toe or from toe to head?
|
head to toe
|
|
|
How does one detect jaundice?
|
apply pressure to the skin and look for yellowing "blanching"
also look at the infant's sclera |
|
|
What is a Mongolian bruise?
|
a type of birthmark which may be confused with a bruise
|
|
|
What disease may café au lait spots be seen in?
|
neurofibromatosis
|
|
|
What may tufts of hair overlying the spine be a sign of?
|
underlying spina bifida occulta
|
|
|
Many infants have distended capillaries at the napes of their necks. What are these called?
|
stork bites
|
|
|
What is the head to body weight proportion at birth?
What is the head to body length proportion at birth? |
1/3 of body weight
1/4 of body length |
|
|
What is an early indicator of motor development in infancy?
|
head control
|
|
|
By what month should the infant be able to steadily hold the head forward in the sitting position?
|

4 mo of age
|
|
|
What is macrocephaly?
|
a head circumference greater than 2 std. deviations above the mean for a child of similar age and sex.
children who plot at greater than the 95th percentile on growth charts are macrocephalic |
|
|
It is important to remember, by definition, ___% of normal children will have head circumferences greater than 95the percentile.
|
5%
|
|
|
If a child has a large head what should you do to make sure they are ok?
|

measure the parents head
they are often inheritied |
|
|
During the first 6 mo. of life, an increase in head size exceeding ____cm/month is abnormal.
|
2 cm/ month
|
|
|
What is the most frequent cause of macrocephaly?
What are some other causes? |
hydrocephalus
subdural hematoma, subdural effusions, intracranial tumor, thickening of the skull, benign familial megalocephaly |
|
|
What can be done in a child under 1 year of age with macrocephaly or suspected effusions?
|
transillumination
|
|
|
What are the steps to performing transillumination of the skull in a child with macrocephaly?
A translucent area greater than ___cm may be abnormal. |
place a flashlight equipped with a narrow, opaque rubber cuff around its glass end firmly against the infant's scalp in a darkened room.
A translucent area greater than 2 cm may be abnormal. |
|
|
What is microcephaly?
|
head circumference measuring more than 2 std deviations below the mean
|
|
|
A head circumference less than the 5th percentile for age and sex is regarded as what?
|
microcephalic
|
|
|
What are some causes of microcephaly?
|
congenital infections, such as cytomegalovirus, toxoplasmosis, or syphilis, trauma, and craniosynostosis
|
|
|
At birth the brain is normally ___% of its adult volume. It is ___% of its adult volume by age 1.
|
25%
75% |
|
|
The bones of the skull are separated by spaces called what?
|
sutures
|
|
|
What are sutures?
|
fibrous septa between cranial bones
|
|
|
When are sutures normally not palpable anymore?
|
after the 6th month of life
|
|
|
When does the final closure of sutures occur?
|
not until early adulthood
|
|
|
Where do the sutures intersect?
|
at the posterior and anterior fontanelles
|
|
|
What does the anterior fontanelle measure at birth?
|
4-6 cm in its largest diameter
|
|
|
When does the anterior fontanelle close?
|
between 4 and 26 months of age
90% close between 7 and 19 months |
|
|
Intracranial pressure is reflected by the condition of what?
|
anterior fontanelle
|
|
|
What kind of pressure is reflected by the condition of the anterior fontanelle?
|
intracranial pressure
|
|
|
What leads to depression of the anterior fontanelle?
|
volume depletion
|
|
|
What causes the anterior fontanelle to bulge?
|
intracranial pressure
|
|
|
Noramlly, is the anterior fontanelle (slightly depressed or slightly bulged?) relative to the frontal and parietal bones.
|
slightly depressed
|
|
|
What happens to the anterior fontanelle with crying?
|
the fontanel bulges, but remains pulsatile
|
|
|
Is a true bulging fontanelle visibly pulsatile?
|
no
|
|
|
What are causes of a bulging fontanelle? (5)
|
hydrocephalus
meningitis subdural hematoma shaken baby tumor |
|
|
When does the posterior fontanelle usually close to palpation?
|
within a few weeks after birth, and should always close by 2 mo of age
|
|
|
What is premature closure of the sutures called? and what does it present as?
|
craniosynostosis and presents as asymmetry of the head or with a decreased in head growth
|
|
|
Because cranial bones in infancy grow predominately at their borders, craniosynostosis can hamper normal enlargement of the head and lead to what?
|
distortions
|
|
|
What is 10-20% of craniosynostosis related to?
|
various syndromes
|
|
|
What is molding? When should it go away by?
|
some overlapping of the skull bone that is commonly present at birth. Normal head shape should be regained by the 1st month of life
|
|
|
What can infants do that may cause them to develop abnormal head shape without craniosynostosis?
|
sleep primarily on their backs
|
|
|
What is caput succedaneum?
|
a diffuse boggy swelling of the scalp brought on by pressure that usually disappears by the first day or two of life. It does cross suture lines.
|
|
|
What is a cephalohemotoma caused by? Does it cross suture lines? When does it usually decreased by>
|
caused by a subperiosteal collection of blood over one or more flat bones of the skull.
The swelling does NOT cross suture lines. Usually decreases by 3 to 6 weeks, but may persist |
|
|
The mastoid air cells do not fully develop until ____ years of age?
|
3
|
|
|
What 2 sinuses are present at birth?
|
maxillary and ethmoid
|
|
|
When are the maxillary and ethmoid sinuses aerated at?
|
6 months
|
|
|
When are the sphenoid sinuses aerated by?
|
3 years
|
|
|
When are the frontal sinuses aerated by?
|
3-7 years
|
|
|
What is a newborns visual acuity?
|
can distinguish between light and dark
estimated visual aquity of 20/400 |
|
|
What will usually indicate that the infant has some vision (in the absent of cortical blindness)?
|
a pupillary light reflex
|
|
|
What is the estimates of visual acuity at one year?
|
20/40- 20/60
|
|
|
By 3 years old what is visual acuity approx. at?
|
20/30
|
|
|
When is macular development complete?
|
not until after 6-7 years of age
|
|
|
20/30 vision by Snellen testing may be considered normal until what age?
|
4 or 5
|
|
|
How does testing for visual acuity differ from an infants to a baby that is 3 months of age?
|
infants- a central and steadily maintained fixation indicates 20/200 or better vision
3 months of age- a baby should fix and follow on objects such as a human face 180 degrees |
|
|
When does a fixation reflex develop?
|
in the first 1 to 2 months of life
|
|
|
How can visual evoked responses be done?
|
by measuring the cortical response to light on the retina
|
|
|
Screening for visual acuity in toddlers can be done using what?
|
standard objects
a dime recognized at 5 feet is consistent with 20/50 vision |
|
|
When should formal vision screening begin at?
|
3 years of age
|
|
|
What 2 things can be used for vision screening at 2 1/2 to 3 yrs of age?
|
Allen picture cards: if these cards are recognized at 20 feet it indicates at least 20/30 vision.
Illiterate Snellen charts, with the E pointing different directions |
|
|
Who should the red reflex be present in?
|
all children
|
|
|
What can the absence of red reflex indicate?
|
ataracts or retinoblastoma
|
|
|
What are the 3 reasons a child may have cataracts?
|
1/3 hereditary
1/3 due to syndromes 1/3 from unknown etiology or due to congenital infections |
|
|
Is the fundoscopic exam more difficult to perform in younger children or an adult?
|
younger children
|
|
|
Bcuz small children are usually slightly myopic, in a examiner with normal vision the retina will come to focus on ophthalmoscopy at ____ TO ____ diopter.
|
-1 to -2
|
|
|
On fundoscopic exam of small children, what is retinal arteries and veins ration?
|
bout the same
|
|
|
On fundoscopic exam, does the AV ratio decrease or increase as the child gets older?
|
decrease
|
|
|
What are retinal hemorrhages in infants and small children almost always a sign of?
What exam is indicated? |
child abuse (shaken baby syndrome)
a complete dilated eye exam is indicated in every case of suspected child abuse |
|
|
How does a newborns pupil at rest differ from that in older children?
|
at rest a newborn's pupil is small and will contract and dilate more slowly
|
|
|
Tears are present at birth, but not in response to emotion until how old?
|
2nd month of life
|
|
|
One third of term babies have what wrong with their eyes?
|
nasolacrimal duct obstruction
|
|
|
What is nasolacrimal duct obstruction caused by?
|
a thin membrane located across the lower end of the tear duct
|
|
|
What is the symptom of nasolacrimal duct obstruction? When does it usually clear by?
|
persistent watering of the eye
usually spontaneously clear in the first few weeks of life |
|
|
In a baby with nasolacrimal duct obstruction, persistent blockage beyond 6 months of life is an indication for what? What is a potential complication?
|
ophthalmology referral
potential complications include persistent conjunctivitis |
|
|
What do Brushfield spots appear as? What are they associated with?
|
a speckled appearance of the iris
associated with Down's syndrome |
|
|
What is hypertelorism?
|
increased distance between the eyes and is associated with many syndromes
|
|
|
Where are epicanthal folds seen at? What are they associated with?
|
seen at the nasal side of the eye
associated with Down's symdrome |
|
|
When may glaucoma be present?
|
at birth or the first several weeks of life
|
|
|
What are symptoms for glaucoma? (3)
|
excessive tearing
photophobia blepharospasm |
|
|
What happens to the cornea in a baby with glaucoma?
|
the cornea increases in diameter and may be cloudy
|
|
|
What happens to the pupil in a baby with glaucoma?
|
it dialates
|
|
|
What may happen to the eye in a baby with glaucoma?
|
may enlarge overall
appears red and irritated and may be confused with conjunctivitis |
|
|
In 50% of glaucoma cases in young infants, what is the first sign?
|
photophobia
|
|
|
When does Strabismus commonly occur? When should it be absent by?
|
occurs in the first few months of life
should be absent by 6 months of age |
|
|
What is the terminology used for Strabismus? (4)
|
eso (turning inward)
exo (turning outward) tropia (obvious, constant deviation) phoria (a latent tendency for eye deviation) |
|
|
Constant eso or exotropia should be referred to ophthalmology is present at ____ months of age.
|
3 months
in general, any strabismus noted after 6 months of age should be referred. |
|
|
What are the 3 types of strabismus?
|
infantile esotropia
accommodative esotropia nonaccommodative esotropia |
|
|
Which type of srabismus almost always required surgery?
|
infantile esotropia
|
|
|
What are some characteristics of infantile esotropia?
|
present at birth
tends to run in families almost always requires surgery |
|
|
What is accommodative esotropia related to?
|
hyperopia
|
|
|
What is nonaccommodative esotropia usually due to?
|
poor vision, trauma, or prematurity
|
|
|
When does accommodative esotropia occur?
|
children who are farsighted compensate by increased accommodation. If the hyperopia is severe enough (+5 or +6 diopters), the eye may not be able to diverge in order to compensate for the convergence. Esotropia then develops that disappears with treatment of the hyperopia.
|
|
|
Name the 2 tests for strabismus?
|
corneal light reflex
alternate cover |
|
|
How in the corneal light reflex test given? What is seen if esotropia is present?
|
by shining a penlight onto the eyes from a distance on 1 meter. The light reflex should occur nearly in the center or slightly to the nasal side of each pupil. Have the child first look at the light, then at a distanct object 20 feet away. If the light reflex is seen laterally on the pupil, esotropia is present.
|
|
|
How is the alternate cover test given?
|
by covering one eye, and seeing if eye movement occurs on removal of the eye cover
|
|
|
What is the most frequent cause of visual loss in children?
|
amblyopia
|
|
|
When does amblyopia occur?
|
normal vision development requires that the visual cortex receive focused images simultaneously from both eyes. If this does not occur the visual image from the dysfunctional eye is suppressed and amblyopia will occur.
|
|
|
What are the causes for amblyopia? (3)
|
strabismus
uncorrecter hyperopia or myopia cataracts |
|
|
At what age does treatment become rarely effective for amblyopia?
|
8 years old
the earlier the treatment the better the outcome |
|
|
Normally, where does the upper edge of the pinna align?
|
normally, the upper edge of the pinna aligns on or above an extension of a line drawn across the inner and outer canthi of the eye.
|
|
|
What do low set ears generally accompany?
|
renal and auditory abnormalities
|
|
|
What does otoscopic examination in the infant require? How about a toddler?
|
infant- that the pinna be pulled gently downward to straighten the ear canal
(the angle of the ear canal changes as children age) toddlers- ear must be pulled either straight back or up and back as in adults |
|
|
When examining a child's tympanic membrane what is essential?
|
proper positioning
the child's head must not be mobile during the exam. If the child might move his head It should be restrained either against the table or against the parent's shoulder. |
|
|
What does pneumatic otoscopy evaluate?
|
the mobility of the tympanic membrane
|
|
|
Besides the pneumatic otoscopy what may also be done in infants over 6 months of age to document tympanic membrane mobility?
|
tympanograms
|
|
|
What is decrease mobility of the tympanic membrane the most sensitive indicator of?
|
an effusion
|
|
|
What may generalized erythema of the tympanic membrane be due to? (2)
|
crying or fever
|
|
|
What does the tympanic membrane show in a small child with suppurative otitis media?
|
increased vascularity and is often bright red
it may be retracted or bulging depending on the degree of pus behind the TM An air fluid level may be present |
|
|
What are 22 complication of otitis media?
|
mastoiditis and hearing loss
|
|
|
What is mastoiditis? Why is it important to detect?
|
an infection in the mastoid bone
important to detect due to the possibility of intracerebral due to direct extension of the infection |
|
|
What is external otitis of the ear characterized by?
What is it usually associated with? What will cause it to have pain? |
inflammation and redness of the ear canal
usually associated with an exposure to excess moisture pressure of movement of the tragus usually causes pain |
|
|
What does the acoustic blink reflex involve? What is a normal response?
|
creating a sudden loud noise (hand clap) about 12 inches from a child's ear
a normal response is blinking |
|
|
What are otoacoustic emissions? How can they be detected?
|
faint sounds produces by the motion of the outer hair cells of the cochlea in response to a clicking noise
can be detected by a microphone sealed in the external auditory canal |
|
|
What do brainstem auditory evoked potentials measure?
|
the action potentials generated from the 8th cranial nerve to the inferior colliculus of the midbrain in response to a click
|
|
|
How is play audiometry done and by who?
|
done by audiologists who introduce different sounds while playing with children and observe the child's response to the sounds
|
|
|
At what age can formal screening of the ear be initiated?
|
in the office at age 4, when child is able to cooperate
|
|
|
What are important red flags to hearing loss?
|
delayed speech development
parental suspicion of decreased hearing |
|
|
What children are at risk for hearing loss? (4)
|
premature infants
children who have had meningitis children with cleft palates those with a family history of deafness ** screen these children early for hearing loss** |
|
|
The patency of the nares should b determined at birth by doing what?
|
occluding one nostril at a time
|
|
|
How long are infants obligate nose breathers for?
|
in the first 1-3 months of life
|
|
|
What is choanal astresia?
|
a bony (90%) or membranous (10%) obstruction that can be either unilateral or bilateral
|
|
|
What does bilateral choanal atresia present with?
|
severe respiratory distress at delivery
|
|
|
In an infant with bilateral choanal atresia, how is the affected infants cyanosis relieved? How is the diagnosis made?
|
relieved by crying (paradoxical cyanosis)
the diagnosis is made by the inability to pass a plastic suction catheter through the nares |
|
|
In children, what may unilateral purulent or bloody nasal secretions indicate?
|
the presence of an intranasal foreign body
|
|
|
A child has foul smelling breath and unilateral purulent. What is the dx?
|
presence of an intranasal foregin body
|
|
|
What does flaring of the nasal alae during breathing usually indicate?
|
respiratory distress
|
|
|
What may nasal flattening in children be associated with?
|
an underlying cleft palate
|
|
|
What are nasal polyps usually due to?
|
recurrent infection
|
|
|
Nasal polyps are unusual in children less then ___ years old EXCEPT in children with what?
|
unusual in less than 10 years old
EXCEPT in children with cystic fibrosis |
|
|
What % of children with cystic fibrosis develop nasal polyps?
|
25%
|
|
|
If a child under 10 years of age who does not have cystic fibrosis is found to have polyps, what test needs to be given? What 2 things is it crucial to rule out?
|
CT
rule out glioma or encephalocele |
|
|
How should the mouth be examined in a younger child?
|

should be adequately restrained and the gag reflex should be assessed only once
Never pinch the nose Ask kids to pant like a puppy :-) |
|
|
How should the mouth of an older child be examined?
|
should be given the opportunity to open their mouths widely without the use of the tongue blade
|
|
|
What 3 things should the teeth be examined for? What should be noted?
|
number
condition position whether or not the child has a normal chronology of tooth eruption |
|
|
At 10 months most children have what teeth?
|
two upper and two lower central incisors
|
|
|
After 10 months, how many teeth are usually added every four month?
|
4 teeth are usually added ever four months (8 teeth at 14 months, 12 teeth at 18 months, 16 teeth at 22 months
|
|
|
At what age does a child have a full set of teeth?
|
age 2 (20 baby teeth)
|
|
|
When do secondary teeth begin erupting?
|
about age 7
|
|
|
What are bottle carries? What are they usually due to?
|
can be severe and usually affect the maxillary incisors.
they are usually due to children being put to bed with a bottle |
|
|
What can prolonged thumb sucking after 5 years of age, or pacifier or bottle use after 18 months potentially alter?
|
can potentially alter the palate shape and affect growth of the mouth, causing malocclusion later in life
|
|
|
What should the posterior pharynx and tonsils be examined for? (3)
|
size
color exudates |
|
|
At what age do tonsils usually enlarge?
|
8 to 10 years of age
|
|
|
How are tonsils usually graded?
|
as 1 to 4 plus
|
|
|
Tonsillar symmetry needs to be observed since asymmetrical tonsils may be due to what?
|
abscess
|
|
|
Is strep throat common in toddlers and infants?
|
no... school aged children
children under 6 do not localize pain to the throat very well |
|
|
Is pain a symptom of tonsillitis in a young child?
|
no, children under 6 do not localize pain to the throat very well, so they may not report pain
|
|
|
Palatal malformations vary widely in what?
|
severity
|
|
|
What fraction of births is cleft palate found in? And what may is be associated with?
|
1/2000 births
may be associated with cleft lip |
|
|
When is the cleft lip usually repaired?
|
3 months of age
|
|
|
When is the cleft palate usually repaired?
|
at 8 months of age
|
|
|
Children with cleft palate are at increased risk of what?
|
recurrent otitis media
|
|
|
What may a bifid uvula indicate?
|
submucous cleft palate
|
|
|
How does the neck of the newborn appear?
|
relatively short
|
|
|
What should the dr. check for when examining the neck? (5)
|
size
anomalies webbing ( a sign of Turner's syndrome enlarged lymph nodes or masses examine the thyroid gland |
|
|
Are pulsations in the jugular venous pulse that are visible when the child is sitting upright always normal or always abnormal?
|
always abnormal
|
|
|
What is a thyroglossal duct cyst? Where is it usually located? What happens when a pt. sticks their tongue out?
|
a round smooth firm swelling 1/4 to 1 1/2 inches in diameter.
usually located in the neck midline between the tongue and suprasternal notch the cyst moves up the neck when the tongue sticks out |
|
|
What are 3 neck abnormalities that may be seen?
|
thyroglossal duct cyst
branchial cleft cysts cystic hydromas |
|
|
Why is bacterial meningitis extremely important to diagnosis early?
|
it has a high risk of mortality and morbidity
|
|
|
Name 2 maneuvers for detecting meningitis that are unreliable in children under 3 years?
|
Bridzinski's sign
Kernig's sign |
|
|
How is Brudzinski's sign performed when checking for meningitis?
What 3 results makes it a positive test? |
it is elicited by flexing the child's neck toward the chest while the child is lying supine.
The sign is positive for meningeal irritation if flexion of the neck simultaneously results in involuntary flexion of the hips and/or knees, resistance to flexion of the neck (stiffness) or neck pain with flexion of the neck. |
|
|
Kernig's sign is positive for meningeal irritation when?
|
when there is an inability to extend the leg because of pain when one hip is flexed
|
|
|
What are the characteristics of the breasts of newborns?
|
they are often enlarged and engorged with white liquid referred to as witch's milk.
|
|
|
Why are the breasts of newborns often enlarged and engorged with white liquid?
|
it is due to the effects of maternal estrogen on the breast tissue which may last for several weeks
|
|
|
The respiratory pattern needs to be inspected.
What is the breathing pattern of an infant? What does this result in? |
diaphragmatic
this results in protrusion of the abdomen during inspiration and retracted of the abdomen during expiration |
|
|
What are 3 signs of respiratory distress?
|
respiratory grunting
intercostal, subcostal and supraclavicular retractions flaring of the nostrils with breathing |
|
|
What do retractions in the chest occur due to?
|
due to increased negative intrathoracic pressure from the forced expansion of the chest cage during labored breathing
|
|
|
Why is it particularly important to inspect the child's breathing pattern with their shirt off?
|
in order to detect retractions
|
|
|
What are the characteristics of an infants chest?
|
they are rounded with the antero-posterior diameter equal to the lateral diameter
|
|
|
By 6 years of age, what is the ration of the transverse diameter of the chest to the AP diameter?
|
3.5:1
|
|
|
How may tactile fremitus be evaluated in the infant?
|
while the baby cries
decreased and increased fremitus have the same implication as in the adult |
|
|
What does percussion of the normal infant chest produce?
|
a hyperresonant note throughout
|
|
|
Lack of hyperresonance in the infant has the same significance as ________ does in the adult
|
dullness
|
|
|
You are my everything!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!
|
I love you so much honey!!!!!!!!!!!!!!!!!!!!!!!
|
|

|
:-)
|
|
|
What is the difference between breath sounds of an infant/ small children and an adult?
|
usually louder and harsher in infants and small children than in adults
|
|
|
What are normal sounds in the lung periphery called?
|
bronchovesicular or bronchial
the type of breath sound present offers little help in the diagnosis of consolidation |
|
|
Crackles and wheezes still occur in infants and have (more, the same, less) significance as they do in adults.
|
the same
|
|
|
How can auscultation in a crying child be timed?
|
with inspiration between cries
|
|
|
What is stridor?
|
a characteristically harsh inspiratory noise created by obstruction of the larynx or extrathoracic trachea.
|
|
|
Stridor in a child with a mild degree of narrowing may only be heard with what?
|
exertion
|
|
|
What is the most common acute cause of stridor?
What is the most common chronic cause? |
acute- laryngotracheaobronchitis (croup)
chronic- laryngomalacia |
|
|
When should the cardiac examination begin with? What 3 things should be noted in addition?
|
inspection, notin visible cardiac impulses or precordial bulging
in addition, note the child's overall growth, color, and any dysmorphic features |
|
|
Congenital heart disease is more common in children with what?
|
syndromes (ex. Down's syndrome)
|
|
|
How is the apical impulse normally palpated?
|
in the fourth intercostal space until age 7, when it moves to the fifth intercostal space
|
|
|
Where is the apical impulse located at age 6 and age 7?
|
6- fourth intercostal space
7- fifth intercostal space |
|
|
The apical impulse lies tot he left of the midclavicular line until age____, at the midclavicular line between ages ____ & ___, and it medial to the midclavicular line by age ____.
|
The apical impulse lies tot he left of the midclavicular line until age_4___, at the midclavicular line between ages __4__ & _6__, and it medial to the midclavicular line by age __7__.
|
|
|
How should auscultation be performed?
|
while the child is both sitting and supine
|
|
|
Are heart sounds in children softer or louder than adults?
|
louder
|
|
|
Which sound is normally louder until adolescence: aortic closure sound or pulmonary closure sound
|
pulmonary closure sound
|
|
|
Is splitting of the S2 normal or abnormal at the cardiac apex in many infants and small children? Why?
|
normal
bcuz the pulmonary closure sound is normally louder than the aortic closure sound until asolescence |
|
|
Why is it particularly important to listen for physiologic splitting of S2 at the base of the heart?
|
its presence rules out many congenital heart diseases
|
|
|
Are murmurs graded differently in children vs adult? If so why?
|
graded the same way
|
|
|
Why is it important to distinguish innocent from pathologic murmurs?
|
innocent murmors occur in the absence of cardiac pathology
|
|
|
What % of children have an innocent murmur sometimes during childhood?
|
over 50% or normal children
|
|
|
Innocent murmurs are never solely diastolic in timing. They tend to change in character with what?
|
changes in position or phase of respiration, and increase during fever, exercise or anemia
|
|
|
What 3 things are innocent murmurs NEVER associated with?
|
cyanosis
hepatomegaly tachypnea |
|
|
Name the 3 most common innocent murmurs.
|
A Still's murmur
venous hum pulmonary ejection murmur |
|
|
What is Still's murmur and who is it common in?
|
very common in children age 3 to 7 years. It is grade II-III, brief in duration, early to mid systolic, and heard maximally at the left sternal border. It is a vibratory murmur that decreases with standing or sitting.
|
|
|
Where can a continuous venous hum be heard? What does this murmurs intensity vary with? What position is it loudest in?
|
can be heard over the upper sternum, clavicle and vessels of the neck in young children.
this murmur's intensity varies with the child's head position and decreases with recumbent position (it is loudest in the upright position) |
|
|
What is a pulmonary ejection murmur and who is it common in? Where is it best heard?
|
commonly heard in adolescents
this is a grade I-II, short early to midsystolic murmur, blowing in quality, best heard at the second and third interspaces of the left sternal border. |
|
|
Many pathologic murmurs are not heard until when? What is this due to?
|
a few days after birth
due to the changing physiology, with the closing of the ductus arteriosis, and the increase in pulmonary blood flow that occurs in the perinatal period |
|
|
When do ductal dependent lesions usually present?
|
in the first day r two of life, when physiologic closure of the patent ductus arteriosis occurs
|
|
|
What 3 things does ductal dependent lesions include? (**In each of these where does the dutus provide blood flow)
|
pulmonary atresia (the ductus was providing blood flow to the pulmonary circulation)
hypoplastic left heart syndrome (the ductus was providing blood flow to the systemic circulation) Pre-ductal coarctation of the aorta (the ductus was providing blood flow to the systemic circulation). |
|
|
Infants may have Pre-ductal coarctation of the aorta, so it important to evaluate what to rule this out?
|
essential to evaluate pulses in the newborn infant , comparing volume and timing between the femoral and brachial pulses
|
|
|
What are murmurs to be particularly concerned about that are potentially pathologic? (5)
|
pansystolic, diastolic, have abnormal S1 or S2 splits, or occur in children with signs of heart failure or abnormal pulses
|
|
|
Non-ductal dependent lesions usually have a delayed presentation. What are 5 examples of this?
|
ventricular septal defects
atrial septal defects aortic valve stenosis pulmonary valve stenosis tetralogy of fallot |
|
|
When are ventricular septal defects usually present at?
|
usually present at 2 to 4 weeks of age, when they are large
|
|
|
Describe the murmurs of a child with ventricular septal defects.
|
harsh, holosystolic murmurs, loudest at the lower left sternal border
|
|
|
In a child with ventricular septal defects, what may they develop signs of?
|
congestive heart failure (lung crackles, hepatomedaly, failure to thrive)
|
|
|
In a child with ventricular septal defects, the drop in pulmonary vascular resistance during the first few weeks of life allows for what?
|
increased left to right flow through the defect, and increased pulmonary congestion.
|
|
|
Atrial septal defects are usually not detected until after _____year(s) of age.
|
1 yr
|
|
|
What do Atrial septal defects present?
|
a mild ejection type murmur at the left upper sterna border
|
|
|
In a child with Atrial septal defects, what is it important to identify since it is often mistaken as innocent?
|
it is important to identify the widely split second sound throughout all phases of respiration, as this murmur is often mistaken as innocent
|
|
|
When may aortic valve stenosis be detected? What does it present with? What does severe stenosis present with?
|
at various ages, depending on the degree of stenosis
There is often an associated ejection click, and the mid systolic murmur typically radiates to the carotids. Severe stenosis present with the same peripheral findings as in adults. |
|
|
When does pulmonary valve stenosis present itself? and what does it present as?
|
present at variable ages
this mid systolic murmur is loudest at the left upper sterna border, and can be distinguished from a pulmonary flow murmur due to the associated ejection click and softening of P2 |
|
|
What is Tetralogy of Fallot?
What does it consist of? (4) |
it is a complex congenital heart defect, consisting of a ventricular septal defect, right ventricular outflow obstruction (usually pulmonary stenosiss). malrotation of the aorta and right ventricular hypertrophy.
|
|
|
What does the typical murmur of Tetralogy of Fallot present as?
|
a mid-peaking systolic ejection murmur at the mid to upper left sterna border
|
|
|
When is a third heart sound often heard? What is this thought to be due to?
|
during early to middle diastole in normal children
thought to be due to the end of rapid filling of the third ventricle |
|
|
If a fourth heart sound in heard, is this considered normal or abnormal?
|
abnormal
|
|
|
What are 4 signs of heart failure in children?
|
hepatomegaly
diaphoresis poor feeding respiratory distress |
|
|
How should the abdomen exam begin?
|
with inspection and auscultation, and then proceed to percussion and palpation
|
|
|
When palpating the abdomen, should you examine the areas of pain first or last?
|
last
|
|
|
How should the stomach be palpated? How bout in a crying pt.?
|
examine the areas of complaint last
it is also helpful to distract the child with conversation, and relax the abdominal musculature by flexing the hip and knees. in a crying pt., palpation is best accomplished at the time the infant inspires following a cry |
|
|
What is prune belly syndrome?
|
involves atonic abdominal musculature. A scaphoid abdomen can occur in newborns with a diaphragmatic hernia
|
|
|
Is "potbelly" contour normal in infants and toddlers?
|
yes
|
|
|
How far below the left coastal margin may the spleen in a normal newborn be palpated?
|
1-2 centimeters
|
|
|
At what age is anything larger than a palpable small spleen tip abnormal?
|
child of any age
|
|
|
What is the normal liver size in the midclavicular line, as estimated by percussion at 6 months, 3 years, 10 years, and for teenagers?
|
5cm at 6 months
7cm at 3 years 8-10cm at 10 years 9-12 cm for teenagers |
|
|
The liver edge is normally palpable ____cm below the right costal margin in the midclavicular line in many children
|
2cm
|
|
|
Can both kidneys be normally palpable in infants and small children?
|
yes
|
|
|
Umbilical hernies are often found in children at what age? what race are they more common in?
|
less than 2 years of age
black children |
|
|
What are umbilical hernias caused by? When do they usually resolve?
|
caused by a defect in the abdominal wall that allows abdominal contents to herniate into the umbilicus
usually resolve by age 5 |
|
|
In children with abdominal pain, when asked where the abdomen hurts where do they almost always point to?
|
the umbilicus
|
|
|
If the child points to abdominal pain anywhere else other then the umbilicus, what is there a high likelihood of?
|
significant pathology
|
|
|
What is the reliability for rebound tenderness in small children?
|
limited reliability
|
|
|
What should inspection of the musculoskeletal in children include?
|
a general screening exam of spontaneous movement, posture, gait, station, and stance. Then focus on areas at risk for the child's age
|
|
|
What should the posterior back of the musculoskeletal be examined for? (5)
|
tufts of hair
dimples discolorations cysts masses that may indicate an underlying spina bifida |
|
|
What is the name for lateral curvature of the spine?
|
scoliosis
|
|
|
How can scoliosis be detected? What is the steps?
|
by asking the child to bend forward and marking the spinous processes with a felt-tip pen
From behind, watch for asymmetries of the scapulas, rib cage and hips, as the child slowly stands erect Then look for a curve in the line of ink dots. |
|
|
What musculoskeletal test should be done at check-ups from age 6-7 through puberty?
|
forward bending test
|
|
|
When does scoliosis rapidly worsen?
|
during a child's growth spurt
|
|
|
How can scoliosis be quantified?
|
on X-ray
|
|
|
What is recommended at 20 degrees and at 40 degrees in a child with scoliosis?
|
20 degrees- bracing
40 degrees- surgery |
|
|
What should the hips of all children be evaluated for? When should they be checked?
|
congenital hip dislocation
during every well visit until the child is walking normally |
|
|
What gender is hip dislocation more common in?
|
first born girls, particularly following a traumatic birth
|
|
|
The hips are examined with what test? How is this test performed?
|
Barlow's test
flex the hips and knees at 90 degrees. Gently adduct hips with gentle pressure applied to the lesser trochanter by the thumb. A palpable clunk is posterior dislocation. |
|
|
What is Ortalani's test?
|
attempts to return an already dislocated hip into the acetabulum by abducting the hips
|
|
|
What is a positive test present when the hips are examined for dislocation?
|
a palpable clunk
|
|
|
Clicking in the hips occurs in what % of newborns and is not diagnostic.
|
8-10%
|
|
|
How may unilateral hip dislocation affect skin folds?
|
may cause the skin folds of the thighs and buttocks to be asymmetrical, with the affected side elevated
|
|
|
When do the femoral head ossify? How bout those in a infant with congenital hip dislocation?
|
3-6 months of age
even later in infants with congenital hip dis. |
|
|
What is used for evaluation for congenital hip dislocation in children less than 4 months of age?
|
ultrasound
|
|
|
The treatment of congenital hip dislocation varies by the age when it is detected.
Under 6 months? Children 6-18 months? Over 18 months? |
Under 6 months- treated with a Pavlik hardness
Children 6-18 months- placed in a spica cast Over 18 months- surgery is usually required **the risk of permanent disability increases with later detection** |
|
|
What are 5 deformities of the lower extremities that are common in infants and small children?
|
Genu varum
Blount's disease Genu Valgum Tibial torsion Metatatsus adductus |
|
|
Genu Varum:
What age group is it common in? What does it cause? How does it resolve? |
(bow legs) is common in 1 to 3 year old children. It causes an increased distance between the knees. X-rays will show symmetric bowing of the femur and tibia. This resolves with growth. Casting, bracing, shoes and surgery are not indicated.
|
|
|
What is Blount's disease?
How may it be detected? How is it treated? |
is a growth disturbance of the medial tibial epiphysis that may be confused with genu varum. The proximal tibia develops an angular deformity. Blount's disease may be detected on X-ray, which reveals abnormal fragmentation of the medial epiphysis of the tibia. Treated with surgery or bracing. If genu varum is asymmetrical, or abnormally severe, consider Blount's disease in you differential.
|
|
|
What is Genu Valgum? What age group are they common in? What does it cause?
|
(knock knees) are common n 3-5 year olds. It causes increased distance between feet when the knees are touching. It is self correcting?
|
|
|
What is tibial torsion? What age is this seen in? At what age does it usually correct itself by?
|
most common cause of in-toeing. This is nonpathologic, and seen in children under age 5. It is a rotational deformity caused by in utero molding. The hips and knees are normally aligned, but the lower leg and feet rotate inward. Prominent in toeing and frequent tripping are seen. Tibial torsion usually correct itself by age 2.
|
|
|
What is metatarsus adductus? When does it self- resolve by>
|
adduction of the forefoot without inversion. This positional deformity should be able to be correct to the neutral position. It self-resolves by age 1 or 2.
|
|
|
What should you be careful to distinguish metatarsus adductus from?
|
clubfoot, or talipes equinovarus
|
|
|
What is clubfoot, or talipes equinovarus?
|
a true foot deformity that cannot bee returned to the neutral position through manipulation
|
|
|
How should children be dressed during the genitalia and anus exam?
|
should be allowed to keep their underwear on
|
|
|
When examining the genitalia in males, what should be verified?
|
that both testes have descended into the scrotal sac
|
|
|
In about what % of male neonates will one or two testes not be palpable in the inguinal canal or scrotum? How about in premature male infants?
When will most of these testicles descend? Surgical correction is usually done from ____to ___ months of life in order to decrease the risk of future infertility and cancer |
3%
premature- 33% most of these testicles will descend in the first few months of life |
|
|
Many male infants have retractile testes in the inguinal canal. How can you get them to descend?
|
when placed in warm, comfortable environment like the bathtub!
|
|
|
The foreskin is not retractable at birth. Approx 90% will be retractable by age ____. Circumcision for phimosis is usually not done until age ___ to ___
|
The foreskin is not retractable at birth. Approx 90% will be retractable by age __3__. Circumcision for phimosis is usually not done until age _7__ to _10__
|
|
|
What is ambiguous genitalia of the newborn considered?
|
a medical emergency die to far reaching emotional consequences for the family when informed of the wrong sex of their newborn infant.
|
|
|
Ambiguous genitalia, if due to congenital adrenal hyperplasia may cause what?
|
severe electrolyte disorders that may affect the viability of the child.
|
|
|
What should be checked in ambiguous babies to rule out potentially life-threatening abnormalities?
|
serum eleectrolytes
|
|
|
Do males or females more often present with abnormal genitalia?
|
females
|
|
|
Why are male infants at higher risk for SIDS?
|
they do not develop ambiguous genitalia and thus their hyperkalemia is not detected as often
|
|
|
What fraction of newborns present with hypospadias?
What is it important to note? Why should you not circumcise these babies? |
1/250
note the location of the urethral meatus Do not circumcise, as the foreskin is used for repair at approx. 1 year of age. |
|
|
Hydroceles are hernias are very common in newborn (males or females?)
|
males
|
|
|
If there is fluid in the scrotum, ______ is present
|
a hydrocele
|
|
|
If there is bowel in the scrotum, a ________ is present,
|
hernia
|
|
|
How are hydroceles characterized? They will usually resorb without surgery by age___?
|
may fluctuate in size and transilluminate
They will usually resorb without surgery by age 18 months. |
|
|
Why are hernias always repaired when detected?
|
due to the risk of bowel incarceration
|
|
|
What is imperforate hymen? What will it present as?
|
a thin white transparent hymenal membrane that blocks the vaginal outlet. It can be difficult to see. If there is vaginal bleeding it will present as a dark red bulge. This is a cause for delayed onset of menses.
|
|
|
Labia minor adhesions are common in who? What are they caused by?
|
common in prepubertal girls. They are caused by fusion of the labia minora from inflammation of the this vaginal mucosa that adheres in midline. Most lyse spontaneously.
|
|
|
In children (esp. infants) a large part of the neurologic examination is obtained by careful observation of what?
|
how the infant react to the environment
|
|
|
What are all assessed in the neurologic examination? (8)
|
positioning
degree of alertness spontaneous movements symmetry of movement eye position and movements cry and primitive reflexes Deep tendon reflexes Muscle tone and bulk |
|
|
What may increased or decreased muscle tone indicate?
|
neurologic disease
|
|
|
How should deep tendon reflexes be elicited?
|
by tapping the biceps and patellar tendons
|
|
|
How should the neurological examination be given in normal full-term newborns?
|
lie in a symmetrical position with the limbs semi-flexed and the legs partially abducted at the hip.
The head is slightly flexed and positioned in the midline or turned to one side. Deviations from this position should be investigated. |
|
|
What are extremely important in picking up potential neurologic disease?
|
developmental milestones
|
|
|
It can be helpful to think of a child's development is broad categories. What are they (4)?
|
gross motor
fine motor speech social skills |
|
|
What is a useful test when examining developmental milestones?
|
Denver Developmental Screening Test
|
|
|
What is the Denver Developmental Screening Test?
|
provides a range of ages for expected developmental milestones. This is a highly specific screening test but not very sensitive. This means that many children with mild development delay may test as normal.
|
|
|
A developmental quotient is one normative measure of development. It is equal to the ratio of what?
|
the child's developmental age over their chronologic age x 100
|
|
|
There should be no head lag by ____ months of age.
|
4
|
|
|
At __to __ an infant should be able to reach and grasp objects.
|
5 to 6
|
|
|
By ___ months an infant should be transferring objects from hand to hand.
|
7
|
|
|
By ____ months the infant should be sitting alone.
|
7
|
|
|
By ___ months an infant should be walking.
|
14
|
|
|
Speech development is extremely important to monitor. Mama and Dada should be present by ____ months of age. A specific word (ball, dog) should be present by ____months. Children should be speaking in two to three word sentences by age ___.
|
Speech development is extremely important to monitor. Mama and Dada should be present by __9__ months of age. A specific word (ball, dog) should be present by __15__months. Children should be speaking in two to three word sentences by age __2 yrs_.
|
|
|
A variety of primitive reflexes may be elicited in the newborn and infant. These reflexes result from a lack of what?
|
lack or cortical inhibition on primitive reflexes by a nervous system that is not yet fully develop.
|
|
|
What is the Babinski reflex characterized by? At what ages may this be normally present?
|
by an upgoing toe in response to noxious stimulation of the S1 dermatome, may be normally present in infants and small children until 3 to 4 years of age.
|
|
|
How is the Moro reflex elicited? How is it characterized? When it is present? When should it disappear?
|
elicited by startling the pt.
is characterized by extension of the arms, following a flexion, clenching of the hands and flexion off the knees and hips. The infant then gives a loud cry. This reflex is present at birth and disappears normally ny about 4-5 months of age. |
|
|
A full term infant should ______ an object when placed in the palm of their hand. _______ is another reflex present at birth.
|
A full term infant should _grasp_____ an object when placed in the palm of their hand. _Sucking______ is another reflex present at birth.
|
|
|
The tonic neck reflex present between what ages? When does it disappear? What is tonic neck reflex describes as?
|
2 weeks and 2 months of age
disappears by 4 to 6 months when the infant's head turns to one side, the ipsilateral arm extends and the contralateral arm flexes |
|
|
What are indicators of neuromotor retardation? These may be the earliest clinical signs of cerebral palsy, neurologic problems or mental retardation.
|
failure to achieve head control by 4 months of age, or the persistence of the tonic neck reflex by 6 months of age
|
|
|
When is handedness decided?
|
decided developmentally around 15 months of age.
|
|
|
What does a definite handedness in children younger than 15 months suggests what?
|
hemiparesis
|
|
|
When is a cerebral thumb sign present? What disease is this a sign of?
|
when the infant holds the thumb in the palm curled under flexed fingers. This is a sign of upper motor neuron disease.
|
|

|
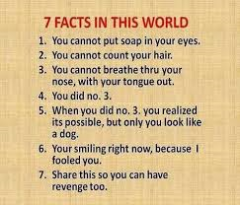
|
|
|
You are so wonderful!!!!!!!
|
You are going to do great!!!!! Better than great!!!!!! You are going to do phenomenal!!!!!!!!!!!!!!
|

