![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
Abdominal pain - types
|
•Visceral
•Somatic (parietal) •Referred •Shifting pain |
|
|
Visceral pain
|
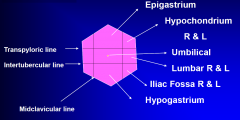
•elicited by distension, inflammation or ischaemia
•intestines / associated organs developed as midline structures therefore visceral pain tends to be midline •transmitted via sensory fibres of the ANS (mainly sympathetic, but distal colon and rectum and bladder are parasympathetic) •centrally perceived sensation is generally slow in onset, dull poorly localised and protracted •embryologically the gut has a segmental origin, so that division into foregut, midgut and hindgut exactly correlates with the vascular supply and correspondingly pain is felt in the epigastrium, umbilical area and hypogastrium |
|
|
Parietal pain
|
•the parietal peritoneum is innervated by somatic nerves
•pain is therefore accurately localised to the site of irritation of the abdominal wall and is accompanied by a reflex contraction of the abdominal wall muscles |
|
|
Referred visceral pain
|
•sensation perceived at a site distant from the primary stimulus
•due to the confluence of afferent nerve fibres from widely different areas within the posterior horn of the spinal cord |
|
|
Shifting pain (radiation)
|
•parallels the course of the underlying condition
•site of pain at onset (visceral) later shifts with progression of eg inflammation as the parietal peritoneum becomes involved (appendicitis) |
|
|
Upper abdominal pain
|
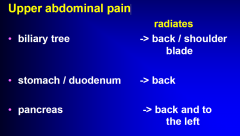
|
|
|
Central abdominal pain
|
•small bowel
•caecum •midline retroperitoneal structures (aorta) |
|
|
Lumbar
|
•Kidneys - radiate to the groin / loin
|
|
|
Lower abdominal pain
|
•appendix (central -> RIF)
•caecum •colon •bladder •uterus •ovaries and fallopian tubes (-> inner thigh) |
|
|
Obstructive vs Inflammatory Pain
|
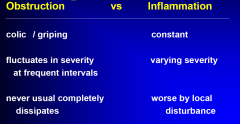
|
|
|
Direct questions relevant to GIT and a history of abdominal pain
|
•appetite,
•weight, •dyspepsia / dysphagia / flatulence / reflux •nausea / vomiting •haematemesis, •bowel habit (constipation / diarrhoea / PR bleeding) •Gynaecological symptoms •Urinary symptoms |
|
|
Examination of the Abdomen
|
•Discolouration
•Scars •Distension •Masses •Bowel signs •Movement •Bruits |
|
|
As part of the examination
Don’t forget……. |
•Hernial orifices
•Rectal examination •Genitalia •Vaginal examination •Femoral pulses •Lymph node drainage |
|
|
Signs of Peritonitis
|
•tenderness - examination causes pain
•guarding - reflex contraction of the abdominal wall muscles •rigidity - localised or generalised increase in the voluntary tone of the abdominal wall •rebound tenderness |
|
|
Investigations (directed!)
|
•FBC
•U&E •LFT •Inflammatory markers •Amylase / Lipase •ABGs •Gp and Hold •Blood Cultures •CEs •Urinalysis •bHCG (NEVER Foreget.. lectures story of discharging a patient and npt checking the bHCG result, turns out the patient had an ectopic) |
|
|
Drugs that can mask Sx in GI
|
•Regular opiate analgesic orders (so only give PRN therefore you can tell if the demand for them is INC, or DEC...)
•Other drugs that may mask the condition eg buscopan |
|
|
Indications for Surgery
|
1. Generalised peritonitis (except pancreatitis)
2. Increasing local tenderness 3. Suspected ischaemia (acidosis, fever, tachycardia) 4. Tense or progressive distension (clinical +/- radiological) 5. Deteriorating clinical signs 6. Pneumoperitoneum |
|
|
Medical Conditions Simulating The Acute Abdomen
|
•Lobar pneumonia and empyema
•Pulmonary Embolus •Acute hepatitis •Diabetic crisis •Porphyrias •Toxins - lead and other heavy metal poisoning •Narcotic withdrawal •Myocardial Infact •Uraemia •Sickle cell crisis •Polyarteritis nodosa •Herpes Zoster •Diseases of the hip and back |
|
|
Physical Findings with various causes of an Acute Abdomen
|
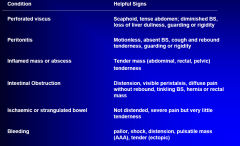
|
|
|
Appendicitis
|
•All ages !
•Diagnosis difficult at the extremes of age •Classic - bizarre presentations •Prodromal symptoms (hours 1-2 days) •Vague central peri-umbilical pain •Shift to RIF •Anorexia •Nausea •(+/- constipation or diarrhoea / dysuria) •Foetor oris •Flushed •Pyrexia •Tachycardic •Tender and guarding RIF •Increased wbc •Doubt consider CT / US •Laparoscopy |
|
|
Biliary Colic
|
•Impaction of a stone in Hartman’s pouch / cystic duct
•FFFF (Fat, Female, Forty, fertile) •Upper abdomen -> back-> shoulder tip •Severe pain - not a true colic, often constant •N&V •Tender and guarded RUQ •US •Mx: Strong analgesics •Interval cholecystectomy |
|
|
Acute Cholecystitis
|
•inflammation of the GB wall due to persistent impaction of a stone
•right hypochondrial pain -> back •persistent •exacerbated by movement •nausea •systemic upset •tender and guarded RUQ •+/- mass •“Boas sign” / Murphy’s sign •Increased wbc •US •Cholecystectomy |
|
|
Bowel Obstruction
4 cardinal S & S SBO vs LBO |
•Vomiting (early SBO)
•Pain (central colic SBO, more ill defined LBO) •Constipation (LBO) •Distension (both) •erect CXR / AXR •wbc •contrast study (gastrograffin enema LBO) •SBO - CT •rehydration •NGT •close observation •LBO - OT •SBO - conservative if improving |
|
|
Pancreatitis
|
•epigastric pain -> back
•severe, constant •relieved by sitting forward •vomiting •alcohol / GS •systemic upset (severity) •jaundice •often generalised tenderness and guarding •Grey Turners / Cullens Sign •Increased wbc •increased amylase / lipase •decreased calcium •abnormal LFTs •CT •Management supportive and conservative |
|
|
Renal Colic
|
•dull loin pain (renal )
•severe loin - groin pain (ureteric) (worse pain they’ve ever had) •haematuria (macroscopic / microscopic) •AXR / IVP / US / CT pyelogram •Analgesia / Hydration |
|
|
Peptic Ulcer Disease
|
•Epigastric discomfort -> back
•Heartburn / Reflux •Relationship to eating (better / worse / time ) Complications: • perforation -> S & S of an acute abdomen UGIB |
|

|
X-ray showing air in around the stomach possible perforation
|
|
|
Diverticulitis
|
•older patient
•LIF ache / pain (left sided appendicitis) •+ / - disruption of bowel habit •nausea •pyrexia •tender and guarding LIF •increased wbc •erect CXR / AXR •abdominal CT •management conservative unless complicated (perforation / abscess / fistula) |
|
|
Abdominal Aortic Aneurysm
|
•aching pain - acute exacerbation
•radiates to back •pulsatile mass •hypotension •obtunded |
|
|
Miscellaneous
|
•Urinary retention
•PID •ectopic pregnancy •ruptured ovarian cyst •torted ovarian cyst |

