![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
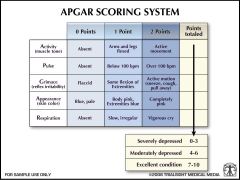
Apgar Scoring
|
|
|
|
What is the significance of the 1 minute and 5 minute Apgar Score?
|
1 minute: need for immediate resuscitation
5 minutes and beyond: probability of susscessful resuscitation. Does NOT predict long-term neurological outcome (is normal in most kids with cerebral palsy) |
|
|
What Apgar Score is predictive of a worse neontal outcome?
|
10 minute score of < or = 3
OR 5 minute score of 0-3 PLUS an umbilical artery pH of < or = 7 significantly increases relative risk of neonatal mortality |
|
|
After how many minutes does the newborn establish regular respirations?
|
by 1 minute of age
|
|
|
Under what circumstances does a neonate require resuscitation?
|
- if there is meconium
- if there is decreased breathing or crying effort - if the infant is not pink - if there is decreased tone - if gestational age is less than term |
|
|
What are the initial steps in neonatal resuscitation?
|
- Place under a radiant warmer
- Suction trachea - Dry - Position head --> suction mouth, then nose - If infant has decreased responsiveness --> provide tactile stimulation - THEN EVALUATE respirations, heart rate, and color |
|
|
Why are newborns prone to heat loss?
|
prone to heat loss due to high surgace area to body mass ratio; if cold stressed will rapidly deplete stores of glycogen and fat
|
|
|
What do you do i thick, particulate meconium is present in a non-vigorous infant?
|
intubate, then suction throuh endotracheal tube
|
|
|
What should you do next if there are decreased (or no) respirations and/or if the HR <100?
|
Perform POSITIVE PRESSURE VENTILATION, with 100% oxygen through bag and mask for 15-30 seconds
|
|
|
What if the infant does not respond after 30 seconds?
|
ENDOTRACHEAL INTUBATION should be performed and ventilation with 100% oxygen continued with a bag through the ETT. if the HR remains <100, continue ventilation
|
|
|
What if the HR is <60 despite effective positive pressure ventilation and 100% oxygen for at least 30 seconds?
|
Initiate chest compressions at 120/minute (compression:ventilation - 3:1)
|
|
|
What should be done if the HR <60 despite effective ventilations and compressions?
|
Give EPINEPHRINE (umbilical vein or ETT) 0.1-0.3 mL/kg of 1:10,000 solution. May repeat q3-5min.
|
|
|
What should you do if there is evidence of significant volume depletion (ie: 2/2 placental abruption)?
|
Give 10-20mL/kg IV of an isotonic crystalloid solution or colloid (albumin, filtered cord blood, or O-negative RBCs, if acute hemorrhage)
|
|
|
What should you do if the infant has respiratory depression and the mother has been given an analgesic drug within 4 hours of delivery?
|
Give 0.1mg/kg of nalaxone hydrochloride either IV or via ETT
|
|
|
What should you do if there is a prolonged resuscitation and metabolic acidosis has been documented
|
Give 2 meq/kg (0.5 mEq/mL of a 4.2% solution) sodium bicarbonate slowly AND ONLY after you have effective ventilation
|
|
|
After resuscitation, if the infant has poor perfusion (weak pulses, low BP, low UOP), what should be done?
|
start a continuous infusion of dopamine or dobutamine at 5-20ug/kg/min along with MIVF. If still no response, consider epinephrine at 0.1-1.0 ug/kg/min (severe shock)
|
|
|
BIRTH INJURIES
What are key diagnostic words for Caput Succedaneum? |
- presenting scalp (most parietal, occipital)
- fluctuant edema (most serous) above periosteum - crosses suture lines |
|
|
BIRTH INJURIES
What is the first diagnostic step in Management of Caput Seccedaneum? |
Reassurance
|
|
|
BIRTH INJURIES
What is the treatment of Caput Seccedaneum? |
If hemorrhagic (less common) and patient is jaundiced, follow bilirubin
|
|
|
BIRTH INJURIES
What is the prognosis of Caput Seccedaneium? |
Resolves completely within days
|
|
|
BIRTH INJURIES
What are key diagnostic words for Cephalohematoma? |
- SUBPERIOSTEAL blood
- usually hard mass - does NOT cross suture line - possible underlying linear skull fracture |
|
|
BIRTH INJURIES
What is the first diagnostic step in cephalohematoma? |
Must follow bilirubin, skull radiographs ONLY IF severe and concern for significant fracture
|
|
|
BIRTH INJURIES
What is the treatment for cephalohematoma? |
May need phototherapy
|
|
|
BIRTH INJURIES
What is the prognosis for cephalohematoma? |
Most resolve in 2 weeks to 3 months; may have calcium deposition for up to 1-5 years
|
|
|
BIRTH INJURIES
What are key diagnostic words for subcutaneous fat necrosis? |
Difficult deliveries and with maternal cocaine use, at sites of trauma --> well defined, hard, irregular lesions of skin; necrosis at 6-10 days of life
|
|
|
BIRTH INJURIES
What are the first diagnostic steps in management of subcutaneous fat necrosis? |
none unless anorexia, vomiting, irritability and increased sleep --> obtain serum calcium
|
|
|
BIRTH INJURIES
What is the treatment for subcutaneous fat necrosis? |
May need to treat significant hypercalcemia with IVF, furosemide, and hydrocortisone
|
|
|
BIRTH INJURIES
What is the prognosis of subcutaneous fat necrosis? |
becomes soft within 2 months then regresses
|
|
|
BIRTH INJURIES
What are the key diagnostic words in skull fracture? |
most linear with cephalohematoma; usually not recognized; depressed - mostly secondary to forceps delivery; palpable indentations
|
|
|
BIRTH INJURIES
What are the first diagnostic steps in management of a skull fracture? |
None unless depressed --> x-ray, possibly CT if suspect underlying brain trauma
|
|
|
BIRTH INJURIES
What is the treatment for neonatal skull fracture? |
usually none, unless large, depressed --> immediate surgery
|
|
|
BIRTH INJURIES
What is the prognosis for neonatal skull fracture? |
most heal within months without problems
|
|
|
BIRTH INJURIES
What are key diagnostic clues for Facial Nerve Paralysis? |
Most with forceps, 1st or 2nd day after birth --> smooth forehead, open eye, no nasolabial fold, corner of mouth droops on ipsilateral side; tongue not affected so feeding is fine
|
|
|
BIRTH INJURIES
What is the prognosis for Facial Nerve Paralysis? |
Most resolve within days to weeks (months is most severe, uncommon)
|
|
|
BIRTH INJURIES
What are key diagnostic clues for Subconjunctival Hemorrhage? |
Red patch in bulbar conjunctiva, common with any delivery
|
|
|
BIRTH INJURIES
What is the prognosis for Subconjunctival Hemorrhage? |
Absorbed in 1-2 weeks
|
|
|
BIRTH INJURIES
What are key diagnostic clues to Clavicular Fracture? |
Most frequent neonatal fx; difficult delivery of shoulder in vertex or extended arms in breech; may not be seen until callus formation at 7-10 days (greenstick); if complete--> at birth with irritability (pain), decreased arm movement, discoloration; deformation at clavicle; no Moro on ipsilateral side
|
|
|
BIRTH INJURIES
What is the first diagnostic step for clavicular fracture? |
plain radiograph
|
|
|
BIRTH INJURIES
What is the treatment for clavicular fracture? |
control pain--> immobilize arm/shoulder
|
|
|
BIRTH INJURIES
What is the prognosis for clavicular fx? |
Bone contour normal after several months
|
|
|
BIRTH INJURIES
What are diagnostic clues to brachial palsy? Erb-Duchenne |
prolonged and dificult delivery; C5-C6 most common; upper arm involved; arm adducted and internally rotated with extension at elvow, pronation of forearm; no reflexes
|
|
|
BIRTH INJURIES
What are diagnostic clues to brachial palsy? Klumpke's Paralysis |
rare; C8-T1 (Horner Syndrome); hand and wrist paralyzed
|
|
|
BIRTH INJURIES
What is the first diagnostic step in management of a Brachial Palsy? |
Plain Radiographs of shulder including lower cervical spine, clavicle and upper humerus to exclude other bone/soft tissue injurys
|
|
|
BIRTH INJURIES
What is the treatment for Brachial Palsy? |
Physical therapy and monthly evaluations; if no correction by 3-9 months --> explore brachial plexus for surgery
|
|
|
BIRTH INJURIES
What is the prognosis for brachial palsy? |
most resolve completely; others may have improvement with early surgery
|
|
|
BIRTH INJURIES
Phrenic Nerve Injury - Key Diagnostic Words - First Diagnostic Step in Management - Treatment - Prognosis |
- Key Diagnostic Words: most unilateral with ipsilateral brachial palsy; hemidiaphragmatic paralysis; lateal hyperextension with stretching of C3, C4, C5; recurrent cyanoss; difficult respirations and no diaphragmatic movement; decreased breath sounds
- First diagnostic step in mgt: plain radiograph --> elevated diaphragm, shift of mediastinum to opposite side and atalectasis bilaterally; best test: real-time ultrasound - Treatment: position with involved side down, oxygen as needed, IV fluids; may need ventilation; if no resolution within 2 months --> surgical plication of diaphragm - prognosis: most recover spontaneously |
|
|
BIRTH INJURIES
Sternocleidomastoid Injury - Key Diagnostic Words - First Diagnostic Step in Management - Treatment - Prognosis |
- Key Diagnostic Words: muscular torticollis; hyperextension in difficult breech or head delivery or in-utero constraint; hematoma --> scarring --> muscle shortening; may see at birth or 10-14 days after birth; head forward to the involved side and chin to opposite shoulder
- First diagnostic step in mgt: plain radiograph studies to exclude other pathology - Treatment: daily stretching, stimulate infant to look in involved direction; place on affected side during sleep; try for 6mo --> if no improvement, then surgery - prognosis: most recover within 2-3 months; if not corrected by 3-4 yrars, skull becomes foreshortened and may have lower cervical and upper throracic scoliosis |
|
|
ROUTINE NEONATAL CARE
|
1) Remove blood and meconium from body with warm water or nonmedicated soap after temperature has stabilized, dry and warm in sterile blankets, Clean perianal area and buttocks with water or mild soap with diaper changes
2) Umbilical cord: one-time appliation of triple dye followed by 2x/d alcohol swab until the cord falls off, or daily bacitracin to the cord 3) Single IM dose of 0.5-1.0mg vitamin K1 oxide within 1 hour of birth to prevent hemorrhagic disease of the newborn 4) Instill either 1% silver nitrate (not adequate for chlamydial infection) or 0.5% erythromycin (or 1% tetracycline) to ppx against ophthalmia neonatorum 5) Data no sufficient for routine recommendation of circumcision. If done, need appropriate anesthesia |
|
|
HIGH RISK INFANTS
- Premature or preterm delivery - LBW - VLBW - IUGR |
- Premature or preterm delivery: <37 wks from 1st day of last menstrual period. A significant cause is in-utero infection leading to chroioamnionitis
- Low Birth Weight (LBW): bw <2500g, results from premature birth, IUGR, SGA. Preterm and IUGR result in significant part of M/M through the first 28 days - VLBW: birth weight <1500g. most are preterm. This is the MOST ACCURATE PREDICTOR of neonatal mortality rate - IUGR: SGA infants have a higher neonatal mortality rate than AGA infants, more prone to fasting hypoglycemia, temperature instability, polycythemia, and perinatal asphyxia |
|
|
HIGH RISK INFANTS
Two types of IUGR |
1) Early-onset or symmetric: decreased cell number, results from problems early in gestation, ie: the first trimester. Weight, length, and HC (ie: brain size) are decreased to relatively same extent.
- Major Causes: chronomosomal , malformation syndromes, teratogenic, infxn. - Main complications: directly relative to underlying cause 2) Late-Onset, asymmetric, or head-sparing: decreased size beinning in the 3T. HC (ie: brain size) is normal, but weight and length are decreased. - Major causes: poor maternal nutrition, placental vascular disease (pre-eclampsia, toxemia), maternal illnesses (chronic HTN, renal disease, anemia). - Compications: related to degree of placental-fetal perfusion and may result in perinatal asphyxia, hypoglycemia, polycythemia-hyperviscosity, or fetal death |
|
|
HIGH RISK INFANTS
- Post-term infants - LGA |
- Post-term Infants: deliver after 42 wks from last menstrual period. May have placental insufficiency leading to hypoxia and meconium staining (more than term). Significant increase in mortality if delivery is delayed >3wks after term. Post-tem, post-mature infants typically have: increased BW, no lanugo, decreased or absent vernix, loose skin, long nails, lots of scalp hair, and white, desquamating skin
- LGA: weigh >90% for GA. Neonatal mortality rates increase at >4000g. most signicant factores are maternal obesity and diabetes; higher incidence of birth injuries, congenital anomalies, and mental/developmental retardation |

