![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
What are the four vascular injury syndromes?
|
ANCA-associated glomerulonephritis
Thrombotic microangiopathy Lupus nephritis Scleroderma |
|
|
What are the two major components in the pathogenesis of vascular disorders?
|
1. Inflammation of blood vessels (seen in vasculitides)
2. Loss of thromboresistance (seen in thrombotic microangiopathies) |
|
|
Two types of renal disease in the setting of vasculitis?
|
Medium vessel disease
Small vessel disease |
|
|
Example of medium vessel disease and disease process.
|
Example = classical polyarteritis nodosa
--> renal infarcts and distal glomerular ischemia --> decline in GFR NOT ASSOCIATED With glomerular inflammation in RBC casts --> ANCA NEGATIVE! |
|
|
Small vessel disease examples and disease process.
|
Microscopic polyangiitis, Wegener's, Churg-Strauss
--> focal necrotizing lesions with crescent formation, active urinary sediment (ANCA+), and rapid progression of kidney failure |
|
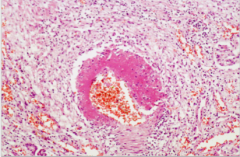
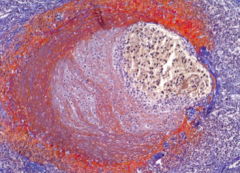
What is shown here?
|
Polyarteritis nodosa (segmental transmural necrotizing vasculitis)
|
|
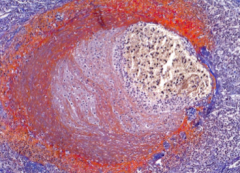
What is shown here?
|
Polyarteritis nodosa in the kidney.
|
|
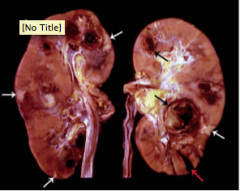
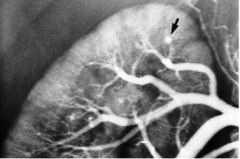
What is shown here?
|
White arrows = renal infarcts
Black arrows = arterial aneurysms Both due to polyarteritis nodosa |
|
|
What is pauci-immune glomerulonephritis?
What is it often associated with? Do ANCA titers always parallel disease activity? |
Negative immunofluorescence studies in the setting of crescentic glomerulonephritis.
ANCAs with extrarenal findings (arthritis, anthralgias, myalgias, fatigue) = NO! |
|
|
Can pauci-immune glomerulonephritis be ANCA negative and without extrarenal findings?
|
Yes!
|
|
|
What are the two distinct patterns of ANCAs?
|
C-ANCA (PR3-ANCA) and P-ANCA (MPO-ANCA)
|
|
|
What type of reactivity does C-ANCA have?
What is it due to? What does positivity strongly suggest? |
Diffuse cytoplasmic reactivity
Antibodies --> cytoplasmic serine protease (proteinase 3) WEGENER'S GRANULOMATOSIS |
|
|
What type of reactivity does P-ANCA have?
What is this due to? In what diseases will it be +? Non-myeloperoxidase P-ANCA has been detected in what diseases? |
Perinuclear only
Antibodies directed at lysosomal myeloperoxidase 30% of patients with anti-GBM, low titers in SLE Sclerosing cholangitis, ulcerative colitis, Crohn's disease |
|

Summary slide
|
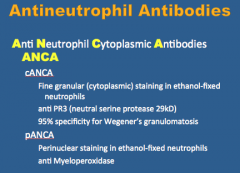
Summary slide
|
|
What is shown in each image?
|
Left = cANCA
Right = pANCA |
|
|
What does binding of ANCAs to neutrophils result in?
What are the adhesion proteins? What cells are the primary target in small vessel vasculitis? |
PMN activation
Increased contact and adhesion with endothelial cells and vascular structures Adhesion = B-2 integrin, mac-1, Fcy Endothelial cells |
|
|
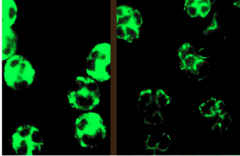
What is the three step pathogenesis of endothelial cell injury by anti-neutrophil cytoplasmic auto-antibodies specifically agianst proteinase 3 (PR3)?
|
1. PMN activation by ANCA
2. Inhibition of PR3-inactivation by ANCA 3. EC activation/lysis by ANCA |
|
|
What does Wegener's granulomatosis lead to?
Symptoms? |
Sinopulmonary renal syndrome
Rhinorrhea, sinusitis, nasopharyngeal mucosal ulcerations Cough, dyspnea, hemoptysis, transient pulmonary infiltrates on chest X-ray 10% azotemia Non specific (fever, weight loss, arthalgias, arthritis, mononeuritis, multiplex, skins lesions may be seen) |
|
|
What is a sensitive and specific test for Wegeners?
|
C-ANCA (PR3-ANCA)
|
|
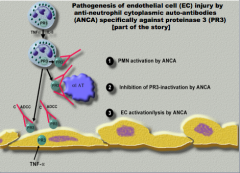
What is shown at each number?
What is the blue haze? |
1-4 = multinucleated giant cells
Blue haze = necrosis Necrotizing granulomatous inflammation of granulomatosis with polyangiits. |
|
What is shown here?
|
|
|
What is shown here?
|
|
|
What is shown here?
|
|
|
|
How do you treat Wegener's?
What is the mortality if untreated? Does relapse occur? |
Cyclophosphamide-based regimens, steroids, plasmapheresis.
80-90% if left untreated 25-50% relapse with 3-5 years follow-up. |
|
|
What are the two broad categories of thrombotic microangiopathies? TMA
|
Hemolytic uremic syndrome
Thrombotic thrombocytopenic purpura |
|
|
What are three symptoms of hemolytic uremic syndrome?
|
1. Hemolytic anemia (schistocytes)
2. Renal dysfunction 3. Thrombocytopenia (due to platelet consumption) |
|
|
What are five symptoms of thrombotic thrombocytopenic purpura?
|
1. Fever
2. Hemolytic anemia 3. Thrombocytopenia 4. Renal dysfunction 5. Neurologic dysfunction (seizures). |
|
|
What is the pathogenesis of thrombotic microangiopathy?
|
Loss of thromboresistance by endothelial cell --> platelet activation --> deposition of platelet and fibrin thrombi in the lumen of affected vessels
Fibrin deposition in subintima and media of vessels --> Onion skin appearance |
|
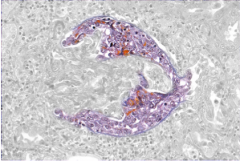
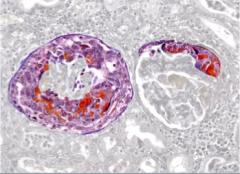
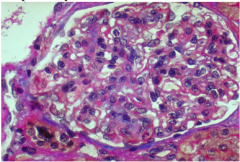
What is shown here?
|
Thrombotic microangiopathy in a glomerulus (thombosed capillary)
|
|
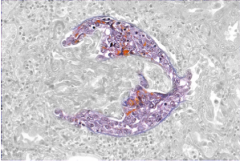
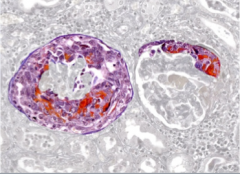
What is this?
|
Thrombotic microangiopathy (thrombosed arteriole)
|
|
|
What are some things that cause endothelial damage?
|
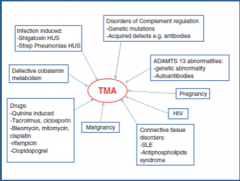
E. coli H7:O157 --> verotoxing --> cytotoxic antiendothelial antibodies
Chemotherapeautic agents (cyclosporine, gemcitabine, bleomycin/cisplatinum) Radiation |
|
|
What could the platelet activation be due to?
|
1. Increased vWF multimers
2. Familial TTP = genetic deficiency of vWF cleaving protease 3. Autoimmune TTP = antibody to vWF cleaving protease develops 4. TTP = occurs in setting of other autoimmune diseases |
|
|
Comment on prothrombin time and partial thromboplastin times in TMA and DIC.
What are TMAs associated with as opposed to DIC? |
TMA = normal times
DIC = prolonged times TMAs = thrombotic diathesis as opposed to bleeding diathesis |
|
What is important here? Diagnosis?
|
??
|
|
|
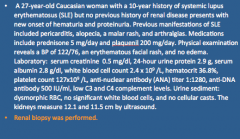
What is a systemic disease sparing no organ system and caused by an aberrant immune response?
Where is the highest prevalence? 10 year survival rate? |
SLE
Brazil 70% |
|
|
Know the lupus criteria again.
|

Malar rash, discoid rash, photosensitivity, oral ulcers, arthritis, serositis, renal disorders, neurologic disorder, hematologic disorder, immunologic disorder, antinuclear antibody
|
|
|
What are the six classes of lupus? Most common? Least common?
|
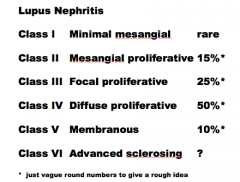
|
|
What is shown here? Is this severe or mild?
|
Lupus nephritis class II
Mesangial proliferative (MILD) |
|
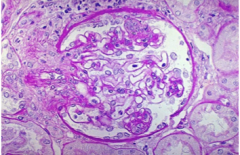
What is shown here? (severity?)
|
Lupus nephritis class III
Focal proliferative Moderate |
|
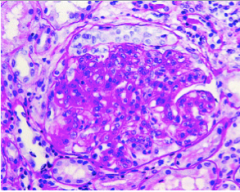
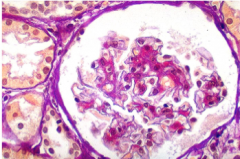
What is shown here?
Severity? |
Lupus nephritis class IV
Diffuse proliferative Notice inflammatory cells, mesangial cells, capillary endothelial cells) SEVERE |
|
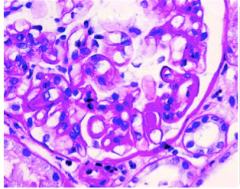
What is shown here? SPECIFICALLY!
|

Lupus nephritis class IV
Diffuse proliferative Wireloop lesions, hyaline thrombus in capillary SEVERE! |
|
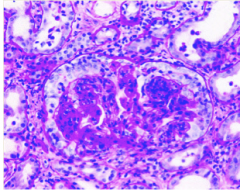
What is shown here?
|
Lupus nephritis class IV
Diffuse proliferative Damaged glomerulus, crescent formation, excess cells of carious types SEVERE! |
|
What is shown here? Quality?
|
Lupus nephritis class V
Membranous NEPHROTIC |
|
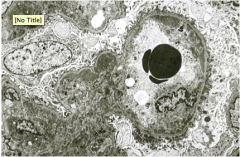
What is shown here?
|
Lupus nephritis EM:
Subendothelial and mesangial deposits |
|
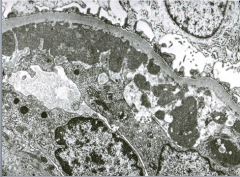
What is shown here?
|
Subendothelial deposits?
|
|

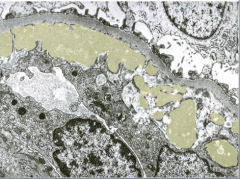
What is shown here?
What is this referred to? |
Immunofluourescence of lupus nephritis
Staining of deposits with antisera to IgG, IgM, IgA, C3, and C4 typically --> FULL HOUSE IMMUNOFLUORESCENCE |
|
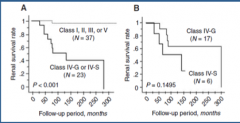
Notice the renal survival rates of the difference classes of SLE?
|
|
|
|
What is the treatment for SLE?
|
1. Aspirin
2. GLUCOCORTICOIDS 3. Immunosuppressants (cyclophosphamide and mycophenolate mofetil) 4. Inhibit toll-like receptor (hydroxychloroquine) 5. Hormone manipulation (dehyroepiandrosterone) 6. Modulation of cell signaling (tacrolimus, sirolimus) |
|
|
What are the only drugs approved by FDA for lupus treatment?
|
Aspirin, glucocorticoids, hydroxychloroquine
|
|
|
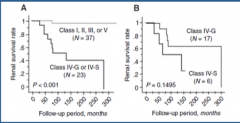
Another term for scleroderma?
Definition? Who is affected? Two types based upon pattern of skin involvement? |
|
|
|
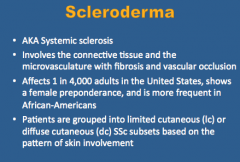
Clinical features of both limited and systemic scleroderma?
|
Simplify this somehow?
|
|
|
Involvement of what organ is frequent in scleroderma? What is scleroderma renal crisis?
How is it treated? |
Mild renal involvement (mild dysfunction, protetinuria, hypertension)
Scl renal crisis --> new onset of accelerated arterial hypertension and/or rapidly progressive oliguric renal failure ACE INHIBITORS --> unusual! |
|
|
What are risk factors for scleroderma?
|
1. early diffuse systemic sclerosis
2. rapidly progressive skin disease 3. anti-RNA polymerase antibodies 4. corticosteroid therapy |
|
|
What occurs in arcuate arteries in scleroderma?
What else is common? What vascular changes do you see associated with a poorer outcome? |
Intimal and medial proliferation with luminal narrowing
Fibrinoid necrosis and thrombosis Mucoid intimal thickening and thrombosis |
|
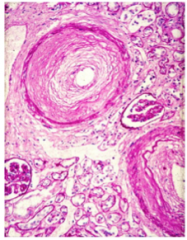
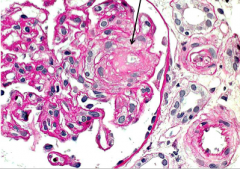
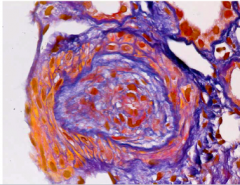
What is shown here?
|
Concentric sclerosing intimal thickening of interlobar arteries 150-500 microns in diameter resembling onion skin.
Systemic Sclerosis (scleroderma) |

