![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
What are the 3 functions of the heart? and there sub-functions?
|
1. Transportation
- respiratory - nutritive - excretory 2. Regulation - hormonal - temperature 3. Protection - clotting - immune |
|
|
what side of the heart is considered pulmonary?
Why? |
right
Because it pumps blood to the lungs |
|
|
what side of the heart is consdiered systemic?
Why? |
left
Because it pumps blood to the body |
|
|
During systole, does blood pressure rise or fall?
|
rises
|
|
|
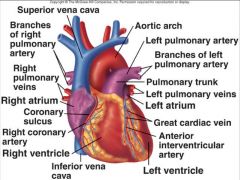
What vessel(s) deliver deoxygenated blood to the heart from the body?
|
superior/inferior vena cava
|
|
|
Blood pressure does what during diastole?
|
falls
|
|
|
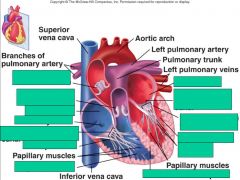
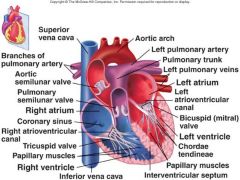
Describe the structures that the blood travels through from the superior and inferior vena cavas to the lungs.
|
Vena cavas ---> right atrium ---> right atrioventricular (tricuspid) valve ---> right ventricle ---> pulmonary semi-lunar valve ---> pulmonary artery ---> lungs
|
|
|
Describe the structures oxygenated blood travels through from the lungs to the body.
|
Lungs ---> pulmonary vein ---> left atrium ---> left AV (bicuspid/mitral) valve ---> left ventricle ---> aortic semi-lunar valve ---> aorta ---> body
|
|
|
When heart rate increases, what happens with all the phases of cardiac cycle?
|
they shorten, especially diastole
|
|
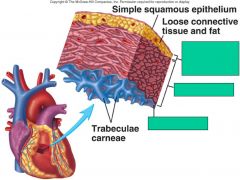
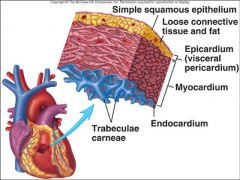
Identify the layers of the heart wall
|
|
|
|
|
|
|
|
|
|
Name/Describe the 2 phases of systole
|
1. Isovolumetric Contraction:
- Blood is not moving in or out of ventricle - All valves are closed - Pressure is building 2. Ejection: - AV valves are closed - Ventricular pressure causes semilunar valves to open - Blood is ejected |
|
|
Name/Describe the 1st phase of diastole
|
Isovolumetric relaxation:
- Semilunar valves close - Ventricles/Atria relaxed - Ventricular/Atrial pressure drops |
|
|
What is Heart Murmur?
|
sounds produced by regurgitation through valves
|
|
|
Name/Describe the 2nd phase of diastole
|
Rapid Filling:
- Ventricular pressure drops below that of the atria - AV valves open - Blood rushes into ventricles |
|
|
Name/Describe 3rd phase of diastole
|
Atrial Contraction (atrial systole):
- Pressure in atria now lower than that of ventricles - Atria contract to deliver the remaining blood - Immediately after atrial contraction, Isovolumetric Relaxation, and hence the cardiac cycle, start all over again. |
|
|
what is the main way that the ventricles are filled?
|
passive ventricular filling during diastole
|
|
|
During diastole:
the chordae tendineae tension is _______ the papillary muscle is ________ the cardiac muscle is _________ the ventricle is _______ the AV valves are ________ and the semilunar valves are |
low
relaxed relaxed dilated open closed |
|
|
What is adjusted by the autonomic nervous system or hormones?
|
heart rate
|
|
|
During systole:
the chordae tendineae tension is _______ the papillary muscle is ________ the cardiac muscle is _________ the ventricle is the AV valves are ________ the semilunar valves are _______ |
high
contracted contracted contracted closed open |
|
|
what are the two ways the AV valves stay closed?
|
the cusp shape causes them to close as blood fills them
the chordae tendineae put tension on them to close them |
|
|
Do the atria and/or ventricles work together or separately?
|
Atria: work as one
Ventricles: work separately from each other |
|
|
The Vagus nerves (X) carries what to small ganglia in cardiac plexus?
|
parasympathetic preganglionic fibers
|
|
|
does the nervous sytem cause the heart to contract?
|
no
|
|
|
Explain the electrical impulse cycle in the SA node
|
1. Pacemaker Potential: Drives the self-generated firing of Pacemaker Cells
Preceding action potential completes ---> cell is hyperpolarized -60mV ---> Na/K channel opens ---> Na comes in fast ---> K goes out slowly ---> slow net depolarization to -40mV threshold 2. Action Potential -40mV causes Ca2+ channels to open ---> Ca2+ influx causes upward phase of action potential ---> at top of action potential (+20mV) K+ channels open ---> repolarization ---> new cycle begins |
|
|
Explain how the spontaneous SA node depolarization can be modulated
|
1. Epinephrine/Norepinephrine:
- Increases cAMP production - cAMP keeps Na+ (HCN) channels open - Faster pacemaker potential 2. Acetylcholine: - Secreted by parasympathetic neurons - Opens K+ channels. - Slows pacemaker potential |
|
|
Describe the path of electrical signals
|
Sinoatrial (SA) node ---> Electrical channels ---> atrioventricular (AV) node ---> Bundle of His ---> Left/Right Bundle Branches ---> Purkinje Fibers (which start at the base and travel up outer walls)
|
|
|
Why is the Pacemaker Potential also called the Diastolic Depolarization
|
Because the pacemaker potential represents the non-contracting time between heart beats (diastole)
|
|
|
Describe the Myocardial Action Potential
|
- Myocardial cell rests at -85mV
- Action potential from SA node brings MC cell to threshold - Voltage gated Na+ channels open, potential shoots straight up (undefined slope) to +15mV - Plateau for 200-300ms due to a balance of Ca influx and K efflux. - More K+ channels open, repolarization occurs. |
|
|
ACh (parasympathetic stimulation) speeds or slows the heart?
|
slows
|
|
|
NE (sympathetic stimulation) does what to the heart?
|
speeds it up
|
|
|
what is the primary ion that causes depolarization in cardiac myocytes?
|
sodium (Na+)
|
|
|
What is the difference between what happens in the SA node and in other cardiac myocytes?
|
The SA node has a faster action potential: sodium causes slight depolorazation until threshold when Ca+ channels open and Ca+ rushes in causing a very fast depolarization.
|
|
|
Membrane potential of pacemaker cells are higher or lower than other cardiac cells?
|
lower
|
|
|
what causes repolarization of cardiac myocytes?
|
potassium leaving the cells
|
|
|
what is the same about skeletal and cardiac muscle?
|
depolarization caused by sodium entering the cell and repolarization caused by potassium leaving the cell
|
|
|
what is different about cardiac muscle cells from skeletal?
|
The plateau phase: the depolarization of the cardiac muscle causes Ca+ channels to open letting Ca+ into the cell (which makes cell go positive) - at the same time, K+ is leaving the cell (which makes cell go negative) - so the movements of these two ions cancel each other out for a time, causing a longer contraction in the cardiac muscle cell.
|
|
|
Increased heart rate (by sympathetic stimulation of SA node) is cause by what hormones?
|
epinephrine (E), norepinephrine (NE), and thyroid hormone
|
|
|
How does the cardiac myocyte repolarize?
|
after plateau phase, the L-type Ca+ channes close while K+ continues leaving, making the cell more negative (repolarization)
|
|
|
describe what the refractory period in cardiac myocytes is and why it is necessary
|
a period of either complete or reduced sensitivity to additional stimulation
Prevents tetanic contraction - allows movement of AP to progress down the heart from the SA node rather than go back up right away. |
|
|
what does the P wave represent?
|
atrial depolarization spreading
|
|
|
what does the QRS complex/wave represent? Immediately after?
|
spread of depolarization into ventricles
immediately after QRS is heart sound 1 "Lub" |
|
|
- what does the S-T segment represent?
- what 2 events does the T wave represent? |
plateau phase of the action potential
ventricle repolarization, heart sound 2 "Dub" |
|
|
which valves are closed during diastole?
|
semilunar valves (bicuspid and tricuspid) - keeps blood that has left the heart from leaking back into the ventricles.
|

